Abstract
Distal tibia fractures are reported to have a high complication rate pre-operatively as well as post-operatively, which can include open fractures, soft tissue damage, infection, malalignment, pseudarthrosis and ankle arthrosis. The operative treatment for the extra-articular distal tibia fractures is a controversial topic in the orthopaedic literature. Some of these fractures are proximal enough to be treated with an intramedullary nail while others are too distal for that. The aim of our study was to compare the results we have had with intramedullary nail (IMN) and minimally invasive plate osteosynthesis (MIPO) in distal metaphyseal (extra-articular) tibia fractures. The study was designed prospectively between January 2013 and March 2016 and took place on the Orthopaedics and Traumatology ward of a Clinical Emergency County Hospital in western Romania. The follow-up visits were scheduled one month, three months and six months post-operatively. For evaluating the ankle function, we used the Olerud–Molander ankle score (OMAS) and union was evaluated at six months on ankle X-rays. At the six-month follow-up visit the average scores were 75.55 (20-100) for the IMN lot and 74.23 (20-90) for the MIPO lot, without finding any statistical difference between the two groups (p >0.1). At the six-month follow-up, X-ray union was objected in 48 (90.5%) of our patients, the IMN lot having worse results (85.18%) than the MIPO lot (96.15%). The results we encountered showed little to no statistical difference when it comes to the functional score we used (OMAS score), leading us to believe that you can achieve comparable results with both implants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal tibia fractures (DTF) are usually caused by high-traumatic accidents and affect active patients. They are reported to have a high complication rate pre-operatively as well as post-operatively, including open fractures, soft tissue damage, infection, malalignment, pseudarthrosis and ankle arthrosis. Functional cast bracing is known to have bad end-results such as a high incidence of ankle stiffness and deformity [1]. Just like in other intra-articular fractures, to obtain a proper diagnosis, we must often use other imagistic techniques such as the computer tomography (CT) [2]. This allows for a better diagnosis and indication, improving the outcome.
The operative treatment for the extra-articular distal tibia fractures is a controversial topic in the orthopaedic literature. Some of these fractures are proximal enough to be treated with an intramedullary nail while others are too distal for that. Furthermore, many surgeons are more familiar with one technique or the other, preferring plates to nails or vice versa. Surgical treatment options vary a lot, most specialists nowadays using either minimal invasive plating osteosynthesis (MIPO), intramedullary nailing (IMN) or external fixator options (ExFix). Each of these treatment options have been discussed in the literature, emphasising on their indications, advantages and disadvantages [3,4,5]. Controversy still exists over the clinical efficacy of each option and its cost-effectiveness [6].
Superior results have been noticed in certain conditions (good soft tissue quality, low energy trauma) when performing open reduction and internal fixation (ORIF) [7]. It was noticed that, when performed on patients with associated nerve or vascular injury, wound complications and infections, ORIF tends to yield bad results, thus increasing the length of the hospitalisation and the number of surgical interventions done subsequently [8]. IMN allows for a minimally invasive, stable fixation with early mobilisation [9], but on the other hand causes an increased number of anterior knee pain and malunions [10].
The aim of our study was to compare the results we have had with IMN and MIPO osteosynthesis in distal metaphyseal (extra-articular) tibia fractures.
Materials and methods
The study was designed prospectively between January 2013 and March 2016 and took place on the Orthopaedics and Traumatology ward of a Clinical Emergency County Hospital in western Romania. The patients were approached for study inclusion after being admitted in our hospital with a distal tibia fracture classified as Muller AO 43-A. The inclusion criteria were: (1) distal metaphyseal tibia fracture AO 43-A, (2) a healthy cognitive status and (3) skeletal maturity (over 18 years old). The exclusion criteria of our study were: (1) intraarticular fractures (AO 43-B/C), (2) pathologic bone fractures, (3) pre-existent trophic changes of the soft tissue, and (4) the indication for an external fixator. The patients were attributed to one of the lots (IMN/MIPO) by the surgeon’s consideration, without being randomised.
The IMN technique was realised using a sub-patellar approach. We used intramedullary nails in a closed reduction internal fixation manner. We standardly used two proximal screws and two distal screws to lock the nail. The MIPO technique was achieved through an anteromedial approach (approximately 5 cm) realised near the tibial malleolus and we used the bridging plate theory. When associated with a peroneal fracture, this was operated first (standard lateral approach), to re-establish the length of the limb.
