Abstract
Purpose
A four-column classification system offers a different way of evaluating tibial plateau fractures. The aim of this study is to compare the intra-observer and inter-observer reliability between four-column and classic classifications.
Methods
This is a reliability study, which included patients presenting with tibial plateau fractures between January 2013 and September 2015 in a level-1 trauma centre. Four orthopaedic surgeons blindly classified each fracture according to four different classifications: AO, Schatzker, Duparc and four-column. Kappa, intra-observer and inter-observer concordance were calculated for the reliability analysis.
Results
Forty-nine patients were included. The mean age was 39 ± 14.2 years, with no gender predominance (men: 51%; women: 49%), and 67% of the fractures included at least one of the posterior columns. The intra-observer and inter-observer concordance were calculated for each classification: four-column (84%/79%), Schatzker (60%/71%), AO (50%/59%) and Duparc (48%/58%), with a statistically significant difference among them (p = 0.001/p = 0.003). Kappa coefficient for intr-aobserver and inter-observer evaluations: Schatzker 0.48/0.39, four-column 0.61/0.34, Duparc 0.37/0.23, and AO 0.34/0.11.
Conclusions
The proposed four-column classification showed the highest intra and inter-observer agreement. When taking into account the agreement that occurs by chance, Schatzker classification showed the highest inter-observer kappa, but again the four-column had the highest intra-observer kappa value. The proposed classification is a more inclusive classification for the posteromedial and posterolateral fractures. We suggest, therefore, that it be used in addition to one of the classic classifications in order to better understand the fracture pattern, as it allows more attention to be paid to the posterior columns, it improves the surgical planning and allows the surgical approach to be chosen more accurately.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tibial plateau fractures are complex articular fractures that usually require surgical treatment. The ideal classification for such a fracture should describe its localization, its characteristics, should have high inter-observer reliability, should guide prognosis and assist in surgical planning.
Marchant first described tibial plateau fractures and divided them into: separated, depressed and combined fractures [1]. In 1960, Duparc and Ficat published one of the most complete classifications considering the coronal, sagittal and axial planes [2]. This classification was simplified in 1990 [3]. The Schatzker classification, published in 1979, divides fractures into six types and is the most widely used classification worldwide [4]. It places more attention on the lateral plateau and includes both anterior and posterior tibial plateau fractures. In 1987, the AO group presented an alphanumeric classification for these fractures that is similar to the Schatzker classification but which is more extensive [5]. In 2013, Gicquel compared the Schatzker, AO and revised Duparc classifications, concluding that computerized tomography (CT) scans improve inter-observer agreement, and they found similar results for the Schatzker and the revised Duparc classifications.
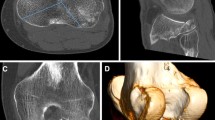
In the past few years, the CT scan has widened the scope of understanding of tibial plateau fractures and has favoured the development of column classifications. In 2010, Luo published the three-column concept for tibial plateau fractures, including a medial, a lateral and a posterior column [6]. This, and other research, has shown that the Schatzker classification might be insufficient to describe some types of fractures, such as those compromising the posterior zone of the tibial plateau [7, 8]. In 1974, Postel published a series comprising 279 cases of posteromedial fracture of the tibial plateau caused due to motorcycle accidents with the knee in flexion [9]. The frequent compromise of the posterior tibia has been identified in other series and this has motivated the use of posterior surgical approaches for treatment [10]. It is estimated that 65% of tibial plateau fractures are compromised of the posterior columns [6, 11, 12]. More recently, Chang et al. (2014) divided tibial plateau fractures into four columns: anteromedial, anterolateral, posteromedial and posterolateral [13], as shown in Fig. 1.
We note that posterior fractures of the tibial plateau have, historically, been ignored, underestimated and mistreated. Classic classifications (such as AO and Schatzker) do not specifically evaluate the posterior part of tibial plateau fractures, and, in other cases (such as Duparc classification), they assess it incompletely. A four-column classification includes the whole articular surface of the proximal tibia. Classic classifications, moreover, have shown important inter-observer variability [14,15,16,17,18]. The aim of this study was to compare the intra-observer and inter-observer variability of a four-column classification compared to classic classifications.
