Abstract
Purpose
Spinopelvic fixation and triangular osteosynthesis give firm internal fixation for unstable pelvic ring injuries (UPRI), but with sacrifice of mobility of the lumbar spine. Here, we describe the procedure and outcomes of a new approach, which we refer to as “within ring”-based sacroiliac rod fixation (SIRF).
Methods
The patient was placed in a prone position and longitudinal skin incisions were made at the medial margins of the bilateral posterior superior iliac spines (PSIS). After reduction of fracture, a pedicle screw was inserted into the first sacral vertebra on the injured side and iliac screws inserted through the bilateral PSIS were bridged using rods.
Results
SIRF was performed in 15 patients. The AO/OTA classification was 61-B2.3 in 1, C1.3 in 4, C2.3 in 7, C3.3 in 1, and H-type spinopelvic dissociation in two cases. The mean operative time was 179 (110–298) minutes, mean blood loss was 533 (100–2700) cc. One patient died during hospitalization and three patients stopped outpatient treatment. The other 11 patients achieved bone union without major loss of reduction in a mean post-operative follow-up period of 23.8 (4–50) months. The mean Majeed score at final follow-up was 86.7 (73–96) out of 96, excluding scoring sexual intercourse.
Conclusions
“Within ring”-based SIRF not including the lumbar spine in the fixation range is a simple, safe, and low-invasive internal fixation method for UPRI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinopelvic fixation (SPF) and triangular osteosynthesis (TOS) are firm internal fixation methods for unstable pelvic ring injury (UPRI) [1,2,3,4]. SPF uses spinal instrumentation, with pedicle screws inserted into the fourth and fifth lumbar vertebrae, because the lumbar spine is used as a fixation point, i.e., the ring structure of the pelvis is reconstructed using the lumbar vertebra. In contrast, TOS fixes the lumbar vertebra only on the injured side, i.e., fixation in combination with iliosacral screw placement. Both methods are used for fractures with severe instability [1,2,3,4,5,6], but wound complications and deep infection associated with high soft tissue invasiveness are problematic [2,3,4, 7]. In addition, mobility of the lumbar spine is sacrificed because the L5/S1 facet (the lumbosacral junction) is firmly fixed [8,9,10,11] and development of adjacent segment disease is of concern [12,13,14]. Thus, implant removal is a premise of SPF and TOS [4, 9, 10].
We have devised a surgical procedure referred to as sacroiliac rod fixation (SIRF) as a new internal fixation method that overcomes the invasiveness and problems of the fixation range of SPF and TOS. In SIRF, the pedicle screw inserted into the first sacral vertebra (S1) on the injured side is connected to bilateral iliac screws with rods. The absence of fixation of the L5/S1 facet (“within ring” concept) allows conservation of mobility of the lumbar spine and resolves the concern for adjacent segment disease. Since a screw is inserted into the sacrum, which is the injured region, fracture can be directly fixed compared with fixation by TOS and SPF, and a long screw inserted directly under the end plate of S1 and advanced close to the promontory of the sacrum plays the role of an anchor against vertical displacement of the hemipelvis. In addition, rods connecting the bilateral iliac screws may exert strong resistance against horizontal and rotational displacements. The objective of this study was to explain the surgical procedure of SIRF and present clinical outcomes.
Materials and methods
Materials
Titanium alloy-based spinal instrumentation (USS II Ilio-Sacral, Modular System for Stable Fixation in the Sacrum and Ilium, DePuy Synthes Co., Zuchwil, Switzerland) was used. The sizes of S1 pedicle screws and iliac screws (all USS II dual-core cancellous polyaxial screws) inserted into the ilium were outer diameter 6.2–8.0 mm and length 30–80 mm (length 65 mm only in a screw with an outer diameter of 6.2 mm). The screws had inner diameters corresponding to cancellous and cortical bone, which increases pull-out strength. Rod-bridging screws have two diameters (5.0 and 6.0 mm) and the instrument is equipped with a polyaxial 3-D head, sleeve, and nuts to connect the rod and screw, enabling the side loading polyaxial screw system, i.e., a combination of the screw head and sleeve retains the rod as if it is wrapped, so that the force loaded on the nut is reduced, resulting in firm construction. In addition, the rod can be easily set because the head has ±25°circumferential mobility. A T-connector was used to bridge bilateral iliac screws to the S1 pedicle screw on the injured side (or bilateral sides) with rods. By joining the two rods using the T-connector, the rods were arranged in a T-shape.
