Abstract
Purpose
To investigate whether epinephrine in irrigation fluid improves visual clarity in arthroscopic shoulder surgery.
Methods
We performed a systematic review and meta-analysis of randomized controlled trials (RCTs) that compared the surgical outcomes of patients who did and did not receive epinephrine during arthroscopic shoulder surgery. We searched the Cochrane Central Register of Controlled Trials, MEDLINE, and Embase for relevant RCTs. We used the Cochrane Collaboration’s tool to assess the risk of bias and adopted random-effects model meta-analysis to combine data. We used the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) methodology to evaluate the overall quality of the body of the retrieved evidence. The primary outcome was visual clarity. The secondary outcomes were operative time, amount of irrigation fluid, the need for increased pump pressure, and adverse cardiovascular events.
Results
This study included three RCTs with a total of 238 participants (124 in the epinephrine group and 114 in the non-epinephrine group). The use of epinephrine in irrigation fluid for shoulder arthroscopy achieved better visual clarity (standardized mean difference, 1.01; 95% confidence interval [CI] 0.63 to 1.39; p < 0.0001) and less need for increased pump pressure (risk ratio, 0.40; 95% CI 0.25 to 0.64; p = 0.0001) compared to the non-epinephrine group. No significant differences were noted in operative time (mean difference − 5.08; 95% CI − 14.46 to 4.31; p = 0.29) and amount of irrigation fluid (mean difference − 1.04; 95% CI − 2.38 to 0.39; p = 0.12) between the two groups. No adverse events were recorded in any of the included trials.
Conclusions
The current evidence shows that the use of epinephrine in arthroscopic shoulder surgery may improve visualization and does not appear to have any major disadvantages.
Level of evidence
Level I
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With improvements in instruments and surgical techniques, arthroscopic treatments of various shoulder diseases have gained popularity. Adequate visual clarity is one of the most important factors for safe and efficient arthroscopic shoulder surgery. Uncontrolled haemorrhage during arthroscopic procedures is one the most common influencing factors on visualization. To improve visualization of shoulder arthroscopy, several methods including thermal coagulation, hypotensive anesthesia, and pump irrigation systems have been developed [1,2,3].
Epinephrine is another common method used to enhance surgical visualization, although its use during arthroscopic surgery is still under debate. Several studies have reported that the addition of epinephrine to irrigation solution could reduce bleeding and improve visual clarity during arthroscopic procedures [4,5,6]. However, adverse cardiopulmonary events related to the use of epinephrine, although rare, have also been reported, including ventricular tachycardia, arrhythmias, and even cardiopulmonary arrest [7,8,9]. With regard to arthroscopic shoulder surgery, at least two trials have reported favourable outcomes following the use of epinephrine [10, 11]. And there is also no consensus on the use epinephrine during arthroscopic shoulder surgery.
To the best of our knowledge, no published systematic reviews have investigated this issue. Therefore, in this study, we systematically evaluated the evidence on the effects of the use of epinephrine during arthroscopic shoulder surgery. The hypothesis of this study was that use of epinephrine in irrigation fluid would increase visual clarity in shoulder arthroscopy than non-use of epinephrine.
Methods
Search strategy
We conducted this systematic review according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [12]. Studies that included patients who underwent arthroscopic shoulder surgery and compared patients who did and did not receive epinephrine were eligible for inclusion. We searched for relevant RCTs from the Cochrane Central Register of Controlled Trials (CENTRAL), PubMed, and EMBASE from inception to December 27, 2017 using the keywords “epinephrine” and “arthroscopic shoulder surgery.” We retrieved both MeSH terms and free text and then used Boolean operators to combine them. The search strategy is detailed in the Supplement (Supp. 1). We also searched any ongoing investigations on this topic from the U.S. National Institutes of Health trials register (http://clinicaltrials.gov). In addition, we contacted specialists in this field for potential ongoing trials or unpublished data on this issue. We also checked the references of the potential studies for potentially eligible trials. We applied no language restriction on trial eligibility.
Selection criteria
We included studies that met the following criteria: (1) RCT design and (2) compared outcomes of patients who did and did not receive epinephrine during arthroscopic shoulder surgery. The exclusion criteria were (1) non-human studies, (2) single arm RCT without control group, and (3) inability to extract data. Two authors independently identified the citations from the searches against the inclusion criteria. We checked the titles and abstracts first and then identified the potentially relevant records by reviewing the full text of the articles. We resolved disagreements by discussion and consulted the third review author for judgment if needed.