Materials and methods
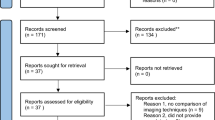
An inter-observer reliability study was performed in a level 1 trauma centre, the Fundación Valle del Lili in Cali, Colombia. Prior to the start of the research, the protocol was evaluated and approved by the Ethics Committee and Institutional Review Board of the Fundación Valle del Lili. The study included patients with tibial plateau fracture that were admitted to the hospital between January 2013 and September 2015. Patients were older than 14 years old, and received both x-rays and computed tomography (CT) of the knee. Fractures were excluded if they were associated with a bone tumour or with previous bone infection.
Once the fractures were deemed to have met the eligibility criteria, demographic data was registered and four orthopaedic surgeons were asked to classify each fracture according to four different classifications: AO, Schatzker, Duparc and 4-column.
Four-column classification system
Using the four columns described by Chang [13], a new classification system was developed in which every column received a letter: anteromedial column (A), anterolateral column (B), posteromedial column (C) and posterolateral column (D). Each fracture can be assigned a minimum of one letter and a maximum of four letters according to the degree of compromise in one or multiple columns. For example, a fracture in the anterolateral column would be represented as B (Fig. 2a and b); a fracture of the four columns as ABCD (Fig. 3a and b); a fracture of the anteromedial, posteromedial and posterolateral columns as BCD (Fig. 4), and so on.
Intra-observer and inter-observer reliability
The four orthopaedic surgeons received the X-rays and CT scan for every case without any extra data or information about the patient and were asked to classify each case. They were instructed in the four classification systems and they received each classification with their proper illustration, to be able to check the classification as necessary. Two were senior orthopaedic surgeons with more than ten years experience in practice and the other two youth orthopaedic surgeons with less than ten years of practice experience. They were blind to demographic data from the patient, to postoperative x-rays, to the radiologists report and to the classifications done by the other participating orthopaedic surgeons. For the intraobserver reliability, one of the senior surgeons was asked to complete the classification of the fractures twice with a two-week interval between them and assigning a different order to the images the second time.
An independent typist registered the results. Demographic descriptive data was analysed calculating means and proportions. Genre, age, aetiology of the fracture, compromise of a posterior column and use of a posterior surgical approach were calculated. Kappa, intra and inter-observer concordance were calculated for the reliability analysis by an independent biostatistician. Stata 13.0 was used for the analysis. Firstly, the intra and inter-observer concordances were calculated by dividing the number of tests that were in agreement by the total number of tests. Chi-squared test was used to calculate differences between percentage agreements. Next, the kappa coefficient was calculated in order to take into account the effect of chance in the degree of agreement between observers. When interpreting kappa, values of 0–0.20 indicate slight agreement, 0.21–0.40 fair agreement, 0.41–0.60 moderate agreement, 0.61–0.80 good agreement, and 0.81–1.00 very good agreement [19].
Results
During the study period, 49 patients fulfilled the eligibility criteria and were included in the study. The mean age of the 49 patients was 39 ± 14.2 years, with a similar proportion of males (51%) and females (49%). Table 1 shows demographic data, including aetiology, showing that motor vehicle accidents were the principal cause of all fractures (69%).
After the observers classified the 49 cases using the four-column classification, it was found that at least one of the posterior columns was affected in 67% of all fractures (n = 33). Nevertheless, only eight cases involved a posterior approach in the surgical management of the fracture.
Intra-observer reliability
The four-column classification showed very high percentage agreement (84%), with significant difference compared to the other classifications (p = 0.001). It was followed by Schatzker (60%), AO (50%) and Duparc (48%). Kappa values were also led by the four-column classification, the only one to show a good agreement (0.61), followed by Schatzker with moderate agreement (0.48), and Duparc (0.370 and AO (0.34), both with fair agreement.
Inter-observer reliability
The inter-observer results showed an overall good degree of agreement across the four observers for the four classifications. The four-column classification showed the highest percentage of agreement (79%), followed by Schatzker (71%), AO (59%) and Duparc (58%), with a statistically significant difference between them (p = 0.003). Meanwhile, kappa values showed a fair agreement for the Schatzker, four-column and Duparc classifications, while AO had only a slight agreement between observers (Table 2).