The follow-up visits were scheduled one month, three months and six months postoperatively. For evaluating the ankle function, we used the Olerud–Molander ankle score (OMAS) because this is a disease-specific test (ankle fractures) that has been validated and it also showed a high test-retest reliability [11]. Bone consolidation was evaluated on the six-month X-rays by the same radiology specialist. Complications such as open fractures, wound complications, malunions, infections and lack of consolidation were recorded.
The statistical analysis (frequencies, means, paired t-test) was performed using the IBM SPSS Statistics 20 software (copyright IBM Corporation 2011).
The study was approved by our hospital’s Ethical Committee Board and is in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Results
Fifty-three patients (37 males, 16 females) with an average age of 37 (18–65) years old were divided into two groups. Our IMN lot had 27 patients (19 males and 8 females) with an average age of 39.2 (18–55) years old and our MIPO lot had 26 patients (18 males and 8 females) with an average age of 33.1 (18–65) years old. Regarding the classification, 12 were AO 43-A1, 18 were AO 43-A2 and 23 were AO 43-A3. The characteristics of our studied lots can be seen in Table 1.
Open fractures were present in 14 patients and they were classified as Gustilo Anderson type I (6 patients), Gustilo Anderson type II (4 patients) and Gustilo Anderson type III (4 patients). Ten of these patients were from the IMN lot and four were from the MIPO lot.
The IMN lot’s complications were four varus malunions (>5o), three patients developed pseudarthrosis, three patients presented with ankle stiffness after six months and one patient had a post-operative infection that required multiple re-interventions (external fixator, rib bone graft and plating). The MIPO lot’s complications were three dehiscent wounds, four recurvatum malunions and four ankle stiffness cases after six months.
Our average one-month OMAS scores were 10.18 (0–25) for the IMN group and 8.26 (0–20) for the MIPO group. At the six-month follow-up visit the average scores were 75.55 (20–100) for the IMN lot and 74.23 (20–90) for the MIPO lot, without finding any statistical difference between the two groups (p > 0.1). At the six-months follow-up, X-ray union was objected in 48 (90.5%) of our patients, the IMN lot having worse results (85.2%) than the MIPO lot (96.15%). Our outcome scores and our complication rates can be seen in Table 2.
We had a 7.5% (4 patients) overall infection rate, with most of the cases being superficial infections from the MIPO lot, and this rate somehow reflecting the high number of open fractures that we had (14 patients, 26.4%). These superficial infections were treated with antibiotherapy, local curettage and secondary wound suture, due to the dehiscence. The one case that had a deep infection was an open fracture from the IMN lot, and it required secondary external fixation, antibiotherapy and ulterior bone grafting with a vascularized rib graft. Statistically significant data was found regarding the encountered types of malunion. All the varus malunion cases were part of the IMN lot (p = 0.047) while all the recurvatum malunions were part of the MIPO lot (p = 0.045). As expected, ankle stiffness was seen in both lots with similar incidence.
Discussion
Plates seem to be the obvious choice for this area and the AO group has described minimally invasive techniques (MIPO—minimally invasive percutaneous osteosynthesis) for implanting plates percutaneously in this anatomical site [12, 13]. Plate reconstruction is also known to provide reliable results in other intra-articular fractures of the lower limb [14]. Extensive studies have been done to compare MIPO techniques with conventional ones [15,16,17]. The main aim of minimally invasive surgery was to get the benefits of plating (anatomic reduction, axis restoration, stable fixation) but without the soft tissue complications and the devascularisation of fracture fragments that occur during open surgery.
Zou et al. published an investigative review study and they concluded that there is no significant difference between open and closed fixation and recommended between MIPO and open reduction depending on fracture pattern [18]. A suitable alternative for decreasing local edema, and avoiding unnecessary bleeding can be the use of tranexamic acid, which has already proved its benefits in arthroplasties [19]. Paluvadi et al. concluded that the MIPO technique (Fig. 1) provides good, slightly delayed bone healing, decreases incidence of non-union and the need for bone grafting. They recommend this technique to be used where intramedullary locked nailing cannot be performed [16].
