Abstract
Purpose
Limb salvage surgery is increasingly used for the treatment of distal femur bone sarcomas. Total knee replacement using megaprosthesis and epiphysis-sparing biologic reconstruction using an allograft are widely used in order to preserve joint motion. We aimed to compare the results of these procedures using gait analysis in patients undergoing limb salvage surgery.
Methods
Fifteen patients were included, nine undergoing allograft with epiphysis sparing (Allograft group) and six undergoing megaprosthesis (Megaprosthesis group). Every patient underwent a gait analysis using the Plug-in-Gait protocol. Spatiotemporal parameters, knee kinematics, and kinetics were compared between the two groups and a cohort of ten asymptomatic subjects. Knee function was assessed by the Gait Deviation Index (GDI) and the Gilette Gait Index (GGI).
Results
Both treatment groups showed decreased knee flexion during the loading response phase. Megaprosthesis patients showed a decreased knee flexion all along stance phase. There was no difference in gait pattern between the treatment groups. GDI was significantly lower in Megaprosthesis and Allograft patients when compared to controls (86.4 and 84.3 vs 94, all p < 0.05). This difference was not clinically relevant.
Conclusion
Our study reveals that Megaprosthesis and Allograft patients did not show differences in gait patterns and global function. Even though Allograft and Megaprosthesis patients have significant changes in gait pattern, knee function is acceptable with effective gait mechanisms. Changes occur during stance phase and are due to the quadriceps weakness. The particular pattern of gait in Megaprosthesis patients could be a concern for prosthesis wear and should be investigated on this specific aspect.
Level of evidence: 4
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Modern techniques have enabled surgeons to increasingly perform limb salvage surgery in patients suffering from distal femur malignancies. To this end, limb salvage surgery has resulted in limb-sparing treatment for more than 65% of patients diagnosed with osteosarcoma [1]. The five-year overall survival rate has now reached 72% after such a procedure for patients diagnosed with osteosarcoma or Ewing’s sarcoma. For the past decade, this kind of treatment has been associated with increased survivorship with a five-year survival rate around 60–80%. Thus, the long-term functional results are becoming a major concern [2,3,4,5]. Indeed, the large resection of bone and muscles after these procedures has been shown to jeopardize knee function [6]. However, it is difficult to obtain an objective assessment of knee function and motion in these patients. Moreover, as medical therapies will enable longer life spans in these patients, it is of primary interest to further investigate knee joint function after reconstruction surgery.
Depending on the location of the tumour and the involvement of knee joint, patients with a distal femur malignant bone tumour can undergo two different types of resection surgery. If the joint is not involved, and if there is sufficient remaining epiphysis, patients are eligible for biological reconstruction with allograft which enables surgeons to spare the knee joint. On the other hand, if the joint cannot be preserved, then the reconstruction will necessitate a total knee replacement with massive endoprosthesis.
The investigation of pathological gait and limb mechanics has been of clinical importance for decades [7], and modern tools such as gait analysis have provided repeatedly validated means for the assessment of lower limb kinematics and kinetics [8, 9]. In addition to time and distance parameters, gait analysis is able to give information about knee motion, moments and constraints applied to the joints. Gait analysis is now part of the current clinical practice in numerous fields of orthopaedic surgery, such as assessment of the pre and post-operative gait impairment that occurs in cerebral palsy. Further, such analysis is becoming increasingly used after joint replacement surgery to assess functional results [10].
The purpose of our study was to compare knee function after megaprosthesis and allograft reconstruction in patients undergoing limb salvage surgery for malignant distal femur tumour using gait analysis.
Methods
Study design
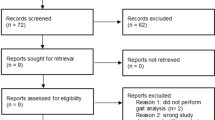
We conducted a single-centre, retrospective study of a prospective collected database. Inclusion criteria were: (1) paediatric patients with diagnosis of malignant bone tumour of the distal femur (osteosarcoma or Ewing’s sarcoma), (2) who underwent limb salvage surgery, and (3) reconstruction with either megaprosthesis or allograft augmented with fibular graft. Patients with less than three years of post-operative follow-up were excluded from the study. Patients were compared to ten asymptomatic volunteers who composed the control group. After approval from our institutional ethical committee, informed consent was obtained from each participant.
