Abstract
Background
The goal of this study was to compare the inter- and intra-observer reliabilities of computed tomography (CT) scans of bicondylar tibial plateau fractures (Bi-TPFs) with or without distraction with a bridging external fixation (EF) as interpreted by inexperienced surgeons.
Methods
Patients that underwent CT after distraction with a bridging EF were allocated to group 1 (n = 18), and patients that underwent CT before distraction with a bridging EF were allocated to group 2 (n = 18). Five observers were given plain radiographs and CT images to assess (survey 1) and this assessment was repeated six weeks later (survey 2). Agreements regarding fracture classification and pre-operative planning were evaluated using kappa coefficients. In addition, to evaluate fracture severity, we designed a severity score.
Results
Inter-observer reliabilities for fracture classification and pre-operative planning were higher in group 1 than in group 2. Surveys 1 and 2 revealed similar kappa coefficients in the two study groups. The mean absolute difference (MAD) in severity scores allocated at the two surveys was significantly different between the two groups (P = 0.045). Intra-observer reliabilities of fracture classification and pre-operative planning were also higher in group 1 than in group 2. In addition, level of training was found to have a significant impact on the MAD in severity scores (P = 0.007).
Conclusions
Inter- and intra-observer reliabilities for fracture classification and pre-operative planning were better for inexperienced surgeons when CT was performed after distraction with a bridging EF for Bi-TPFs. Thus, when staged treatment using EF is selected in Bi-TPF patients, the authors suggest that CT scans be performed after distraction with a bridging EF especially for inexperienced surgeons.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since bicondylar tibial plateau fractures (Bi-TPFs) can have disastrous consequences, such as traumatic arthritis and functional disability [1,2,3,4], they must be managed surgically with focus on anatomical restoration of the articular surface. Most surgeons have performed open reduction of articular surfaces and of fracture sites using a multi-directional approach and internal fixation with various plate-screw systems. In addition, many surgeons have attempted temporary bridging external fixation (EF) pre-operatively to prevent additional injury to surrounding structures or fracture sites and to reduce surgical risks and post-operative complications, prior to definitive procedures [5, 6].
The systematic classification of tibial plateau fractures (TPF) according to fracture type and location is critical, since it aids decision-making regarding the surgical approach and method and affects prognosis. Surgeons have used several classification systems for this purpose, such as the Arbeitsgemeinschaft für Osteosynthesefragen Foundation and Orthopaedic Trauma Association classification (AO classification) system. However, several studies have demonstrated that because of its complexity and peculiarities, application of this classification system to TPFs in practice is cumbersome and prone to observer disagreements [7]. To reduce disagreements and provide a better means of evaluating fracture patterns, many authors have advocated the routine use pre-operative computed tomography (CT) rather than conventional radiography to confirm fracture classification and aid surgical planning [8,9,10]. Especially in Bi-TPF, previous studies have also emphasized that pre-operative CT could be more informative and interpretable, after distraction with a bridging EF due to ligamentotaxis [11, 12]. Therefore, we considered that distraction with a bridging EF followed by CT would be especially helpful for inexperienced surgeons in terms of determining fracture patterns and deciding on pre-operative plans in cases of Bi-TPF. However, to our knowledge, no previous study has compared the reliabilities of CT scans performed with or without distraction using a bridging EF in Bi-TPF. In particular, fracture pattern or sub-type determinations might be changed with or without distraction using bridging EF, which would impact surgical planning and outcomes.
Based on this rationale, we aimed to compare the inter- and intra-observer reliabilities of CT scans in Bi-TPF patients with or without distraction using bridging EF as interpreted by inexperienced surgeons. We hypothesized CT images obtained after distraction with a bridging EF would provide a more accurate and reliable means of pre-operative surgical planning than CT images obtained before distraction.
Materials and methods
Patient selection
This study was approved by the institutional review board of our hospital. From January 2012 to January 2014, radiographs and accompanying CT scans of 36 Bi-TPF cases treated by temporary bridging EF were retrospectively reviewed (Figs. 1, 2, 3, 4, and 5). Patients treated using a temporary bridging EF at another medical centre were excluded because distraction was insufficient. Sufficient distraction was based on restoration of normal joint space width.
