Abstract
Purpose
The studies of the relationship between anterior cruciate ligament (ACL) injury and notch size were in 2-D parameters in Han Chinese, the largest nation in the world, while few studies referred to the 3-D notch volume. The purpose of this study was to determine the differences in notch volume between individuals with and without ACL injuries and the optimal criterion value for abnormal notch volume and its sensitivity in predicting the risk of ACL injuries.
Methods
Two hundred eighty individuals were included in this study, including 140 patients with non-contact sports ACL injuries only and 140 age- and gender-matched individuals without ACL injuries. Both groups underwent pre-operative knee MRI examinations and femoral notches were traced manually on 2-D MRI images, then 3-D notch volume was calculated.
Results
The notch volume was extremely smaller in the ACL-injured group than that in the control group (5.94 ± 1.35 versus 6.86 ± 1.61 cm3, P < 0.001). The notch volume below 6.99 cm3 in males and 5.63 cm3 in females meant being prone to ACL injuries. Females tend to have smaller notch volume than males (5.53 ± 0.93 versus 7.28 ± 1.55 cm3, P < 0.001). The notch volume was in moderate correlation with the body height and weight and in weak correlation with the BMI but in no correlation with the age.
Conclusions
In Chinese Han adults, the notch volume was significantly smaller in the ACL-injured individuals than in the ACL-intact ones, it was smaller in females than the males and it was correlated with the body height, weight and the BMI.
Level of evidence Level III, case-control study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The relationship between ACL injury and femoral notches was first described in 1938 [1], and now, a stenotic notch associated with a high risk of ACL injury has been clarified [2]. The ACL becomes tight to prevent tibial plateau moving ahead in full extension, while it is stretched over the inner side of the lateral femoral condylar in flexion [3, 4]. It may impinge on the inner side of the lateral femoral condylar when receiving anterior shear forces or tibial rotation [5], which would cause an ACL injury.
Although many studies have proved that a narrower femoral notch leads to increased risk of an ACL injury, the evaluation standards were varied, including the notch width index (NWI), the notch width (NW), the intercondylar angle and the tibial plateau slope [1, 6,7,8,9,10]. However, the results could not reach a consistency, perhaps because all of these parameters are based on 2-dimensional (2D) images, which cannot describe the 3-dimensional (3D) space configuration of the notch or evaluate the size perfectly [11, 12]. Few studies tried to determine the relationship between the 3-D notch volume and ACL injuries, but the results were controversial [6, 12,13,14,15], and none of these studies performed the receiver operating characteristic curve (ROC curve), which could show the cut-off value of the notch volume in prediction of the risk of ACL injuries and its sensitivity. Moreover, all of these 3-D studies were small sample researches, neglecting the gender gap or other demographic factors.
The Han Chinese are the largest nation in the world, with the population of more than one billion, which accounts for 92% of the population of China. The incidence of ACL injuries in Chinese athletes is 0.29–0.71%, which is much higher than that of some other countries [16, 17]. However, from all the literatures about notch size we found, only few of them were based on Chinese [18] and none with the notch volume measurement. As the anatomical morphology of the knees, influenced by racial differences [19,20,21,22], might affect the measurement, evaluation of the notch volume in Chinese Han population is needed.
Therefore, the purpose of this study was to determine the differences in the 3-D femoral intercondylar notch volume between individuals with and without ACL injuries. Moreover, the optimal cut-off value of the notch volume in predicting the risk of ACL injuries and the impacts of the demographic factors was also determined.
Methods
Sample size calculation, patient selection and magnetic resonance images taken
The current research was a retrospective case-control study, the ethics of which was approved by our institutional research board. To determine the minimum number of participants required in this study, a sample size calculation was performed based on the results of van Eck et al. [15]. To obtain the power of 0.95 (β of 0.05) and α of 0.01, at least 243 participants in total were needed in the present study. Two hundred eighty individuals were recruited into the study and the sample size reached the statistic requirement.