In total, 15 patients met the inclusion criteria. Study population characteristics are summarized in Table 1. Overall, the mean age was 25.2 years old (± 5.7, from 18 to 35.9 years old) and the mean follow-up was 10.3 years (± 5.5, from 3 to 19.9 years). In the Megaprosthesis group, the mean age was 24.7 years old (± 5.5, from 18 to 33.4 years old) and the mean follow-up was 8.1 years (± 6.9, from 3 to 19.9 years). In the Allograft group, the mean age was 25.6 years old (± 5.5, from 18.5 to 35.9 years old) and the mean follow-up was 11.7 years (± 3, from 7.1 to 17.7 years).
Surgical procedure
Tumours were resected respecting a security margin of 2 cm, based on pre-operative MRI. Depending on the amount of remaining distal femur, patients underwent two different types of surgery. If the resection allowed keeping more than 2 cm above the knee joint, patients underwent a biologic reconstruction (Allograft group). The reconstruction was made using a massive allograft augmented with a vascularized fibula harvested from the same lower limb. The fibula was inserted into the medullary canal of the allograft. A cortical window allowed passage of the vessels. The fixation was made with a long 5-mm lateral customized plate that matched the length of resection (Medicalex, Bagneux, France). Depending on the amount of remaining epiphysis, the distal fixation was made using either screws or a blade (Fig. 1a).
a Radiographic images of a patient who underwent a massive distal femur reconstruction for an osteosarcoma of the right distal femur at 14 years old. A Pre-operative radiograph showing a lytic lesion of the distal metaphysis of the right femur. B Pre-operative MRI confirming that the epiphysis is not involved with the tumor. C Post-operative radiograph after tumor resection and reconstruction with a customized blade-plate, allograft and vascularized fibula. b Radiographic images of a male patient who underwent a total knee replacement for an osteosarcoma of the left distal femur. A Pre-operative radiograph showing a lytic lesion of the distal metaphysis and epiphysis of the left femur. B Pre-operative MRI confirming that the epiphysis is involved with the tumor. C Post-operative radiograph after tumor resection and total knee replacement with cemented megaprosthesis. With regards to tibial component, only the plateau was cemented
If the remaining epiphysis was too small, patients underwent a total knee replacement (Megaprosthesis group) after resection of the tumor. Reconstruction was made using a constrained megaprosthesis, with fixed hinge and a cemented stem in both femur and tibia (Medicalex, Bagneux, France) (Fig. 1b).
In our cohort, nine patients underwent Allograft and six underwent Megaprosthesis.
Data collection
Several demographic and radiographic parameters were collected, such as age, height, weight, limb length discrepancy and length of femur resection.
Each patient and control underwent a gait analysis. As described in the Plug-in-Gait protocol, each patient was equipped with 15 retroflective markers on the lower limbs and pelvis [11, 12]. The gait laboratory was equipped with six HiRes infrared cameras sampled at a frequency of 100 Hz, that were able to register the position of the retroflective markers during gait. Two force platforms were able to give information about ground reaction forces during gait. Patients were asked to walk at a self-selected speed on a 9-m walkway.
Several parameters were recorded. Spatiotemporal parameters included gait speed, stride length and cadence. Kinematics parameters included hip flexion extension, knee flexion extension and ankle flexion extension.
Analysis of gait cycles was made according to a previously published methodology [13]. The gait cycle was divided into Stance phase (initial contact, loading response, mid-stance and terminal stance) and Swing phase (initial, mid- and terminal swing) (Fig. 2).
A functional assessment based on the gait analysis was performed for every patient and control. This assessment was made by the Gait Deviation Index (GDI) [14] and the Gillette Gait Index (GGI) [15]. Global function was assessed by the Musculoskeletal Tumor Society Score (MSTS).