Data extraction
Two authors independently extracted pre-specified data from the included studies using a standardized data collection form, including first author, year of publication, study design (patient selection and concealment), details of participants (number, age, sex, etc.), use of epinephrine (concentration and volume), and outcome data including visual clarity, operative time, and adverse cardiovascular events. A third author arbitrated when the two authors disagreed.
The primary outcome was visual clarity. Secondary outcomes included operative time, amount of irrigation fluid, the need for increased pump pressure, and adverse cardiovascular events.
Quality assessment
Two authors independently assessed the risk of bias of the included RCTs using the Cochrane Collaboration’s tool [13, 14]. A third author arbitrated when the two authors disagreed. We evaluated bias of the trials in the following seven domains: random sequence generation, allocation concealment, blinding of patients and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other types of bias [14]. For each domain, each trial was rated as having a high risk of bias, low risk of bias, or unclear risk of bias according to the quality of the trial [13].
The same two authors independently assessed the quality of the body of the combined evidence using the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) approach. We evaluated five domains and rated the strength of evidence for each outcome (GRADEpro, Version 20, McMaster University, 2014).
Data synthesis and analysis
We used a random-effects meta-analysis for all outcomes as inherent clinical heterogeneity was expected across the included RCTs [15]. Data were expressed as mean difference (MD) or standardized mean difference (SMD) with a 95% confidence interval (CI) for continuous data and risk ratio (RR) for dichotomous data. A p value of < 0.05 was considered to be statistically significant. We used X2 and I2 statistics to evaluate statistical heterogeneity with a level of significance set at p < 0.10. I2 values of 0–24.9, 25–49.9, 50–74, and 75–100% were considered to indicate no, low, moderate, and high heterogeneity, respectively [16, 17]. Subgroup analysis was performed if significant heterogeneity was noted. We also estimated between-study variance using the tau-square (τ2) statistic [14]. If the standard deviation of continuous data was not reported, we estimated the mean and variance from the reported median, range, and sample size [18]. When the standard deviation and range were not available, variance was estimated from the p value in the t test. When only graphs were available without raw data for analysis, software was used to extract the details [19]. We used forest plots to report the summary of results. Review Manager 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) was used for the meta-analysis.
Subgroup analysis
If data were available, we performed subgroup analysis including:
-
1.
Different types of surgery
-
2.
Different positions: beach-chair versus lateral decubitus
-
3.
With or without nerve block
Results
Included studies
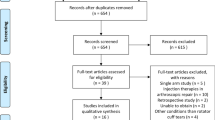
We identified 108 published RCTs after searching PubMed, Embase, and CENTRAL databases (Fig. 1). No additional records were identified from the reference lists of the included RCTs, and no ongoing trials were identified after searching the trial register and consulting specialists. We removed 24 duplicates, leaving 84 records. Two independent authors excluded records after checking the titles and abstracts of these 84 records. The same two authors assessed the full text of the remaining six records. One record was excluded due to a non-RCT design, and two were excluded due to a lack of a control group. We finally included three RCTs in this study: Avery et al. [10], Jensen et al. [11], and van Montfoort et al. [20] (Fig. 1).
Study characteristics
A total of three studies with a total of 238 participants (124 in the epinephrine group and 114 in the non-epinephrine group) were included in the qualitative systematic review (Table 1). The included RCTs were published between 2001 and 2016, and the enrolled sample sizes ranged from 54 to 101.
Epinephrine dose
All of the included studies reported how they added epinephrine to the irrigation solution (Table 2). The epinephrine concentration (1:3,000,000 g/L) was identical across all of the included studies. Two studies used saline for the irrigation solution [11, 20], and the other study used lactated Ringer solution [10].
Characteristic of surgical details
The Jensen trial [11] included patients who received therapeutic and diagnostic shoulder arthroscopy, and the other two trials reported a variety of procedures mainly including rotator cuff repair and intra-articular procedures such as Bankart labral repair [10, 20]. General anesthesia was used in all of the studies, and additional interscalene nerve block was applied in two of the included studies [10, 20]. The initial setting of the pressure-control pump ranged from 30 to 55 mmHg. The details of surgery are shown in Table 2.
Study quality
The Jensen trial [11] did not describe details about the randomization process. Blinding of the patients and surgeons (performance bias) in all trials was generally rated as low risk. Blinding of outcome assessment (detection bias) was generally rated as high risk, since multiple outcome assessors evaluated the outcome subjectively in two of the trials [11, 20]. In addition, two trials did not mention details of the participants with comorbidities or medications that may have increased bleeding tendency, which was rated as an unclear to high risk of bias [11, 20]. The summary of the risk of bias for all of the included trials is shown in Fig. 2a, b.