CT scan of the same patient as in Fig. 1. CT was performed at a local medical centre before distraction with bridging external fixation. a Coronal, b sagittal, and c axial CT images showing a multi-fragmented Bi-TPF. CT, computed tomography; Bi-TPF, bicondylar tibial plateau fracture
Simple radiographs of the same patient as in Fig. 1. The patient was transferred to our hospital and underwent simple radiographs after distraction with bridging external fixation at our hospital
CT scan of the same patient as in Fig. 1. Because he did not provide initial CT images, a second CT scan was performed after distraction with external fixation. a Coronal, b sagittal, and c axial CT images showed that fracture fragments were aligned in their original positions. CT, computed tomography
Intraoperative photo after distraction with bridging external fixation of the same patient as in Fig. 1
The first consecutive 18 Bi-TPF patients, regardless of age, sex, and fracture severity, underwent CT after distraction with a bridging EF and were allocated to group 1 (n = 18). The second set of 18 consecutive Bi-TPF patients underwent CT before distraction with a bridging EF and were allocated to group 2 (n = 18). Ages, sex ratios, pre-operative osteoarthritic changes, and external wound were not significantly different in the two groups. One or 2 weeks after temporary bridging EF, we performed final internal fixation while considering the soft tissue and general condition of patient.
The demographics of patients in the two groups are provided in Table 1. Overall, 36 Bi-TPFs (20 right fractures and 16 left fractures) were identified in 36 patients (25 male and 11 female).
All patients underwent anteroposterior and lateral radiography of the knee (out of plaster) and CT scans prior to definitive internal fixation. Three-dimensional (3D) imaging was performed in all patients, and images were reconstructed using a SOMATOM Definition AS unit (Siemens Medical Solutions, Forchheim, Germany).
Study design
One investigator supervised the entire study, but did not act as an observer or otherwise participate in the study. For the first survey, five observers were given plain radiographs and CT images using picture archiving and communications system (PACS); cases were randomly numbered for each survey. Six weeks after the first survey, the same cases were presented in a different order to the five observers. Observers were not informed that they were assessing the same cases. The observers were two junior, trauma-trained, staff orthopaedic surgeons (surgeons 1 and 2) at a level I trauma centre, two senior orthopaedic residents (residents 1 and 2), and one junior orthopaedic resident (resident 3).
Evaluation tools: classification system, pre-operative planning, and post-operative complication
In this study, we used the AO classification system. According to this system, we classified all 36 fractures as 41 (proximal segment tibia) and type C; observers then evaluated AO groups (1, 2, or 3) and subgroups. And articular classification was devised by dividing the long axis of the tibial articular surface into three equal parts (Fig. 6). The articular classification has seven categories: a, b, c, a + b, b + c, c + a, and a + b + c.
Pre-operative planning was classified according to approach and implant position. Approach and implant position are always influenced by soft tissues, and thus, we assumed that all soft tissues were good enough to apply skin incision. We categorized approaches as anterolateral, posteromedial, posterior, anterolateral + posteromedial, anterolateral + posterior, posteromedial + posterior, and all, and also categorized implant positions as medial, lateral, posterior, medial + lateral, medial + posterior, lateral + posterior, and all.
To evaluate fracture severity, we designed a severity score system based on the system devised by Dodd et al., in which approach and implant position were weighted 2:1, which contrasts with the AO classification, as we considered pre-operative planning more important [13]. AO groups were directly converted into scores; approach and implant position system were awarded 2 points each. The severity score is the sum of all points, and the maximum score was 15. The example of real survey is provided in Table 2. This table is result of Figs. 3 and 4 which are group 1, and observers also reviewed full CT images using PACS.
In addition, group 1 patients were evaluated for complication due to distraction with bridging EF.
Statistical analysis
All statistical analyses, except kappa coefficient analysis, were performed using IBM SPSS version 23.0 (IBM Co., Armonk, NY, USA), and P < 0.05 was considered statistically significant. The Mann-Whitney U test was used to analyze intergroup differences between ages and severity scores, and the chi-square and Fisher’s exact test were used to analyze other intergroup differences. Inter- and intra-observer reliability analysis was performed using Fleiss’s kappa coefficients on R Studio version 0.99 (R Studio Inc., Boston, MA, USA). The kappa values were interpreted according to the guidelines of Landis and Koch [14]: less than 0.0 as “poor,” 0.0 to 0.20 as “slight,” 0.21 to 0.40 as “fair,” 0.41 to 0.60 as “moderate,” 0.61 to 0.80 as “substantial,” and greater than 0.80 as “excellent.”