Statistical analysis
Data are presented as means, standard deviations and ranges. Comparisons were conducted between treatment groups; subsequently, each treatment group was compared to the control group. Different kinematic comparisons were performed: affected limb versus contralateral limb in each treatment group, kinematics of affected limb in each group versus control group and kinematics of contralateral limb in each group versus control group. Normality was tested by a Kolmogorov-Smirnov test. If the distribution was normal, Student T-tests were performed for the comparison of means. If not, Kruskall-Wallis tests were used. Values below 5% were considered as statistically significant (i.e. p < 0.005).
Results
Spatiotemporal parameters
The results of spatiotemporal parameters in the three groups and their comparison are presented in Table 2. Cadence was not different between the allograft and the megaprosthesis groups (105 vs 99 steps/min, p = 0.192), as well as walking speed (1.03 vs 1.01, p = 0.658), step length (0.58 vs 0.61 m, p = 0.293) and stride length (1.18 vs 1.23, p = 0.348). When compared to controls, patients of the two treatment groups had significantly lower cadence, walking speed, step and stride lengths.
Allograft versus megaprosthesis (Fig. 3)
Immediately preceding toe off, there was a significant decrease in knee flexion at terminal stance in Megaprosthesis patients. Otherwise, knee kinematics were not significantly different between the two treatment groups. Knee kinetics, GGI and GDI, did not show any significant difference between the two groups. With regards to the MSTS, it was 81.1% (± 9.7, from 66.7 to 96.7%) in the Allograft group and 79.4% (± 10.2, from 70 to 96.7%) in the Megaprosthesis group. This difference was not statistically significant (81.1% vs 79.4%, p = 0.758).
Allograft versus controls (Fig. 4)
With respect to the affected limb, there was a decrease of knee flexion at loading response during the early stage of stance phase. Of note, there was no significant difference in maximum knee flexion during initial swing (toe clearance from the floor). This gait pattern with a less extended knee led to a decrease in knee moment during the loading response and a decrease in knee power. The contralateral limb showed a slight decrease in knee extension before heel strike (terminal swing). There was no major change in contralateral knee kinetics.
The results of the GDI and GGI scores and the statistical comparison are presented in Table 3. As expected, Allograft patients had significantly worse scores than controls with regards to every parameter.
Megaprosthesis versus controls (Fig. 5)
With respect to the affected limb, gait analysis showed significant changes in knee kinematics. Knee flexion was significantly lower within the Megaprosthesis patients throughout stance phase. The loading response (0–15% of gait cycle) was significantly lower (less knee flexion) in Megaprosthesis patients than in controls. At heel rise (terminal stance, 40-50% of gait cycle), knee flexion was lower in Megaprosthesis patients. The compensatory mechanisms were also greater when looking at the contralateral limb. There was a significant decrease in knee flexion during the late stance phase and the initial swing phase. The results of the statistical comparison of GDI and GGI are presented in Table 3.
Discussion
Our study aimed to compare knee motion in Megaprosthesis and Allograft patients after limb salvage surgery for malignant bone tumor. Despite the small sample of patients, we were able to highlight differences between treatment groups. The present study is one of the first comparing these two techniques for the treatment of distal femur malignancies (Table 4).
The comparison between the two treatment groups revealed that there were only few differences in knee kinematics and kinetics. Megaprosthesis patients had a more extended knee throughout stance phase but this difference was not significant except at terminal stance (50%), where Megaprosthesis patients had a decreased knee flexion when compared to Allograft patients. Otherwise, spatiotemporal parameters and functional scores were not significantly different in the two groups. These results are of primary interest as they suggest that there is no superiority of one technique over the other in terms of gait function. Moreover, both groups showed good results in terms of MSTS, suggesting that at long-term, both techniques provide good functional results.