Discussion
These results show that the four-column classification has the highest percentages of agreement for both intra and inter-observer reliability. It also has the highest kappa value for intra-observer evaluation and is second, after Schatzker, for inter-observer kappa. This shows that the four-column system is a very reliable classification, especially for the results among a same observer. This can be related to the cumulative experience of using it and the easy system of only choosing the affected columns, without having to decide if there is a split, a depression, or both. Therefore, it is a good complement for a classic classification. It has the advantage of being the most reliable and showing how compromised the different topographical areas from the articular surface of the tibial plateau are. Meanwhile, classic classifications are very useful in describing the fracture pattern but are less reliable.
Four-column and Schatzker were the most reliable among the four observers, showing the least variability between them and the lowest probability of chance affecting the results. These are important findings for clinical practice, as practitioners need to be able to speak the same language with colleagues when assessing a tibial plateau fracture, as this affects reliability between different observers.
New classification systems emerge as an attempt to better explain fracture patterns. A new classification, such as the four-columns classification, should be reliable but should also offer additional advantages in comparison to classic classifications. The way of dividing tibial plateau fractures, in the four-column classification, into two anterior and two posterior columns in the articular surface of the proximal tibia, and then assigning one letter to each column, is an easy way to classify these fractures. It also has the advantage of highlighting the posterior columns, which might be important to consider a posterior surgical approach. In this study, there were a high percentage of fractures in the posterior columns (67%), but only 24% of this group of patients were surgically treated through a posterior surgical approach. It is possible that, with the implementation of this new classification system, a higher percentage of cases would receive treatment using a posterior approach.
The main limitation of this classification system is that it provides information only regarding the compromise of the proximal tibia in the articular surface. It can be assumed that as more columns are fractured, the fracture status and prognosis are worse, but there are other important aspects that also need to be considered, such as the fracture pattern, metaphyseal/diaphyseal extension and soft tissue status. These could be assessed using a classic classification, such as Schatzker, and a soft tissue classification such as Tscherne [20]. The clinical practitioner, when classifying a tibial plateau fracture, might need to use the four-column classification in conjunction with a classic classification and a Tscherne classification, in order to make a complete assessment.
For future studies it is important to show the clinical relevance of using this four-column classification. There are some questions that may be answered: does increasing awareness in the posterior tibial plateau correlate with an increase in the use of posterior surgical approaches? Does the use of posterior surgical approaches in those cases correlate with better clinical, functional and radiological results in the short and long-terms?
To our knowledge, no previous studies have described a four-column classification system and compared it to the classic classification systems for tibial plateau fractures. This four-column classification has the advantage of showing the highest percentage of agreement between observers and among the same observer, with the best intraobserver and second best interobserver kappa value. Unlike the other classifications, it also includes the whole articular surface of the tibial plateau and highlights fractures of the posterior column. We therefore recommend its use in the clinical practice.
Conclusion
This new four-column classification offers a reliable system for classifying tibial plateau fractures. It showed the highest intra and inter-observer agreement. When taking into account the agreement that occurs by chance, Schatzker classification had the best interobserver kappa value, but again the four-column had the highest intraobserver kappa value. It should be noted that the four-column classification is a more inclusive classification for posteromedial and posterolateral fractures. We suggest that it should be used with one of the classic classifications in order to better understand fracture patterns, to allow more attention to be paid to the posterior columns, to improve surgical planning and to provide a more systematic way of choosing the best surgical approach.