Visual clarity
All three studies reported on visual clarity using either a visual analogue scale (VAS) or numeric rating scale (NRS). However, the von Montfoort trial [20] only published grading data but not raw data. We could not obtain the full data despite correspondence via email, and thus we could only include two studies in the quantitative meta-analysis. The epinephrine group had better visual clarity compared to the non-epinephrine group (SMD = 1.01; 95% CI 0.63 to 1.39; p < 0.0001) (Fig. 3 and Table 3).
Operative time
Two of the studies reported outcomes on operative time [10, 20]. There was no significant difference in operative time between the epinephrine and the non-epinephrine groups (MD = − 5.08, 95% CI − 14.46 to 4.31; p = 0.29) (Fig. 4a and Table 3). There was no significant difference between the two groups in the number of patients receiving rotator cuff repair only (p = 0.37, Fig. 4b and Table 3).
Amount of irrigation fluid
All three studies reported the total amount of irrigation fluid in the epinephrine and non-epinephrine groups, and no significant difference was found between the two groups (MD = − 1.04, 95% CI − 2.38 to 0.29; p = 0.12) (Fig. 5a and Table 3). In addition, there was no significant difference in the amount of irrigation fluid between the two groups in the patients receiving rotator cuff repair (p = 0.30, Fig. 5b and Table 3).
Need for increased pump pressure
Two of the studies reported findings on the need for increased pump pressure [10, 20]. The Avery trial [10] used an initial pump pressure of 30 mmHg, while the van Montfoort trial [20] set the pressure at 50 mmHg. The meta-analysis showed that the use of epinephrine decreased the need for increased pump pressure (RR = 0.40, 95% CI 0.25 to 0.64; p = 0.0001) (Fig. 6 and Table 3). That is, the use of epinephrine decreased the need for adjusting the pump pressure by 252 (95% CI 151 to 315) per 1000 cases.
Complications
All three studies reported outcomes on complications or adverse cardiopulmonary events. No events were recorded in any of the studies.
GRADE
We used the GRADE methodology to rate the overall quality of evidence. Overall, low to very low quality of evidence showed that the use of epinephrine in arthroscopic shoulder surgery may improve visual clarity and decrease the need for increased pump pressure. The level of evidence was downgraded due to a high risk of detection bias (lack of blinding in outcome assessment), inconsistency, and imprecision (details of judgment are shown in Table S1).
Discussion
The major finding of this study is that the use of epinephrine during arthroscopic shoulder surgery may significantly improve visual clarity and decrease the need for increased pump pressure. There were no significant differences in operative time and the amount of irrigation fluid between the patients who did and did not receive epinephrine, and no adverse events were reported with the use of epinephrine. That is, the use of epinephrine during arthroscopic shoulder surgery could enhance surgical visualization without increasing the risk of adverse events and overall expenditure.
The finding of improved visualization in this study is consistent with previous studies that reported the use of epinephrine in other procedures [5, 6, 21]. Adding epinephrine to irrigation fluid can cause contraction of the local smooth muscle lining of arterioles [21], which can decrease bleeding and thereby improve visual clarity. In clinical studies, Olszewski et al. [6] reported a significant decrease in the use of tourniquets in patients receiving epinephrine (1 mg/L), while Kuo et al. [5] reported that the use of epinephrine without a tourniquet could replace the routine use of a tourniquet in arthroscopic knee surgery. No adverse events were noted in either of these studies [5, 6].
Controlling blood pressure plays a vital role in increasing visualization and minimizing bleeding during arthroscopic shoulder surgery. Unlike other types of surgery of the extremities, tourniquets cannot be used in this anatomical area. Hypotensive anaesthesia is a common method used to control bleeding in arthroscopic shoulder surgery, and regional nerve block can aid in stabilizing haemodynamic changes by blocking pain stimulation due to surgical manipulation during shoulder procedures [22, 23]. The use of pressure/flow control pump irrigation can provide two benefits, including increasing the working space and compression haemostasis [24]. The present study showed that the use of epinephrine could offer better visualization during arthroscopic shoulder surgery even with the combined use of all of the aforementioned factors, although the improved visualization did not translate into higher efficacy as measured by operative time or volume of irrigation fluid. Nevertheless, this benefit is crucial for operators who work with anaesthesiologists who are less familiar with regional block and shoulder arthroscopy or who perform a lower volume of arthroscopic shoulder interventions.