Results
Inter-observer agreements
Overall, the inter-observer reliabilities of fracture classification were higher in group 1 than in group 2 (Table 3). For the AO group, kappa coefficients were “moderate” in group 1 and “fair” in group 2. For the AO subgroup, kappa coefficients were “fair” in groups 1 and 2, though slightly higher in group 1. For articular classification, kappa coefficients were “moderate” in groups 1 and 2, but slightly higher in group 1.
Pre-operative planning also had higher kappa coefficients in group 1 than in group 2 (Table 3). The kappa coefficients for approach and implant position were “fair” in group 1 and “slight” in group 2. Surveys 1 and 2 showed similar kappa coefficients in both of the groups.
Mean severity scores in group 1 were 10.61 and 10.76 in surveys 1 and 2, respectively; the mean absolute difference between the two surveys in group 1 (MAD_G1) was 0.156 (Table 4). Mean severity scores in group 2 were 9.90 and 10.14 in surveys 1 and 2, respectively; the mean absolute difference between the two surveys in group 2 (MAD_G2) was 0.422. The difference between MAD_G1 and MAD_G2 was statistically significant (P = 0.045).
Intra-observer agreement
Overall, the intra-observer reliabilities for fracture classification and pre-operative planning were higher in group 1 than in group 2 as determined by mean kappa coefficients (Table 5).
Surgeons (1 and 2) showed perfect intra-observer agreement. Resident 1 also showed perfect agreement for the AO group and AO subgroup for groups 1 and 2, but others showed “excellent” kappa coefficients in group 1 and “excellent” to “substantial” in group 2. Surgeons had higher kappa coefficients than residents, and senior residents had higher kappa coefficients than the junior resident. Although the junior resident was unfamiliar with these classifications and pre-operative planning, he achieved perfect intra-observer agreement for articular classification.
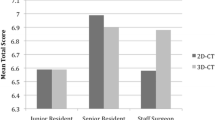
The mean severity scores for all the 36 patients awarded by surgeons were 10.25 and 10.25 for surveys 1 and 2, respectively, and the mean absolute difference between surveys for surgeons (MAD_S) was 0.000 (Table 6). The mean severity scores for all the 36 patients awarded by senior residents were 10.10 and 10.24 for surveys 1 and 2, respectively, and the mean absolute difference between surveys for senior residents (MAD_R) was 0.194. Furthermore, the difference between MAD_S and MAD_R was statistically significant (P = 0.007). These findings indicate level of observer training had a significant impact on mean absolute difference.
Post-operative complication
None of the patients had complications related to motor weakness, sensory change, or circulation due to distraction with bridging EF. There were only cosmetic problems due to pin scar tissue after applying bridging EF.
Discussion
This study was conducted to compare the inter- and intra-observer reliabilities of interpretations of the CT scans of Bi-TPF patients by inexperienced surgeons with or without distraction using bridging EF. The results showed better inter- and intra-observer reliabilities for fracture classification and pre-operative planning when distraction with bridging EF was performed in Bi-TPF patients before CT imaging.
Experts agree that recognition of Bi-TPF characteristics is important to guide clinical and surgical decision-making [15, 16], and thus, many authors advocate CT should be performed after distraction with a bridging EF for Bi-TPFs [11, 12, 17], because slight traction using bridging EF can make CT images easier to interpret, especially by inexperienced surgeons due to ligamentotaxis. However, the issue has not been evaluated thoroughly.
Some studies performed on related topics are of relevance. Chan et al. evaluated the reliability of fracture classification and treatment planning in TPF using simple radiographs with or without CT images and found that additional CT scan increased inter- and intra-observer agreements on treatment planning [8]. Mellema et al. evaluated the reliability and diagnostic accuracy of two-dimensional (2D) and 3D CT in Schatzker types 4 to 6 TPF, and concluded that 2D CT alone showed better reliability and diagnostic accuracy [18]. In the present study, we compared the reliabilities of CT images in Bi-TPF with and without distraction using bridging EF. We found that inter- and intra-observer reliabilities for fracture classification and pre-operative planning were better for inexperienced surgeons when CT was performed after distraction.