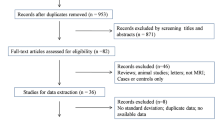
We got a total of 4012 Han Chinese patients in our hospital from June 2015 to July 2016, who hurt their knees in non-contact sport-related injury (Fig. 1). Juveniles were excluded in the research because the epiphyseal plates were not closed in most of them and the potential age-related changes of femoral notch should be ruled out [14]. Since the degenerative changes of joints appeared with age, potential osteophytosis of the notch in the middle-aged and the elderly would cause evident blurring, which should be also eliminated. The ACL-injured patients who hurt their knees more than 1 year before the MRI taken were ruled out [13], for the ACL-deficient knees degenerated much sooner than the normal ones and osteophytosis of the bones might affect the calculation of notch volume. The patients with multiple ligament injuries were also excluded. Therefore, 901 patients were excluded in total.
Nine hundred seventy-three patients had MRI evidence of ACL injury, but 77 of them were excluded by arthroscopy because of partial ACL tears. From the remaining 896 patients, 70 males and 70 females were randomly selected by a computer program as the male ACL-injured group and the female ACL-injured group. Two thousand one hundred thirty-eight patients had no MRI evidence of ACL injury, but 160 of them were excluded because of other ligament injuries or partly ACL injuries. From the remaining 1978 patients, 70 males and 70 females were randomly selected as the control group to match the ACL-injured group by the computer program.
All the participants underwent routine 3.0-T knee MRI through the same scanner (Siemens Verio, 3.0 T) before operation. The axial slices (thickness, 3.0 mm) were selected for the notch volume calculation.
Notch volume measurement
The technique for measuring the notch volume was displayed in Fig. 2, similar to that previously described by Charton et al. [12]. In our research, the image software was Tviews (WinningSoft, China). All the measurements were conducted in the same way twice by a single experienced radiologist. The mean value was noted as the notch volume.
a The most distal level of the intercondylar notch. This was the level that both the femoral condyles were anteriorly continuous. b One of the middle levels of the intercondylar notch. c The most proximal level of the intercondylar notch. This was the level that both the femoral condyles and their cartilages were clearly visible. For notch volume measurement and calculation, firstly, select the sequential 2-D axial slices that clearly displayed the boundaries of the femoral notch, and secondly, manually trace the boundaries based on the anatomic landmarks. The 2-D notch area was calculated by the software automatically. The first slice was the most proximal one that both the femoral condyles (including their cartilages) were clearly visible, and the last slice was the most distal one that both the femoral condyles were anteriorly continuous. Thirdly, calculate the notch volume by summing all the 2-D areas multiplying its slice thickness
Statistical analysis
For all the participant data and the notch data, the mean, standard deviation and standard error were calculated. Unpaired, two-tailed t test was performed to determine the differences between the ACL-injured group and the control group, and the gender differences were also compared. The ROC curve of femoral notch volume was analysed, and the area under the ROC curve (AUC) and the optimal criterion value for distinguishing the risk of ACL injuries in males and females had been calculated. Bivariate Pearson correlation coefficients and their level of significance were calculated between femoral notch volume and their ages, body height, weight and BMI for all 280 participants to ascertain which of these were correlated to the notch volume [13,14,15].
All the statistical analyses were performed by the software Statistical Product and Service Solutions for Windows (SPSS, version 22.0, USA).
Results
There were 280 participants in total, including 140 ACL-injured patients and 140 ACL-intact participants. The mean intercondylar notch volume of each group was showed in Table 1. The notch volume was perceptibly smaller for the ACL-injured cohort than the control cohort (5.94 ± 1.34 versus 6.86 ± 1.61 cm3, P < 0.001), and the females had a predisposition for a smaller femoral notch compared with males (5.53 ± 0.93 versus 7.28 ± 1.55 cm3, P < 0.001).
Subgroup analysis was executed by gender in Table 2. Both the male and female ACL-injured patients had smaller size of the notch than the ACL-intact ones (6.67 ± 1.31 versus 7.89 ± 1.55 cm3 and 5.21 ± 0.94 versus 5.84 ± 0.82 cm3, respectively), and the males tend to have larger notch sizes compared with females regardless of ACL injuries.