Installation
Setting the patient in a prone position is the first important step in SIRF. The procedure is performed on a radiolucent operating table giving access for the C-arm fluoroscopic unit under the table for anteroposterior, lateral, inlet, and outlet projections. It is confirmed that the pelvis is not inclined under fluoroscopy before surgery, in which the pelvis on the non-injured side (ala of the ilium and obturator foramen) is the anteroposterior view. Median arrangement of the spinous process of the lumbar vertebra is also important. The location of the spinous process helps to judge whether the insertion angle of the S1 pedicle screw is appropriate. To apply SIRF effectively, the lateral view is important, and clear and extensive visualization of the lumbar spine over the pelvis is required. The important features of fluoroscopic images in SIRF are described in detail below. The surgical field was extensively disinfected and the lower limb on the affected side was also disinfected and draped to prepare for manual or direct traction during surgery.
Approach
Skin incisions of about 5 cm were made along the medial margin of the bilateral posterior superior iliac spines (PSIS) (Fig. 1a). To secure a working space to insert the S1 pedicle screw, a 3–4 cm skin incision was added at a proximal site on the injured side. The aponeurotic origins of the latissimus dorsi and thoracolumbar fascia were incised together, and PSIS was exposed under the periosteum. The gluteus maximus muscle on the lateral side and the iliocostalis lumborum and multifidus on the medial side were detached from the bone to expose PSIS entirely. The multifidus was detached from the lateral toward the median or proximal side of the sacrum, depending on the need to expose the fracture and S1 pedicle screw insertion region.
Incisions of about 5-cm were made along the medial margins of the bilateral PSIS (black lines). The incision was extended toward the proximal side as needed (a). Lowering of the Schanz pin inserted into the ipsilateral iliac crest and iliac screws, and setting the fulcrum at the Schanz pin inserted in the L5 pedicle toward the vertebral body reduces vertical displacement (b). To retain the reduced position, the Schanz pin inserted into the contralateral ilium and lowered Schanz pin on the injured side were connected and fixed by external fixation (c). If the S1 pedicle and iliac screws are close together, bridging with the rod using the T-connector is difficult (d)
Reduction and fixation
It is desirable to reduce displacement toward the cranial side and rotational displacement of the hemipelvis on the injured side as much as possible before surgery. We insert Kirschner wire with a diameter of 2.0 mm into the femur on the affected side and apply 10 kg direct traction to reduce displacement before surgery. If reduction of rotational displacement was required, this was performed to the extent possible when external fixation was attached. When the fracture was displaced into the sacral neuropore on axial CT, it was reduced while carefully observing symptoms. Regarding intra-operative reduction, we mainly attempt reduction of vertical displacement, in which a Schanz pin with a diameter of 5 mm is inserted into the iliac crest and reduction is applied by operating a joystick, in addition to direct traction of vertical displacement of the affected limb. Vertical displacement was also reduced by expanding the surgical field toward the proximal side and lowering the Schanz pin and iliac screw inserted into the ipsilateral iliac crest, setting the fulcrum at the Schanz pin inserted into the L5 pedicle. Once a reduced position was acquired, internal fixation was applied. To ensure retention of the reduced position, an external fixator was often used during surgery (Fig. 1b).