Pre-operative and three-month post-operative, AP and lateral X-rays of the ankle and calf. Osteosynthesis was achieved with an angular stable plate with locked screws inserted with the MIPO technique for the distal tibia, and a simple plate and screws for the fibula. Union is slowly starting to occur in a 43-year-old male patient with a AO 43-A3 distal tibial fracture
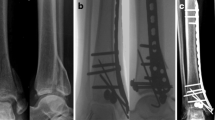
IMN can be a less obvious choice for these fractures, but if the fracture pattern allows it, meaning an extra-articular fracture of the distal tibial diaphysis, or a fracture with nondisplaced intra-articular fragments, an intramedullary nail can be a very effective solution for internal fixation (Fig. 2). El Attal et al. studied 180 tibial fractures in which they included extra-articular fractures of the distal tibia (AO 43 A1/A2/A3) treated with closed reduction and reamed IMN. They had a 10.6% rate of delayed union and a 5.4% rate of 5° or more axial malalignment [20]. Hoegel et al. compared reamed and unreamed nailing either with angle stable or conventional interlocking to plate osteosynthesis on four groups of artificial tibiae. They found out that the reamed nailing was biomechanically superior to the unreamed conventionally locked nail and unreamed distally angular stable locked nails and these implants were stiffer than the locked plate osteosynthesis, an implant that had the highest values of torsional and axial force movement [21]. Kuhn et al. studied a prototype retrograde tibial nail in cadaveric specimens and found it to be superior to the classic MIPO technique (superior stability and higher load to failure forces) [22].
Pre-operative and three-month post-operative, AP and lateral X-rays of the ankle and calf. Osteosynthesis was achieved with a locked intramedullary nail for the distal tibia fracture, and a plate and screws with three additional neutralisation screws for the fibula. The nail was distally locked with three screws (1 anteroposterior, 1 oblique and 1 lateral). This is a 26-year-old male patient with a AO 43-A3 distal tibial fracture caused by a car accident
These studies all point out that for extra-articular distal tibial fractures, the IM nailing, either antegrade or retrograde, is a better choice than the classic angle stable locked MIPO technique. While the latter has been proven in clinical practice and can address fractures with articular extension or comminution it can also cause soft tissue complication, decreased distal vascularization, increased rate of delayed and non-union and later weight-bearing, all these being minimally influenced by the locked nail. This can also be extremely important in open fracture cases where a IM nail provides excellent fixation of the fracture fragments and allows, if necessary, extensive debridement and reconstructive treatment of the soft tissues without direct implant exposure.
Looking forward and already having seen the computerization of several implants such as the Taylor Spatial Frame [23,24,25] and patient-specific instrumentation in joint replacements and corrective osteotomies [26, 27], we hope that future solutions can be found for some further enhancement of plates and nails.
Conclusion
The results we encountered showed little to no statistical difference when it comes to the functional score we used (OMAS score), leading us to believe that you can achieve comparable results with both implants. Of course, there are cases that can make the surgeon chose one implant over the other and this is where the surgeon’s experience plays a far more significant role than guideline recommendations. From what we have learned, we can say that it is extremely important to avoid malalignment during fixation and applying the MIPO technique when the skin is in poor condition.
References
Digby JM, GMN H, Webb JK (1982) A study of function after tibial cast bracing. Injury 14:432–439
Deleanu B, Prejbeanu R, Tsiridis E, Vermesan D, Crisan D, Haragus H, Predescu V, Birsasteanu F (2015) Occult fractures of the proximal femur: imaging diagnosis and management of 82 cases in a regional trauma center. World J Emerg Surg 10:55. https://doi.org/10.1186/s13017-015-0049-y
Marcus MS, Yoon RS, Langford J et al (2013) Is there a role for intramedullary nails in the treatment of simple pilon fractures? Rationale and preliminary results. Injury 44:1107–1111
Li Y, Jiang X, Guo Q, Zhu L, Ye T, Chen A (2013) Treatment of distal tibial shaft fractures by three different surgical methods: a randomized, prospective study. Int Orthop 38:1261–1267
Kuhn S, Greenfield J, Arand C et al (2015) Treatment of distal intraarticular tibial fractures: a biomechanical evaluation of intramedullary nailing vs. angle-stable plate osteosynthesis. Injury 46:99–103