Orthopaedic staff surgeons achieved better intra-observer reliabilities than residents, and senior residents performed better than the junior resident. A similar study also reported level of training was associated with better planning scores, although the results obtained were not statistically significant [13]. We believe that level of training aids consistent fracture pattern evaluation and pre-operative planning.
One of the most important aspects of the treatment of Bi-TPF is joint surface recovery, and thus, it is important that joint surfaces be accurately evaluated, which led to our devising an articular classification. Notably, even the junior resident with little orthopaedic knowledge achieved perfect intra-observer agreement in both groups for articular classification. Due to ligamentotaxis, a slight traction by bridging EF aids recovery of the original articular surface [19], and this seemed to be beneficial even when the junior resident evaluated the articular surface. The most widely used classifications in Bi-TPF are AO classification, Schatzker classification [20], and three-column concept [11]. More recently, Chang et al. divided tibial plateau fractures into four columns: anteromedial, anterolateral, posteromedial, and posterolateral [21], and there was also a report that their four-column classification was the most reliable in TPF [22]. However, most of the cases in this study were Schatzker type 5 or 6 and included all columns. Therefore, we could not use these classifications.
There was no complication related to distraction after bridging EF. And there were only cosmetic problems due to pin scar tissue. We suppose the reason for this is that bridging EF was applied only for short period of one to two weeks, and traction was applied manually to prevent excessive force. Egol et al. also evaluated 57 cases of high-energy TPF treated with staged bridging EF and reported that there was no complication related to distraction after bridging EF [23].
When a patient with a Bi-TPF visits an emergency room, the orthopaedic surgeon should evaluate the patient and determine an operative plan before another physician orders a CT scan. The surgeon should decide on conventional open reduction and internal fixation, hybrid EF, or staged treatment using bridging EF. When staged treatment using by bridging EF is selected in Bi-TPF, we suggest that CT should be performed after distraction with bridging EF. Some authors have reported that effective doses delivered during diagnostic CT are similar to those received by Japanese survivors of the atomic bomb [24]. In one study, it was estimated that the numbers of deaths attributable to CT during one year in the USA was 700 for head examination and 1800 for abdominal examination [25]. To avoid unnecessary radiation, surgeons should make operative plans immediately and order initial and final CT scans.
The retrospective nature of this study and the relatively small number of cases and observers are obvious limitations. And the levels of agreement with the participants in this study may simply reflect philosophy of our medical center. Moreover, although all patients had a Bi-TPF, two groups were not exactly the same in terms of fracture configuration. For accurate comparisons, two CT scans were required per patient, but considerations of radiation dose prevent this possibility. However, the first consecutive 18 Bi-TPF patients underwent CT after distraction with a bridging EF and the second consecutive 18 patients underwent CT before distraction although it was not randomized control study. This study is the first to demonstrate that distraction can make CT images more interpretable in Bi-TPF, though further study is needed to determine the clinical results obtained when distraction is performed before CT scan in Bi-TPF. In addition, further study can be also performed about wrist or ankle joints using this study design.
Conclusion
Inter- and intra-observer reliabilities of inexperienced surgeons with respect to fracture classification and pre-operative planning improved when CT was performed after distraction with a bridging EF in Bi-TPF. Thus, when staged treatment using bridging EF is selected in TPF patients, we suggest that a CT scan be performed after distraction with a bridging EF especially when surgeons lack experience.