Epiphysis-sparing reconstruction using Allograft gives satisfactory results. In a recent study, Aponte-Tinao et al. reported 86% survival rate at five and ten years. Using the Musculoskeletal Tumor Society scoring system, they reported an average score of 26 points out of 30 at last follow-up (86%, at >10 years) [16]. Our results are in line, with a mean score of 81.1%. However, this kind of evaluation is necessarily contingent upon subjective data. To our knowledge, our series is the first to compare the results of such reconstructions to a control population using gait analysis. Our results suggest that there were very few changes in gait kinematics and kinetics in patients undergoing this kind of surgery. Kinematics revealed a decreased knee flexion during loading response. In addition, several spatiotemporal parameters, such as walking speed, were significantly decreased.
With respect to the gait of the contralateral limb, there was a decrease in knee flexion during terminal swing. Such a decrease may be explained by variation in limb length as previously reported by Okita et al. [2]. We noted a similar increase in power during the end of stance phase that may be reflective of the contralateral limb bearing an increased load in order to compensate for the weakness in the affected limb.
The results of the functional assessment revealed that GDI and GGI scores were significantly worse in Allograft patients than in controls (85.5 vs 94 and 53.8 vs 38.9, respectively, all p < 0.05). However for the GDI, the minimal difference to detect clinical changes was reported to be 9.4 by Correa et al. [17]. In our series, the difference between Allograft patients and controls was 8.5. We can therefore guess that this difference, even if statistically significant, was not clinically relevant.
The gait pattern in Megaprosthesis patients showed more differences when compared to control group. There was a clear decrease in knee flexion throughout stance phase. This change in kinematics led to a corresponding decrease in both knee moment and knee power which accords with the literature [3, 4]. Additionally, a similar change in knee flexion was reported in a previous study of megaprosthesis patients that underwent resection of the promial tibia [18]. This pattern is typical of patients with quadriceps weakness or extensor apparatus dysfunction [19]. During loading response, the quadriceps works eccentrically in order to control knee flexion. If the quadriceps is not strong enough, hip extensors will compensate by bringing the lower limb into a more extended position in order to provide mechanical stability. Thus, as several authors have previously reported, hyperextension appears to be a compensatory mechanism to secure stance phase [20, 21]. In patients undergoing resection of a bone tumor at the distal femur, damage to the quadriceps and the extensor apparatus is unavoidable. Consequently, this gait pattern primarily represents soft tissue damage, rather than joint stiffness stemming from the prosthesis itself. In 1991, Capanna et al. have published a classification based on the amount of bone and soft tissue resection [6]. They found a clear relationship between inadequate extensors power and functional impairment.
Gait changes and its influence on the forces applied to the knee joint have been widely reported. However, authors mainly reported changes in the frontal plane [22]. In our patients, changes occurred in the sagittal plane with a decrease of flexion throughout stance phase. These changes in kinematics lead to an increase of the extension moment between 20 and 50% of the gait cycle. This moment is directly applied on the hinge of the prosthesis, as it is the main structure to retain the knee from hyperextension. Thus this particular gait pattern may jeopardize prosthesis survival. To our knowledge, this hypothesis has not been investigated; however, given the clear clinical implication further research should investigate the potential correlation of prosthesis wear and a knee hyperextension gait pattern.
The contralateral limb showed abnormal gait as well. There was a decrease in knee flexion during the late stance phase. This stage corresponds to the affected limb loading response. Thus, the decrease in knee flexion is the consequence of the affected knee hyperextension during loading response. The limb length discrepancy may also play a role in this particular pattern. These results are consistent with previously reported results by Okida et al. [2].
Interestingly, only the GDI score of the affected limb was significantly worse than controls. Demonstrating that, despite changes in gait patterns, patients undergoing Megaprosthesis after bone tumor retain satisfactory function of the lower limb.
This study has several limitations, mainly due to the nature of the disease. First of all, our study samples were very small (9 and 6 patients in Allograft and Megaprosthesis groups, respectively). As such, our small sample size may lead to a low statistical power. This may account for our inability to highlight differences between the two treatment groups. Although it is difficult to obtain gait data in these patients, we were able to obtain such data in 15 patients with a mean follow-up of eight and 12 years, respectively. This is one of the largest series ever published with such a long follow-up. However, it is still likely that, in terms of gait, no difference exists between these two different limb salvage techniques.