Kuo LT, Chi CC, Chuang CH (2015) Surgical interventions for treating distal tibial metaphyseal fractures in adults. Cochrane Database Syst Rev 3:Cd010261
Piatkowski K, Piekarczyk P, Kwiatkowski K, Przybycien M, Chwedczuk B (2015) Comparison of different locking plate fixation methods in distal tibia fractures. Int Orthop 39(11):2245–2251
Kayali C, Agus H, Eren A, Ozluk S (2009) How should open tibia fractures be treated? A retrospective comparative study between intramedullary nailing and biologic plating. Ulus Travma Acil Cerrahi Derg 15(3):243–248
Megas P, Zouboulis P, Papadopoulos AX, Karageorgos A, Lambiris E (2003) Distal tibial fractures and non-unions treated with shortened intramedullary nail. Int Orthop 27(6):348–351
Li Y, Liu L, Tang X, Pei F, Wang G, Fang Y et al (2012) Comparison of low, multidirectional locked nailing and plating in the treatment of distal tibial metadiaphyseal fractures. Int Orthop 36:1457–1462
Nilsson GM, Eneroth M, Ekdahl CS (2013) The Swedish version of OMAS is a reliable and valid outcome measure for patients with ankle fractures. BMC Musculoskelet Disord 14:109. https://doi.org/10.1186/1471-2474-14-109
Wagner M, Frigg R (2006) AO manual of fracture management—internal fixators: concepts and cases using LCP/LISS. Thieme Publishing Group, Nederlands Tijdschrift voor Traumatologie
Wagner M (2003) 1. Injury 34(Suppl 2:B):31–42
Deleanu B, Prejbeanu R, Crisan D, Predescu V, Popa I, Poenaru DV (2015) Gait characteristics before hardware removal in patients operated upon for tibial plateau fractures. Int Orthop 39(7):1411–1415
Gupta RK, Rohilla RK, Sangwan K, Singh V, Walia S (2010) Locking plate fixation in distal metaphyseal tibial fractures: series of 79 patients. Int Orthop 34(8):1285–1290
Paluvadi SV, Lal H, Mittal D, Vidyarthi (2014) Management of fractures of the distal third tibia by minimally invasive plate osteosynthesis—a prospective series of 50 patients. J Clin Orthop Trauma 5(3):129–136
Ahmad MA, Sivaraman A, Zia A, Rai A, Patel AD (2012) Percutaneous locking plates for fractures of the distal tibia: our experience and a review of the literature. J Trauma Acute Care Surg 72(2:E):81–87
Zou J, Shi Z-M, Zhang W, Zhang C-Q (2012) Open reduction and internal fixation better than percutaneous plate osteosynthesis in distal tibial fractures. J Invest Surg Informa Healthcare USA 25(5):326–329
Predescu V, Jinescu G, Olaru RI, Prescura C, Deleanu B (2016) Study of the tranexamic acid on blood loss in arthroplasty. RevChim 67(8):1513–1515
Attal ELR, Hansen M, Rosenberger R, Smekal V, Rommens PM, Blauth M (2011) Intramedullary nailing of the distal tibia illustrated with the expert(TM) tibia nail. Oper Orthop Traumatol 23(5):397–410
Hoegel FW, Hoffmann S, Weninger P, Bühren V, Augat P (2012) Biomechanical comparison of locked plate osteosynthesis, reamed and unreamed nailing in conventional interlocking technique, and unreamed angle stable nailing in distal tibia fractures. J Trauma Acute Care Surg 73(4):933–938
Kuhn S, Appelmann P, Mehler D, Pairon P, Rommens PM (2014) Retrograde tibial nailing: a minimally invasive and biomechanically superior alternative to angle-stable plate osteosynthesis in distal tibia fractures. J Orthop Surg Res Bio Med Central Ltd 9(1):35
Sala F, Thabet AM, Capitani P, Bove F, Abdelgawad AA, Lovisetti G (2017) Open supracondylar-intercondylar fractures of the femur treatment with Taylor spatial frame. J Orthop Trauma 31(10):546–553 doi. https://doi.org/10.1097/BOT.0000000000000923
Shah AB, Jones C, Elattar O, Naranje SM (2017) Tibiotalocalcaneal arthrodesis with intramedullary fibular strut graft with adjuvant hardware fixation. J Foot Ankle Surg 56(3):692–696
Morris R, Hossain M, Evans A, Pallister I (2017) Induced membrane technique for treating tibial defects gives mixed results. Bone Joint J 99-B(5):680–685
Predescu V, Prescura C, Olaru R, Savin L, Botez P, Deleanu B (2017) Patient specific instrumentation versus conventional knee arthroplasty: comparative study. Int Orthop 41(7):1361–1367
Haglin JM, Eltorai AE, Gil JA, Marcaccio SE, Botero-Hincapie J, Daniels AH (2016) Patient-specific orthopaedic implants. Orthop Surg 8(4):417–424
Acknowledgements
Not applicable.
Funding
There is no funding source
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the SCJU Pius Branzeu Research Committee and with the 1964 Helsinki declaration and its later amendments.
Rights and permissions
About this article
Cite this article
Mioc, ML., Prejbeanu, R., Deleanu, B. et al. Extra-articular distal tibia fractures—controversies regarding treatment options. A single-centre prospective comparative study. International Orthopaedics (SICOT) 42, 915–919 (2018). https://doi.org/10.1007/s00264-018-3775-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3775-4