The ROC curve of the femoral intercondylar notch volume was performed for the males and females, respectively (Fig. 3). For the males, 6.99 cm3 was the optimal cut-off value for the abnormal femoral notch volume, while for the females, 5.63 cm3 was the optimal cut-off value for the abnormal femoral notch volume.
a ROC curve was performed with the data of the intercondylar notch volume in the ACL-injured males. The area under the ROC curve was 0.719, and less than 6.99 cm3 was the optimal criterion value for determining the abnormal volume of the intercondylar notch, with the sensitivity of 0.729 and the specificity of 0.643. b ROC curve was performed with the data of the intercondylar notch volume in ACL-injured females. The area under the ROC curve was 0.686, and less than 5.63 cm3 was the optimal criterion value for determining the abnormal volume of the intercondylar notch, with the sensitivity of 0.629 and the specificity of 0.686
The correlation between the notch volume and the demographic factors was displayed in Table 3. There was slight to moderate correlation between the notch volume and the body height, weight or BMI (R = 0.561, P < 0.001; R = 0.483, P < 0.001; R = 0.281, P < 0.001, respectively) but no correlation with age (R = − 0.072, P = 0.232).
Discussion
Some researchers put forward the hypothesis that the femoral intercondylar notch stenosis was a risk factor of ACL injuries in the early 20s [1, 23]. Many studies endeavoured to ascertain it, while the results varied because of varied parameters and inevitable errors of the measurement methods.
In our study, one of the most important findings was the conspicuous deviance of the 3-D intercondylar notch volume between the ACL-injured patients and the ACL-intact participants. There have been only three previous studies comparing the 3-D intercondylar notch volume between the ACL-injured and ACL-intact subjects in adult populations with conflictive results. van Eck et al. [15] obtained an inconsistent result compared to ours: the participants with intact ACLs trended to have smaller notch volume: the reasons were not clear, but it was probably caused by the small sample size. On the other hand, the result did not reach statistical significance (P = 0.052). Although others obtained a similar result to ours, the uncertainty still existed. The study of Simon et al. [6] did not mention the measurement of notch volume, and again, it was a small sample size study and reached no statistical significance. In spite of the same method for notch volume measurement, Wratten et al. obtained a much smaller notch volume (4.5 ± 1.1 cm3 in the ACL-injured group and 5.3 ± 1.2 cm3 in the control group) than our results [13], and it was much smaller than juveniles’ (5.5 ± 1.1 cm3 in ACL-injured group and 6.4 ± 1.5 cm3 in the control group) [14]. The reasons were various. The racial difference may cause the diversity of femoral anatomy and the notch volume difference. Also, the personal error of the manual tracing the images would lead to the notch volume deviation.
The differences in the femoral intercondylar notch size between the ACL-injured patients and the normal ones had been confirmed in prior 2-D studies, including the NWI, the NW and the intercondylar angle [1, 6,7,8,9,10]. Keays et al. and Simon et al. [1, 12] found a smaller notch size in the ACL-injured knees than the normal ones, but Harner et al. and Muneta et al. [9, 10] found no such differences. However, these 2-D research methods could not describe the three-dimension configurations of the intercondylar notch. Both Charlton et al. and Van Eck et al. assessed the notch size with the method of both 2-D parameters and 3-D notch volume through CT and MRI, respectively, and the same result of no significant statistical correlation between the 2-D notch parameters and the 3-D notch volume was obtained. As the rotation and angulation in the 2-D measurement are inevitable, the 2-D parameters are not recommended to replace the 3-D notch volume [11, 12]. So, for better describing the femoral notch, 3-D measurement was necessary.
Our study was the first one to perform the optimal cut-off value of the notch volume in risk prediction of ACL injuries with its sensitivity. Different from the previous studies [24,25,26,27,28,29], we calculated the optimal criterion value for males and females, respectively. Because the discrepancies in the size of the notch between males and females were objective, just as the results of previous researches and ours [12,13,14,15, 30], it is not appropriate to establish only one criterion for both males and females. It is noteworthy that the cut-off value is not perfect, because it must take into account the shape of the notch when describing the size of the notch. Past researches have confirmed that the risk of ACL injuries is related to the notch shape, for example, type A notch is more prone to ACL injury [25].