Second, the comparison between the two treatments groups is potentially biased, as the indications are not the same. However, the objective of our study was not to promote one technique over another, but to analyze the differences in gait patterns.
Finally, we found that gait changes are mainly due to soft tissue damage that occurred during surgery. It would have been of great interest to follow Capanna’s classification in our study. Unfortunately, the retrospective design of our study precludes having sufficient data about the exact amount of resection, especially on soft tissues. However, the small sample size does not allow performing statistical comparisons. Stratification by amount of soft tissue damage would lead to comparisons between groups of three or four patients. The low power of such statistical comparisons would probably lead to misleading conclusions. Anyway, a larger series could allow drawing conclusions from this type of information and thus be of major interest.
Some clinical implications can be drawn from our results: it is crucial to preserve as much extensor mass as possible when performing such surgical procedures. If too much muscle damages are needed to remove the tumor, the extensor apparatus must be reconstructed by any means possible.
Conclusion
This is one of the largest series reporting the objective functional results of two techniques of limb salvage surgery after a malignant bone tumor. With gait analysis, we found that both Megaprosthesis and biologic reconstruction with allografts provide good results in the long-term and minimal gait impairment. Our study suggests that no difference exist in terms of gait when comparing these two techniques. We were able to shed light on the changes that occur after such surgery. Both Allograft and Megaprosthesis patients showed a more extended knee during stance phase, likely due to the soft tissue damages secondary to the surgery. These modifications in kinetics and kinematics of the knee had an impact on spatiotemporal parameters, with a decreased walking speed and step length. However, patients were able to have an efficient walk, as demonstrated by the results of the GDI and GGI scores.
The particular gait patterns reported in this study suggest that gait changes may be mainly due to muscle resection. In order to reduce changes in gait pattern, it thus may be crucial to focus on postoperative rehabilitation. By improving quadriceps strength and knee proprioception, it is possible that differences in gait would disappear in both affected and contralateral limbs.
Knee hyperextension during stance phase leads to an increase in extension moment that applies to the joint. In tumour surgery around the knee, especially in patients with a megaprosthetic reconstruction, this knee hyperextension is achieved with the motion of the prosthesis and it is very important for the patients to lock the knee in extension while walking. These patients have a typical gait pattern with knee hyperextension, even if they do not necessarily have complete active extension (because of defect or improper reattachment of the extensor mechanism). Further studies could be of major interest, in order to correlate the changes in gait pattern to cartilage or prosthesis wear.
Even if differences with the control group were greater in Megaprosthesis patients, there were very few differences between the two treatment groups. However, larger samples are necessary in order to highlight differences.
References
Schrager J, Patzer RE, Mink PJ et al (2011) Survival outcomes of pediatric osteosarcoma and Ewing’s sarcoma: a comparison of surgery type within the SEER database, 1988-2007. J Registry Manag 38:153–161
Okita Y, Tatematsu N, Nagai K et al (2013) Compensation by nonoperated joints in the lower limbs during walking after endoprosthetic knee replacement following bone tumor resection. Clin Biomech (Bristol, Avon) 28:898–903. https://doi.org/10.1016/j.clinbiomech.2013.08.005
Bruns J, Raabe K, Deuretzbacher G (2016) Gait analysis in tumor patients after distal femoral resection and implantation of a megaprosthesis. Acta Orthop Belg 82:287–297