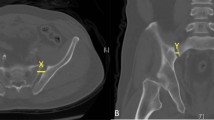
First, the pedicle screw was inserted into S1 because if the iliac screw on the injured side is inserted first, the positions of the S1 pedicle screw and iliac screw heads may be too close to each other, which interferes with bridging with rods (Fig. 1c). The S1 pedicle screw entry point was lateral and slightly distal to the L5/S1 facet, and was prepared using an awl. The direction of the awl was set with reference to the angle of the pedicle against the midline in an axial CT image acquired before surgery. Then, a probe was inserted in the appropriate direction through the entry point. Advancing the probe in a too lateral direction results in insertion of a short screw or perforation of the cortical bone and deviation from the vertebra, whereas a too medial direction results in perforation of the spinal canal. Thus, the probe was advanced in an appropriate direction for a sufficient distance using the feel of the hand and the fluoroscopic image. Since the S1 pedicle screw insertion was targeted directly under the end plate and was advanced close to the promontory of the sacrum (Fig. 2a), a probe with a curved tip was used. When the probe passed through the pedicle, the tip was turned medially and advanced until resistance was felt. At this point, when the probe tip passes over an extension line connecting the spinous processes of lumbar vertebrae in the anteroposterior view of fluoroscopy, it has to be handled carefully because it may have advanced too medially and perforated the spinal canal (Fig. 2b). It was then confirmed that the screw insertion route was safely secured using a pedicle sounder. We use a screw with a 7-mm diameter for the S1 pedicle screw, and finally confirm that the screw tip did not pass over the midline in the fluoroscopy anteroposterior view and that the screw was advanced along the end plate directly under it, close to the promontory in the lateral view. Since the bone shape of PSIS protrudes medially, the bone was resected as needed when it was difficult to set the S1 pedicle screw insertion angle toward the medial side. When the fracture type was AO/OTA classification 61-C3, S1 pedicle screws were inserted bilaterally.
An axial CT image (a) and 3D-CT (b): The S1 pedicle screw was inserted directly under the end plate and advanced close to the promontory of the sacrum. An anteroposterior ragiograph (c): S1 pedicle screws were inserted bilaterally in AO/OTA class 61-C3.3 fractures. An axial CT image (d): Since the direction of the right S1 pedicle screw was too medial, the screw deviated into the spinal canal. The patient complained of numbness of the S1 region after surgery. Implant removal was scheduled soon after bone union
Since the iliac screw entry point was at a site as distant from the S1 pedicle screw as possible due to the reason described above, the distal half of the PSIS bone was resected using a chisel or Luer (Fig. 3). To prevent skin irritation by the iliac screw head, a sufficient amount of bone was resected from PSIS, which enabled adjustment to nearly the same depth as that of the S1 pedicle screw and simple bridging with rods between the iliac screws in the transverse direction and bridging the S1 pedicle screw on the injured side in the longitudinal direction. The screw insertion process was the same as that for the S1 pedicle screw. Attention should also be paid to the direction of iliac screw insertion. The iliac screws were carefully inserted with reference to the slope of the external plate, so that they did not penetrate the inner plate of the ilium. They were advanced laterally in the fluoroscopy anteroposterior view and passed above the greater sciatic notch in the fluoroscopy lateral view, with care not to penetrate the hip joint (Fig. 4). We use a screw with an 8-mm diameter and 80-mm length for all patients. For the reasons described above, the iliac screws were inserted to a sufficient depth and the S1 pedicle screw was inserted so as to be present on the same plane. The iliac screw on the non-injured side was inserted symmetrically to the already inserted iliac screw using the same procedure.
Rods of 6-mm diameter were selected and set as follows. First, a short rod in the longitudinal direction was passed through the S1 pedicle screw head. Then, a long rod in the transverse direction, which was passed through the T-connector beforehand, was passed through the heads of the bilateral iliac screws, and the distal end of the short rod in the longitudinal direction was fitted in the T-connector, by which the screws were bridged by the rods (Fig. 5a). Finally, the connection between the S1 pedicle and iliac screws was tightened at a 12-Nm torque. The connection between the T-connector and rods was tightened using a manual lock. Bridging the screws with the rods was smoothly applied using the side loading polyaxial screw system and by bending the rod. It is important to pay attention to the screw insertion sites on the injured side so that the implants are not crowded (Fig. 1c). When rods could not be set using the T-connector, the S1 pedicle and iliac screws were bridged only by bending the rods (Fig. 5b). For S1 pedicle screws inserted on the bilateral sides, the rods were basically set using the same procedure.