Some studies have reported life-threatening adverse events with arthroscopic shoulder surgery. Although rare, most of these adverse effects were related to the beach-chair position [7, 8, 23]. None of our included studies reported any serious complications such as tachycardia, arrhythmia, or cardiopulmonary arrest associated with the use of epinephrine. This may be due to two factors: first, all of the included trials use the lateral decubitus position and, second, the relatively small number of patients in each study, all of which lacked adequate power to detect these rare complications (i.e., type II error). The debate as to whether the use of epinephrine in arthroscopic shoulder surgery is safe without any risk remains unclear based on the current limited evidence.
Two studies combined general anaesthesia with interscalene nerve block for anesthesia [10, 20]. Some authors hypothesized that these two techniques may lead to hypotension and put the patient at risk, especially in the sitting position. However, a recent prospective RCT found no significant differences in average systolic blood pressure, incidence of mean arterial pressure lower than 60 mmHg, or a decrease in systolic pressure more than 20% from baseline [25]. That is, the combined use of general anaesthesia and interscalene block appeared to be a safe procedure in arthroscopic shoulder surgery in the sitting position. In addition, the use of epinephrine has been reported to efficiently reduce the incidence of unexpected bradycardia and hypotension, which may affect brain perfusion [23, 26]. In short, the use of epinephrine may also minimize the risk of arthroscopic shoulder surgery.
Significant statistical heterogeneity was noted in the two related outcomes of operative time and amount of irrigation fluid. Nevertheless, complex procedures resulted in a longer operative time compared to simple procedures, and the longer the operative time, the larger the amount of irrigation fluid. The main source of heterogeneity of this outcome was due to the van Montfoort study [20], in which the epinephrine group had a shorter operative time than the non-epinephrine group. The diversity of the type of surgery may also have contributed to heterogeneity. As expected, intra-articular arthroscopic shoulder surgery resulted in less bleeding than extra-articular surgery, including rotator cuff repair and subacromial procedures. We then tried to assess the heterogeneity by performing subgroup analysis with limited data. The I2 statistics were decreased in the subgroup focusing on the patients receiving arthroscopic rotator cuff repair (Figs. 4b and 5b). Other factors such as a surgeon effect (two different surgeons), concomitant procedures, and underlying comorbidities with bleeding tendency may also have caused the heterogeneity to some extent.
Strengths and limitations
This study has several strengths. First, it is the first systematic review and meta-analysis of RCTs to explore the effects of the use of epinephrine during arthroscopic shoulder surgery. Second, we comprehensively searched the three largest and most comprehensive databases for relevant RCTs. Third, all of the included RCTs were assessed using the Cochrane Collaboration’s tool for the risk of bias. Fourth, the GRADE approach was used to evaluate the strength of evidence for each outcome.
Our meta-analysis also has some limitations. First, of the three included studies, one was published in 2001 and the other two were published in the past three years. Due to improvements in surgical instruments and techniques over this time period, inevitable bias cannot be avoided. Second, all three of the included studies evaluated outcomes in patients receiving surgery in the lateral decubitus position, which may limit the application of our findings to patients receiving surgery in the sitting position. Third, due to the limited studies available, we were unable to perform all of the planned subgroup analyses. Further studies are needed to evaluate the effects of potential confounding factors including type of surgery, positioning, and nerve block. Fourth, none of the included studies in this review reported long-term outcomes, which makes it impossible to draw any conclusions on the potentially toxic effects of epinephrine on chondrocytes [27].
Conclusions
The current evidence shows that the use of epinephrine in arthroscopic shoulder surgery may improve visual clarity and decrease the load of medical staff without increasing adverse events.