Carty CP, Bennett MB, Dickinson IC, Steadman P (2009) Assessment of kinematic and kinetic patterns following limb salvage procedures for bone sarcoma. Gait Posture 30:547–551. https://doi.org/10.1016/j.gaitpost.2009.08.234
Carty CP, Dickinson IC, Watts MC et al (2009) Impairment and disability following limb salvage procedures for bone sarcoma. Knee 16:405–408. https://doi.org/10.1016/j.knee.2009.02.006
Capanna R, Ruggieri P, Biagini R et al (1991) The effect of quadriceps excision on functional results after distal femoral resection and prosthetic replacement of bone tumors. Clin Orthop Relat Res:186–196
Saunders J, Inman VT, Eberhart H (1953) The major determinants in normal and pathological gait. J Bone Joint Surg Am 35:543–558
Riley PO, Paolini G, Della Croce U et al (2007) A kinematic and kinetic comparison of overground and treadmill walking in healthy subjects. Gait Posture 26:17–24. https://doi.org/10.1016/j.gaitpost.2006.07.003
Kainz H, Graham D, Edwards J et al (2017) Reliability of four models for clinical gait analysis. Gait Posture 54:325–331. https://doi.org/10.1016/j.gaitpost.2017.04.001
Ollivier M, Parratte S, Lunebourg A et al (2016) The John Insall award: no functional benefit after unicompartmental knee arthroplasty performed with patient-specific instrumentation: a randomized trial. Clin Orthop Relat Res 474:60–68. https://doi.org/10.1007/s11999-015-4259-0
Kadaba MP, Ramakrishnan HK, Wootten ME (1990) Measurement of lower extremity kinematics during level walking. J Orthop Res 8:383–392. https://doi.org/10.1002/jor.1100080310
Davis RB, Õunpuu S, Tyburski D, Gage JR (1991) A gait analysis data collection and reduction technique. Hum Mov Sci 10:575–587. https://doi.org/10.1016/0167-9457(91)90046-Z
Loudon J, Swift M, Bell S (2008) The clinical orthopedic assessment guide. The Clinical Orthopedic Assessment Guide, 2nd edition. Human Kinetics, pp 395–408
Schwartz MH, Rozumalski A (2008) The gait deviation index: a new comprehensive index of gait pathology. Gait Posture 28:351–357. https://doi.org/10.1016/j.gaitpost.2008.05.001
Schutte LM, Narayanan U, Stout JL et al (2000) An index for quantifying deviations from normal gait. Gait Posture 11:25–31
Aponte-Tinao L, Ayerza MA, Muscolo DL, Farfalli GL (2015) Survival, recurrence, and function after epiphyseal preservation and allograft reconstruction in osteosarcoma of the knee. Clin Orthop Relat Res 473:1789–1796. https://doi.org/10.1007/s11999-014-4028-5
Correa KP, Devetak GF, Martello SK et al (2017) Reliability and minimum detectable change of the gait deviation index (GDI) in post-stroke patients. Gait Posture 53:29–34. https://doi.org/10.1016/j.gaitpost.2016.12.012
Colangeli M, Donati D, Benedetti MG et al (2007) Total knee replacement versus osteochondral allograft in proximal tibia bone tumours. Int Orthop 31:823–829. https://doi.org/10.1007/s00264-006-0256-y
Perry J (1990) Pathologic gait. Instr Course Lect 39:325–331
Benedetti MG, Bonatti E, Malfitano C, Donati D (2013) Comparison of allograft-prosthetic composite reconstruction and modular prosthetic replacement in proximal femur bone tumors: functional assessment by gait analysis in 20 patients. Acta Orthop 84:218–223. https://doi.org/10.3109/17453674.2013.773119
Rompen JC, Ham SJ, Halbertsma JPK, van Horn JR (2002) Gait and function in patients with a femoral endoprosthesis after tumor resection: 18 patients evaluated 12 years after surgery. Acta Orthop Scand 73:439–446. https://doi.org/10.1080/00016470216319
D’Lima DD, Fregly BJ, Patil S et al (2012) Knee joint forces: prediction, measurement, and significance. Proc Inst Mech Eng Part H J Eng Med 226:95–102. https://doi.org/10.1177/0954411911433372
Acknowledgements
Authors declare no conflict of interest regarding this article.
SP received a grant from SOFCOT, SOFOP and ADEREM for this work
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pesenti, S., Peltier, E., Pomero, V. et al. Knee function after limb salvage surgery for malignant bone tumor: comparison of megaprosthesis and distal femur allograft with epiphysis sparing. International Orthopaedics (SICOT) 42, 427–436 (2018). https://doi.org/10.1007/s00264-017-3608-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3608-x