An anteroposterior ragiograph (a): SIRF construct with unilateral S1 pedicle screw insertion. An simulated pelvis (b): Connection between the screws was achieved using the T-shaped connector. An anteroposterior ragiograph (c): When the rod could not be set using the T-connector, the S1 pedicle and iliac screws were bridged with only one rod. In this case, the heads of the pedicle and iliac screws were aligned on almost the same horizontal line
Patients
Of 31 patients with pelvic ring fracture treated with internal fixation at our hospital between January 2012 and December 2016, 15 received SIRF (Table 1). The mean age was 49.5 years old (20–83 years old), and ten and five patients were male and female, respectively. The cause of injury was fall in seven patients, traffic accident in five, and compression by a heavy item in three. The mean injury severity score was 16.9. The fracture type was AO/OTA class 61-B2.3 in one patient, C1.3 in four, C2.3 in seven, C3.3 in one, and H-type spinopelvic dissociation in two.
Clinical results
The mean operative time was 179 minutes (range 110–298 min), the mean blood loss was 533 cm3 (100–2700 cm3), seven patients (46.7%) required blood transfusion, and the mean volume of blood transfusion was 600 cm3 of RCC (280–1400 cm3). One patient who required 1400 cm3 of RCC also required 720 cm3 of FFP during surgery. One patient died during the hospital stay and three patients stopped visiting the outpatient clinic. Excluding these patients, the clinical course was surveyed in 11 patients. The mean follow-up period was 23. 8 months (4–50 months), and bone union was achieved in all patients. No marked loss of the reduced position occurred after surgery. No wound complication requiring reoperation developed, but deep infection occurred in one patient and was treated with lavage and debridement. Implant removal was performed within one year after surgery in three patients, due to implant irritation in two patients and by request for one patient. The Majeed pelvic score is a patient-reported outcome evaluating five areas: pain (30 points), work (20 points), sitting (10 points), sexual intercourse (4 points), and standing (36 points). The mean Majeed score at final follow-up was 86.7 (range 73–96) out of 96, excluding scoring sexual intercourse.
Discussion
The procedure to reduce vertical displacement during surgery with SIRF is the same as those in SPF and TOS. Loading a distraction force on the injured-side hemipelvis while setting the fulcrum at L5 may be useful to reduce vertical displacement. However, we do not use the screw inserted into L5 as a fixation point based on the “within ring” concept, and we always remove the screw during surgery. In 40 patients treated with TOS, Sagi et al. [4] found lumbago and accompanying limitation of lumbar spinal mobility in 95% of cases and coronal tilt (scoliosis) of the L5/S1 segment in 13%, but when the implant was extracted, lumbago and scoliosis improved in 100% and limitation of lumbar spinal mobility improved in 90% of cases. Keel et al. [9] and Mouhsine et al. [10] also stated that it is desirable to extract the implant, given the cost of crossing the L5/S1 motion segment, and we agree with this suggestion. Based on these considerations, we consider that SIRF is markedly more beneficial than TOS and SPF. SIRF is simple and safe, but it is important to pay attention to the insertion direction and length of the S1 pedicle screw on the injured side, and screws have to be used with avoidance of closely positioned screw heads. In our opinion, the indication of SIRF may be AO classification 61-C1.3. When fixation of the anterior element is added, the indication may be expanded to AO classification 61-C2.3 and C3.3.
A previous report of the lumbopelvic stabilization showed that secondary surgery due to the unexpected complications underwent in eight patients (42%) and the implants in all the cases were removed. The causes were implant irritation (11%), skin ulcer (5%), deep infection (16%) and haematoma/seroma (10%) [2]. Another report demonstrated that 13% of the cases required secondary surgery and the implants in the 16% of the cases were removed due to the deep infection [4]. Based on the results of these reports, recently, minimal-invasive surgery has been performed to the lumbopelvic stabilization. The minimal-invasive surgery was shown to be able to reduce the incidence of the complications including surgical site infections [15, 16].
In our series, deep infection developed in one patient (6.7%). Wound cleaning by debridement was applied to this patient. Primary wound closure was possible without implant removal. The skin irritation required implant removal in two patients (13.3%). In SIRF, resection of PSIS is often necessary to insert the S1 pedicle screw, and the distal bone of PSIS is also sufficiently resected to insert iliac screws, which may result in resection of the overall PSIS bone. We thought resection of PSIS in the two cases were insufficient. No marked loss of the reduced position occurred after surgery. Regarding the concern over the fixation ability of SIRF, when iliac screws on the injured side become loose, their role as an anchor against the force of the S1 pedicle screw to dislocate in the vertical direction may be lost. Fortunately, we have not encountered it, but the fixation ability of SIRF should be verified by the accumulation of cases and long-term follow-up. The Majeed score at follow-up was mostly favourable.