References
Apley AG (1979) Fractures of the tibial plateau. Orthop Clin North Am 10:61–74
Hohl M (1967) Tibial condylar fractures. J Bone Joint Surg Am 49:1455–1467
Ibsen JG, Mossing N (1971) Conservative treatment of tibial condylar fractures. Acta Orthop Scand 42:431–432
Sarmiento A, Kinman PB, Latta LL, Eng P (1979) Fracutres of the proximal tibia and tibial condyles: a clinical and laboratory comparative study. Clin Orthop Relat Res 145:136-145
Moore TM, Patzakis MJ, Harvey JP (1987) Tibial plateau fractures: definition, demographics, treatment rationale, and long-term results of closed traction management or operative reduction. J Orthop Trauma 1:97–119
Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr (1999) A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma 13:78–84
te Stroet MA, Holla M, Biert J, van Kampen A (2011) The value of a CT scan compared to plain radiographs for the classification and treatment plan in tibial plateau fractures. Emerg Radiol 18:279–283. https://doi.org/10.1007/s10140-010-0932-5
Chan PS, Klimkiewicz JJ, Luchetti WT, Esterhai JL, Kneeland JB, Dalinka MK, Heppenstall RB (1997) Impact of CT scan on treatment plan and fracture classification of tibial plateau fractures. J Orthop Trauma 11:484–489
Wicky S, Blaser PF, Blanc CH, Leyvraz PF, Schnyder P, Meuli RA (2000) Comparison between standard radiography and spiral CT with 3D reconstruction in the evaluation, classification and management of tibial plateau fractures. Eur Radiol 10:1227–1232. https://doi.org/10.1007/s003300000326
Macarini L, Murrone M, Marini S, Calbi R, Solarino M, Moretti B (2004) Tibial plateau fractures: evaluation with multidetector-CT. Radiol Med 108:503–514
Luo CF, Sun H, Zhang B, Zeng BF (2010) Three-column fixation for complex tibial plateau fractures. J Orthop Trauma 24:683–692. https://doi.org/10.1097/BOT.0b013e3181d436f3
Haidukewych GJ (2002) Temporary external fixation for the management of complex intra- and periarticular fractures of the lower extremity. J Orthop Trauma 16:678–685
Dodd A, Oddone Paolucci E, Korley R (2015) The effect of three-dimensional computed tomography reconstructions on preoperative planning of tibial plateau fractures: a case-control series. BMC Musculoskelet Disord 16:144. https://doi.org/10.1186/s12891-015-0608-0
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Maroto MD, Scolaro JA, Henley MB, Dunbar RP (2013) Management and incidence of tibial tubercle fractures in bicondylar fractures of the tibial plateau. Bone Joint J 95-B:1697–1702. https://doi.org/10.1302/0301-620X.95B12.32016
Johnson EE, Timon S, Osuji C (2013) Surgical technique: Tscherne-Johnson extensile approach for tibial plateau fractures. Clin Orthop Relat Res 471:2760–2767. https://doi.org/10.1007/s11999-013-2962-2
Mills WJ, Nork SE (2002) Open reduction and internal fixation of high-energy tibial plateau fractures. Orthop Clin North Am 33:177–198 ix
Mellema JJ, Doornberg JN, Molenaars RJ, Ring D, Kloen P, Traumaplatform Study C, Science of Variation G (2016) Tibial plateau fracture characteristics: reliability and diagnostic accuracy. J Orthop Trauma 30:e144–e151. https://doi.org/10.1097/BOT.0000000000000511
Kumar A, Whittle AP (2000) Treatment of complex (Schatzker type VI) fractures of the tibial plateau with circular wire external fixation: retrospective case review. J Orthop Trauma 14:339–344
Schatzker J, McBroom R, Bruce D (1979) The tibial plateau fracture. The Toronto experience 1968--1975. Clin Orthop Relat Res 138:94-104
Chang SM, Hu SJ, Zhang YQ, Yao MW, Ma Z, Wang X, Dargel J, Eysel P (2014) A surgical protocol for bicondylar four-quadrant tibial plateau fractures. Int Orthop 38:2559–2564. https://doi.org/10.1007/s00264-014-2487-7
Martinez-Rondanelli A, Escobar-Gonzalez SS, Henao-Alzate A, Martinez-Cano JP (2017) Reliability of a four-column classification for tibial plateau fractures. Int Orthop. https://doi.org/10.1007/s00264-017-3543-x
Egol KA, Tejwani NC, Capla EL, Wolinsky PL, Koval KJ (2005) Staged management of high-energy proximal tibia fractures (OTA types 41): the results of a prospective, standardized protocol. J Orthop Trauma 19:448–455 discussion 456
Pierce DA, Preston DL (2000) Radiation-related cancer risks at low doses among atomic bomb survivors. Radiat Res 154:178–186
Brenner D, Elliston C, Hall E, Berdon W (2001) Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 176:289–296. https://doi.org/10.2214/ajr.176.2.1760289
Funding
The authors did not receive grants or outside funding in support of their research or preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the institutional review board of our hospital.
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(XLSX 35 kb)
Rights and permissions
About this article
Cite this article
Ryu, S.M., Park, J.W., Moon, J.J. et al. Computed tomography of bicondylar tibial plateau fractures after distraction with a bridging external fixation. International Orthopaedics (SICOT) 42, 2451–2458 (2018). https://doi.org/10.1007/s00264-018-3853-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3853-7