Females suffering ACL injuries much more frequently than males during the same exercise were reported at the end of the twentieth century [12, 31, 32]: possible reasons included extrinsic and intrinsic factors, such as sports skills, physiological hormone factors and anatomical structure diversity of the knee [32]. In our study, the 3-D femoral intercondylar notch volume was significantly smaller in females than that in males in the Chinese Han population, which was similar to that of other races [12,13,14,15, 30]. This result was also confirmed by other researchers in the 2-D measurement [2, 12, 18].
In our study, we analysed the relationship between the notch volume and the demographic factors, and the findings were that the notch volume was moderately correlated to the body height and weight, and weakly correlated to the BMI but not correlated to the age. Major studies were only concerned about the differences in the notch size between the ACL-injured and the ACL-intact knees but ignored other demographic factors. Our finding of no correlation between the age and the notch size was confirmed by most literatures we found [13, 14]. However, it was controversial whether individual differences, including the body height, weight and the BMI, were correlated to the notch size or not. van Eck et al. [15] identified the correlation between the body height and weight and the notch volume was moderate but not for BMI. Wrattan et al. [13] obtained a result of no significant relation between the notch volume and all these demographic factors, which was different to ours. However, these two were small sample researches with low power. Furthermore, it was speculated that the racial difference was one of the important influencing factors which could cause the differences [11, 24, 29]. Our results partly demonstrated the opinion that the demographic factors might be the main reasons of high risk of ACL injuries in females. As the notch volume was significantly associated with the body height, weight and BMI and these in females tended to be lower, the gender differences caused by all these demographic factors could not be ruled out.
Limitations
Our study had potential limitations. First, because a single experienced radiologist measured the notch volume twice, deviation between the observers could not be ruled out; whereas, Vrooijink et al. denoted that the inter- and intra-observer reliability of the MRI measurement was satisfactory [33]. Furthermore, the result of van Eck et al. [15] indicated that the inter-observer homogeneity was very high (r = 0.89) when using the same method to gather data. Thus, our study was convincing. Second, the subjects of the control group were not all normal subjects, which might lead to the bias. To avoid femoral notch volume changes, we excluded the cases with bone defect, bone erosion and osteophytosis displayed on MRI.
Conclusions
A significantly smaller notch volume was found in the non-contact ACL-injured individuals compared with that in the control group in the Chinese Han population, and females trended to have a smaller notch rather than males. The notch volume was correlated with the body height, weight and BMI but not with age.
References
Keays SL, Keays R, Newcombe PA (2016) Femoral intercondylar notch width size: a comparison between siblings with and without anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 24(3):672–679. https://doi.org/10.1007/s00167-014-3491-6
Souryal TO, Freeman TR (1993) Intercondylar notch size and anterior cruciate ligament injuries in athletes. A prospective study. Am J Sports Med 21(4):535–539
Petersen W, Tillmann B (1999) Structure and vascularization of the cruciate ligaments of the human knee joint. Anat Embryol 200(3):325–334
Anderson AF, Lipscomb AB, Liudahl KJ, Addlestone RB (1987) Analysis of the intercondylar notch by computed tomography. Am J Sports Med 15(6):547–552