Our case series was small, retrospective and included many AO/OTA type B2.3 to C3.3 and spinopelvic dissociation fractures. The selection of unilateral or bilateral pedicle screw insertion into S1 depends on the judgment of attending physicians, and establishment of an indication for SIRF is necessary. As such, we have to observe a longer follow-up period.
Conclusion
SIRF using the “within ring” concept and not including the lumbar spine in the fixation range is a simple, safe, and low-invasive internal fixation method for UPRI.
References
Kach K, Trentz O (1994) Distraction spondylodesis of the sacrum in “vertical shear lesions” of the pelvis [in German]. Unfallchirurg 97:28–38
Bellabarba C, Schildhauer TA, Vaccaro AR et al (2006) Complications associated with surgical stabilization of high-grade sacral fracture displacements with spino-pelvic instability. Spine 31:S80–S88
Schildhauer TA, Bellabarba C, Nork SE et al (2006) Decompression and lumbopelvic fixation for sacral fracture-displacements with spino-pelvic dissociation. J Orthop Trauma 20:447–457
Sagi HC, Militano U, Caron T et al (2009) A comprehensive analysis with minimum 1-year follow-up of vertically unstable transforaminal sacral fractures treated with triangular osteosynthesis. J Orthop Trauma 23:313–319
Bederman SS, Hassan JM, Shah KN, Kiester PD et al (2013) Fixation techniques for complex traumatic transverse sacral fractures: a systematic review. Spine 38:E1028–E1040
Lindahl J, Mäkinen TJ, Koskinen SK et al (2014) Factors associated with outcome of spinopelvic dissociation treated with lumbopelvic fixation. Injury 45:1914–1920
Konig MA, Jehan S, Boszczyk AA et al (2012) Surgical management of U-shaped sacral fractures: a systematic review of current treatment strategies. Eur Spine J 21:829–836
Pearcy MJ, Portek I, Shepherd J (1984) Three dimensional X-ray analysis of normal movement in the lumbar spine. Spine 9:294–297
Keel MJB, Benneker LM, Siebenrock KA (2011) Less invasive lumbopelvic stabilization of posterior pelvic ring instability. J Trauma 71:E62–E70
Mouhsine E, Wettstein M, Schizas C et al (2006) Modified triangular posterior osteosynthesis of unstable sacrum fracture. Eur Spine J 15:857–863
Toogood P, McDonald E, Pekmezci M (2013) A biomechanical comparison of ipsilateral and contralateral pedicle screw placement for modified triangular osteosynthesis in unstable pelvic fractures. J Orthop Trauma 27:515–520
Karakaşlı A, Ceçen B, Erduran M, Taylan O, Hapa O, Havıtcıoğlu H (2014) Rigid fixation of the lumbar spine alters the motion and mechanical stability at the adjacent segment level. Eklem Hastalik Cerrahisi 25:42–46
Lawrence BD, Wang J, Arnold PM, Hermsmeyer J, Norvell DC, Brodke DS (2012) Predicting the risk of adjacent segment pathology after lumbar fusion: asystematic review. Spine 37:S123–S132
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine 29:1938–1944
Keel MJ, Benneker LM, Siebenrock KA, Bastian JD (2011) Less invasive lumbopelvic stabilization of posterior pelvic ring instability: technique and preliminary results. J Trauma 71:62–70
König MA, Seidel U, Heini P, Orler R, Quraishi NA, Boszczyk AA, Boszczyk BM (2013) Minimal-invasive percutaneous reduction and transsacral screw fixation for U-shaped fractures. J Spinal Disord Tech 26:48–54
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Futamura, K., Baba, T., Mogami, A. et al. “Within ring”-based sacroiliac rod fixation may overcome the weakness of spinopelvic fixation for unstable pelvic ring injuries: technical notes and clinical outcomes. International Orthopaedics (SICOT) 42, 1405–1411 (2018). https://doi.org/10.1007/s00264-017-3712-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3712-y