References
Burkhart SS, Danaceau SM, Athanasiou KA (2001) Turbulence control as a factor in improving visualization during subacromial shoulder arthroscopy. Arthroscopy 17:209–212
Morrison DS, Schaefer RK, Friedman RL (1995) The relationship between subacromial space pressure, blood pressure, and visual clarity during arthroscopic subacromial decompression. Arthroscopy 11:557–560
Tuijthof GJ, Dusee L, Herder JL, van Dijk CN, Pistecky PV (2005) Behavior of arthroscopic irrigation systems. Knee Surg Sports Traumatol Arthrosc 13:238–246
Furia JP, Zambetti GJ Jr (1992) An injection technique to create a bloodless field in arthroscopically assisted anterior cruciate ligament reconstruction. Am J Sports Med 20:406–409
Kuo LT, Yu PA, Chen CL, Hsu WH, Chi CC (2017) Tourniquet use in arthroscopic anterior cruciate ligament reconstruction: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet Disord 18:358
Olszewski AD, Jones R, Farrell R, Kaylor K (1999) The effects of dilute epinephrine saline irrigation on the need for tourniquet use in routine arthroscopic knee surgery. Am J Sports Med 27:354–356
Cho SH, Yi JW, Kwack YH, Park SW, Kim MK, Rhee YG (2010) Ventricular tachycardia during arthroscopic shoulder surgery: a report of two cases. Arch Orthop Trauma Surg 130:353–356
Karns JL (1999) Epinephrine-induced potentially lethal arrhythmia during arthroscopic shoulder surgery: a case report. AANA J 67:419–421
Nemani VM, Frank RM, Reinhardt KR et al (2012) Popliteal venotomy during posterior cruciate ligament reconstruction in the setting of a popliteal artery bypass graft. Arthroscopy 28:294–299
Avery DM 3rd, Gibson BW, Carolan GF (2015) Surgeon-rated visualization in shoulder arthroscopy: a randomized blinded controlled trial comparing irrigation fluid with and without epinephrine. Arthroscopy 31:12–18
Jensen KH, Werther K, Stryger V, Schultz K, Falkenberg B (2001) Arthroscopic shoulder surgery with epinephrine saline irrigation. Arthroscopy 17:578–581
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Higgins JP, Altman DG, Gøtzsche PC, Cochrane Bias Methods Group, Cochrane Statistical Methods Group et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ d5928:343
Higgins JP, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. http://www.cochrane-handbook.org. Accessed 15 Dec 2015
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Mitchell M, Muftakhidinov B, Winchen T, et al (2017) Engauge Digitizer Software. Webpage: http://markummitchell.github.io/engauge-digitizer, Accessed 11 Dec 2017
van Montfoort DO, van Kampen PM, Huijsmans PE (2016) Epinephrine diluted saline-irrigation fluid in arthroscopic shoulder surgery: a significant improvement of clarity of visual field and shortening of Total operation time. A randomized controlled trial. Arthroscopy 32:436–444
Funk RH, Wagner W, Rohen JW (1992) The effect of epinephrine on ciliary process vasculature and IOP studied by intraocular microendoscopy in the albino rabbit. Curr Eye Res 11:161–173
Brown AR, Weiss R, Greenberg C, Flatow EL, Bigliani LU (1993) Interscalene block for shoulder arthroscopy: comparison with general anesthesia. Arthroscopy 9:295–300
Lee JH, Min KT, Chun YM, Kim EJ, Choi SH (2011) Effects of beach-chair position and induced hypotension on cerebral oxygen saturation in patients undergoing arthroscopic shoulder surgery. Arthroscopy 27:889–894
Hsiao MS, Kusnezov N, Sieg RN, Owens BD, Herzog JP (2016) Use of an irrigation pump system in arthroscopic procedures. Orthopedics 39:e474–e478
Janssen H, Stosch RV, Pöschl R et al (2014) Blood pressure response to combined general anaesthesia/interscalene brachial plexus block for outpatient shoulder arthroscopy. BMC Anesthesiol 14:50. https://doi.org/10.1186/1471-2253-14-50
Sia S, Sarro F, Lepri A, Bartoli M (2003) The effect of exogenous epinephrine on the incidence of hypotensive/bradycardic events during shoulder surgery in the sitting position during interscalene block. Anesth Analg 97:583–588
Yeh PC, Kharrazi FD (2012) Postarthroscopic glenohumeral chondrolysis. J Am Acad Orthop Surg 20:102–112
Acknowledgements
The authors thank Ms. Yu-Shiun Tsai for her help in searching the databases and obtaining the full text of the trials.
Author information
Authors and Affiliations
Contributions
Author A was responsible for the study concept and design and drafting of the manuscript. Author A and Author B were responsible for the trial selection and appraisal of methodological quality. Author A and Author C participated in acquisition, analysis, and interpretation of data. Author E provided consultation of statistics and methodology. Author F provided consultation of clinical and reviewed the manuscript. Author D and Author E were in charge of the study concept and design, supervised the study, and critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Liang-Tseng Kuo, Chi-Lung Chen, Pei-An Yu, Wei-Hsiu Hsu, Ching-Chi Chi, and Jae-Chul Yoo declare that they have no conflict of interest.
Ethical approval
No ethical approval is needed for our systematic review and meta-analysis.
Informed consent
No identifying information about individual participants was shown in this systematic reivew, and thus inform consent was not needed.
Rights and permissions
About this article
Cite this article
Kuo, LT., Chen, CL., Yu, PA. et al. Epinephrine in irrigation fluid for visual clarity in arthroscopic shoulder surgery: a systematic review and meta-analysis. International Orthopaedics (SICOT) 42, 2881–2889 (2018). https://doi.org/10.1007/s00264-018-4021-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4021-9