Olsen OE, Myklebust G, Engebretsen L, Bahr R (2004) Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med 32(4):1002–1012
Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM (2010) A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech 43(9):1702–1707. https://doi.org/10.1016/j.jbiomech.2010.02.033
Anderson AF, Anderson CN, Gorman TM, Cross MB, Spindler KP (2007) Radiographic measurements of the intercondylar notch: are they accurate? Arthroscopy 23(3):261–268. https://doi.org/10.1016/j.arthro.2006.11.003
Alentorn-Geli E, Pelfort X, Mingo F, Lizano-Diez X, Leal-Blanquet J, Torres-Claramunt R, Hinarejos P, Puig-Verdie L, Monllau JC (2015) An evaluation of the association between radiographic intercondylar notch narrowing and anterior cruciate ligament injury in men: the notch angle is a better parameter than notch width. Arthroscopy 31(10):2004–2013. https://doi.org/10.1016/j.arthro.2015.04.088
Muneta T, Takakuda K, Yamamoto H (1997) Intercondylar notch width and its relation to the configuration and cross-sectional area of the anterior cruciate ligament. A cadaveric knee study. Am J Sports Med 25(1):69–72
Harner CD, Paulos LE, Greenwald AE, Rosenberg TD, Cooley VC (1994) Detailed analysis of patients with bilateral anterior cruciate ligament injuries. Am J Sports Med 22(1):37–43
Van Eck CF, Martins CA, Kopf S, Lertwanich P, Fu FH, Tashman S (2011) Correlation between the 2-dimensional notch width and the 3-dimensional notch volume: a cadaveric study. Arthroscopy 27(2):207–212. https://doi.org/10.1016/j.arthro.2010.06.027
Charlton WP, St John TA, Ciccotti MG, Harrison N, Schweitzer M (2002) Differences in femoral notch anatomy between men and women: a magnetic resonance imaging study. Am J Sports Med 30(3):329–333
Wratten CJ, Tetsworth K, Hohmann E (2015) Three-dimensional femoral notch volume in anterior cruciate ligament-deficient versus anterior cruciate ligament-intact patients: a matched case-control study with inter-gender comparison. Arthroscopy 31(6):1117–1122. https://doi.org/10.1016/j.arthro.2014.12.014
Swami VG, Mabee M, Hui C, Jaremko JL (2013) Three-dimensional intercondylar notch volumes in a skeletally immature pediatric population: a magnetic resonance imaging-based anatomic comparison of knees with torn and intact anterior cruciate ligaments. Arthroscopy 29(12):1954–1962. https://doi.org/10.1016/j.arthro.2013.08.031
van Eck CF, Kopf S, van Dijk CN, Fu FH, Tashman S (2011) Comparison of 3-dimensional notch volume between subjects with and subjects without anterior cruciate ligament rupture. Arthroscopy 27(9):1235–1241. https://doi.org/10.1016/j.arthro.2011.03.085
Mihata LC, Beutler AI, Boden BP (2006) Comparing the incidence of anterior cruciate ligament injury in collegiate lacrosse, soccer, and basketball players: implications for anterior cruciate ligament mechanism and prevention. Am J Sports Med 34(6):899–904. https://doi.org/10.1177/0363546505285582
Janssen KW, Orchard JW, Driscoll TR, van Mechelen W (2012) High incidence and costs for anterior cruciate ligament reconstructions performed in Australia from 2003–2004 to 2007–2008: time for an anterior cruciate ligament register by Scandinavian model? Scand J Med Sci Sports 22(4):495–501. https://doi.org/10.1111/j.1600-0838.2010.01253.x
Ouyang X, Wang YH, Wang J, Hong SD, Xin F, Wang L, Yang XW, Wang JR, Wang LM, Wei BO, Wang Q, Cui WD, Fu XL (2016) MRI measurement on intercondylar notch after anterior cruciate ligament rupture and its correlation. Exp Ther Med 11(4):1275–1278. https://doi.org/10.3892/etm.2016.3078
Tannenbaum E, Kopydlowski N, Smith M, Bedi A, Sekiya JK (2014) Gender and racial differences in focal and global acetabular version. J Arthroplast 29(2):373–376. https://doi.org/10.1016/j.arth.2013.05.015
Yue B, Varadarajan KM, Ai S, Tang T, Rubash HE, Li G (2011) Differences of knee anthropometry between Chinese and white men and women. J Arthroplast 26(1):124–130. https://doi.org/10.1016/j.arth.2009.11.020