References
Gerard-Marchant P (1939) Fractures des plateaux tibiaux. Rev Chir Orthop 26:499–546
Duparc J, Ficat P (1960) Fractures Articulares de LExtremite Supérieure du Tibia. Rev Chir Orthop Reparatrice Appar Mot 46:398–486
Huten D, Duparc J, Cavagna R (1990) Fractures récentes des plateaux tibiaux de l’adulte. Éditions Techniques, Enc Med Chir, Appareil locomoteur, Paris
Gicquel T, Najihi N, Vendeuvre T, Teyssedou S, Gayet LE, Huten D (2013) Tibial plateau fractures: reproducibility of three classifications (Schatzker, AO, Duparc) and a revised Duparc classification. Orthop Traumatol Surg Res 99(7):805–816. doi:10.1016/j.otsr.2013.06.007
Schatzker J, McBrown R, Bruce D (1979) The tibial plateau fracture: the Toronto experience 1968-1975. Clin Orthop Relat Res 138:94–104
Muller ME, Nazarian S, Koch P (1987) Classification AO des fractures. Springer, Berlin
Luo CF, Sun H, Zhang B, Zeng BF (2010) Three column fixations for complex tibial plateau fractures. J Orthop Trauma 24(11):683–692. doi:10.1097/BOT.0b013e3181d436f3
Molenaars RJ, Mellema JJ, Doornberg JN, Kloen P (2015) Tibial plateau fracture characteristics: computed tomography mapping lateral, medial, and bicondylar fractures. J Bone Joint Surg Am 97(18):1512–1520. doi:10.2106/JBJS.N.00866
Postel M, Mazas F, de la Caffinière JY (1974) Posterior fracture-separation of the tibial plateaux. Rev Chir Orthop Reparatrice Appar Mot 60(2 Suppl):317–323
Martínez A, Cayón M (1999) Fracturas del platillo tibial postero medial. Rev Colomb Ortop Traumatol 13(1):37–41
Doornberg JN, Rademakers MV, van den Bekerom MP, Kerkhoffs GM, Ahn J, Steller EP, Kloen P (2011) Two-dimensional and three-dimensional computed tomography for the classification and characterisation of tibial plateau fractures. Injury 42(12):1416–1425. doi:10.1016/j.injury.2011.03.025
Yang G, Zhai Q, Zhu Y, Sun H, Putnis S, Luo C (2013) The incidence of posterior tibial plateau fracture: an investigation of 525 fractures by using a CT-based classification system. Arch Orthop Trauma Surg 133(7):929–934. doi:10.1007/s00402-013-1735-4
Chang SM, Hu SJ, Zhang YQ, Yao MW, Ma Z, Wang X, Dargel J, Eysel P (2014) A surgical protocol for bicondylar four-quadrant tibial plateau fractures. Int Orthop 38(12):2559–2564. doi:10.1007/s00264-014-2487-7
Sohn HS, Yoon YC, Cho JW, Cho WT, Oh CW, Oh JK (2015) Incidence and fracture morphology of posterolateral fragments in lateral and bicondylar tibial plateau fractures. J Orthop Trauma 29(2):91–97. doi:10.1097/BOT.0000000000000170
Hu YL, Ye FG, Ji AY, Qiao GX, Liu HF (2009) Three-dimensional computed tomography imaging increases the reliability of classification systems for tibial plateau fractures. Injury 40(12):1282–1285. doi:10.1016/j.injury.2009.02.015
Lowe JA, Tejwani N, Yoo B, Wolinsky P (2011) Surgical techniques for complex proximal tibial fractures. J Bone Joint Surg Am 93(16):1548–1559
Johnson EE, Timon S, Osuji C (2013) Surgical technique: Tscherne-Johnson extensile approach for tibial plateau fractures. Clin Orthop Relat Res 471(9):2760–2767. doi:10.1007/s11999-013-2962-2
Zeltser DW, Leopold SS (2013) Classifications in brief: Schatzker classification of tibial plateau fractures. Clin Orthop Relat Res 471(2):371–374. doi:10.1007/s11999-012-2451-z
Altman DG (1992) Practical statistics for medical research. Chapman & Hall, London
Tscherne H, Oestern HJ (1982) A new classification of soft-tissue damage in open and closed fractures. Unfallheilkunde 85(3):111–115
Acknowledgements
The authors thank Dr. Helen Reina for the copy editing of this manuscript, as well as Juan Esteban Restrepo, for his help with statistical calculations and analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Funding
This research received no funding.
Informed consent
For this type of study formal consent is not required.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The institutional review board approved this study.
Rights and permissions
About this article
Cite this article
Martínez-Rondanelli, A., Escobar-González, S.S., Henao-Alzate, A. et al. Reliability of a four-column classification for tibial plateau fractures. International Orthopaedics (SICOT) 41, 1881–1886 (2017). https://doi.org/10.1007/s00264-017-3543-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3543-x