Harvey WF, Niu J, Zhang Y, McCree PI, Felson DT, Nevitt M, Xu L, Aliabadi P, Hunter DJ (2008) Knee alignment differences between Chinese and Caucasian subjects without osteoarthritis. Ann Rheum Dis 67(11):1524–1528. https://doi.org/10.1136/ard.2007.074294
Shelbourne KD, Gray T, Benner RW (2007) Intercondylar notch width measurement differences between African American and white men and women with intact anterior cruciate ligament knees. Am J Sports Med 35(8):1304–1307. https://doi.org/10.1177/0363546507300060
Palmer I (1938) On the injuries to the ligaments of the knee joint. A clinical study. Acta Chir Scand 53:1–28
Hernigou P, Garabedian JM (2002) Intercondylar notch width and the risk for anterior cruciate ligament rupture in the osteoarthritic knee: evaluation by plain radiography and CT scan. Knee 9(4):313–316
Ireland ML, Ballantyne BT, Little K, McClay IS (2001) A radiographic analysis of the relationship between the size and shape of the intercondylar notch and anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc 9(4):200–205. https://doi.org/10.1007/s001670100197
Stein V, Li L, Guermazi A, Zhang Y, Kent Kwoh C, Eaton CB, Hunter DJ, Investigators OAI (2010) The relation of femoral notch stenosis to ACL tears in persons with knee osteoarthritis. Osteoarthr Cartil 18(2):192–199. https://doi.org/10.1016/j.joca.2009.09.006
Hoteya K, Kato Y, Motojima S, Ingham SJ, Horaguchi T, Saito A, Tokuhashi Y (2011) Association between intercondylar notch narrowing and bilateral anterior cruciate ligament injuries in athletes. Arch Orthop Trauma Surg 131(3):371–376. https://doi.org/10.1007/s00402-010-1254-5
Al-Saeed O, Brown M, Athyal R, Sheikh M (2013) Association of femoral intercondylar notch morphology, width index and the risk of anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc 21(3):678–682. https://doi.org/10.1007/s00167-012-2038-y
Geng B, Wang J, Ma JL, Zhang B, Jiang J, Tan XY, Xia YY (2016) Narrow intercondylar notch and anterior cruciate ligament injury in female nonathletes with knee osteoarthritis aged 41–65 years in Plateau Region. Chin Med J 129(21):2540–2545. https://doi.org/10.4103/0366-6999.192771
Chandrashekar N, Slauterbeck J, Hashemi J (2005) Sex-based differences in the anthropometric characteristics of the anterior cruciate ligament and its relation to intercondylar notch geometry: a cadaveric study. Am J Sports Med 33(10):1492–1498. https://doi.org/10.1177/0363546504274149
Gwinn DE, Wilckens JH, McDevitt ER, Ross G, Kao TC (2000) The relative incidence of anterior cruciate ligament injury in men and women at the United States Naval Academy. Am J Sports Med 28(1):98–102
Arendt E, Dick R (1995) Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med 23(6):694–701
Vrooijink SH, Wolters F, Van Eck CF, Fu FH (2011) Measurements of knee morphometrics using MRI and arthroscopy: a comparative study between ACL-injured and non-injured subjects. Knee Surg Sports Traumatol Arthrosc 19(Suppl 1):S12–S16. https://doi.org/10.1007/s00167-011-1502-4
Acknowledgements
The authors would like to thank Dr. Wei Xiao’er from Radiology Department, Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Shanghai, China for technical guidance.
The authors would like to thank Ms. Yujun Xu for statistical guidance.
Funding
This study received funding from the National Natural Science Foundation of China (81301547) and National Natural Science Foundation of China (31370945).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was approved by Ethics Committee of Shanghai Sixth People’s Hospital (Approval No. 2016-111).
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Zhang, C., Xie, G., Fang, Z. et al. Assessment of relationship between three dimensional femoral notch volume and anterior cruciate ligament injury in Chinese Han adults: a retrospective MRI study. International Orthopaedics (SICOT) 43, 1231–1237 (2019). https://doi.org/10.1007/s00264-018-4068-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4068-7