Abstract
Purpose
This study reports a case series of 44 primary total knee arthroplasties (TKAs) using autogenous morcellised bone grafting for large (≥10-mm-deep) medial tibial defects, which are generally repaired using metal augmentation. The bone-grafting technique is described in detail and the radiological outcomes are presented.
Methods
A total of 44 TKAs were followed up for a mean period of 58 months (range 24–139 months). Multiple drill holes were made in the sclerotic floor of the defect, followed by the impaction of morcellised cancellous bone grafts to fill the defects. Tibial components were fixed using the cemented or noncemented technique and no internal fixation devices were used. Stem extension of the tibial component was only used in one TKA.
Results
Radiograms revealed that the grafted bone was completely incorporated into the host bone within one year post-operatively. No grafted bone absorption or collapse was detected. A clear zone between the tibial component and grafted bone was observed in six knees, but it did not become enlarged thereafter.
Conclusions
The presented technique provided favourable radiological outcomes and had several advantages: (1) it enables preservation of as much bone as possible for future revision surgery; (2) it is cost effective and simple because metal augments, internal fixation devices and stem extension are not needed; (3) it can be used in the same manner any defect to a depth ≥3 mm. Thus, this is an acceptable and reproducible alternative technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) provides favourable long-term outcomes [1–4]; however, managing bone defects in primary TKA is still challenging. Various methods have been reported for managing medial tibial defects in primary or revision TKA, such as filling with bone cement [5, 6], autogenous [7–11] or allogenous [12, 13] block bone grafting and metal augmentation [14–18]. Generally, a defect depth of <5 mm should be filled with bone cement, that of 5–10 mm with bone grafts and that of >10 mm with metal augmentation, as Vail et al. [19] indicated in their textbook. In this study, we report a case series of 44 TKAs in which we used autogenous morcellised bone grafting for large (≥10-mm-deep) medial tibial defects. This study aimed to describe this bone-grafting technique in detail and to analyse its radiological outcomes retrospectively.
Materials and methods
The study protocol was approved by the Institutional Review Board of our clinic. Written informed consent was obtained from all patients. During June 2003 to April 2014, 47 TKAs in 45 patients were performed using the following presented bone-grafting technique. One patient (one TKA) died, and two patients (two TKAs) were lost before the two year follow-up evaluation. Thus, a total of 44 TKAs (42 patients) were followed up for a mean period of 59 months (range 24–139 months). Eight patients were men (nine TKAs), and 34 were women (35 TKAs); mean age at surgery was 73.9 years (range 56–85 years). Pre-operative diagnoses were osteoarthritis (n = 33), rheumatoid arthritis (n = 3), osteonecrosis of the medial tibial condyle (7) and Charcot’s joint (n = 1). Implants were from LCS (Depuy, Warsaw, IN, USA), Profix (Smith & Nephew, Memphis, TN, USA), Magna-ROM 21 (Centerpulse, Austin, TX, USA), Genesis II (Smith & Nephew) and NexGen (Zimmer) in 1, 2, 5, 10 and 26 TKAs, respectively. All TKAs were performed by a single surgeon (TS). Defect type according to Dorr’s classification [10] was central in one knee and peripheral in 43 and according to Watanabe’s classification [20] flat peripheral in 12 and slant peripheral in 31 (Fig. 1). Mean depth (n = 44), mediolateral width (n = 40) and anteroposterior width (n = 40) of the medial tibial defect measured after the horizontal osteotomy of the tibial articular surface were 12.3 mm (range 10–23 mm), 17.5 mm (range 10–26 mm) and 36.9 mm (range 30–45 mm), respectively.
Defect classification according to Watanabe [20] (black arrows): a flat peripheral and b slant peripheral types
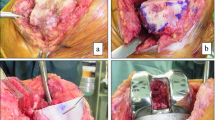
Figure 2 shows the the grafting technique used in this study. Multiple drill holes were made in the sclerotic floor of the defect to promote vascularity beneath the floor (Fig. 2a). Morcellised cancellous bone was obtained from the resected femoral and tibial subchondral bones. To prevent bone cement from entering the space between the graft and tibial host bed, grafts were firmly impacted using a metal bar and manual pressure. An assistant’s index finger was used as a bank during impaction to prevent the grafted bone from crumbling (Fig. 2b and c). Tibial components were fixed similarly (Fig. 2d). No internal fixation devices were used, and extension of the tibial stem was used in only one knee (with Charcot’s joint).
Bone-grafting technique: a Multiple drill holes on the sclerotic floor of the defect. b, c Morcellised cancellous bone grafts firmly impacted using a metal bar and manual pressure. During impaction, an assistant’s index finger (asterisk) was used as a bank to prevent grafted bone from crumbling. d Tibial component fixed using bone cement
Partial weight-bearing was allowed four to five days after surgery. Full weight bearing was allowed after one to two weeks in most patients.
Results
Patient demographic data and radiological outcomes are summarised in Table 1. Post-operative radiological changes in the grafted bone are shown in Fig. 3. In general, the grafted bone exhibited osteosclerotic changes two to three months post-operatively (Fig. 3a). Subsequently, the grafted bone became less dense, and bony trabeculae were detected (Fig. 3b). Finally, the grafted bone was completely incorporated into the host bone, with bony trabeculae crossing the interface within one year post-operatively (Fig. 3c). No absorption or collapse of the grafted bone was detected; trabeculae were observed in all knees. A clear zone between the tibial component and grafted bone was observed in six knees, but it did not enlarge thereafter. The margin of the grafted area represented a sclerotic line similar to a bony cortex in 32 TKAs (72.7%) (Fig. 4).
Discussion
The most important finding of this study is that radiological outcomes after autogenous morcellised bone graft for large medial tibial defects in primary TKA were favourable. Grafted bone was completely incorporated into host bone without absorption or collapse within one year post-operatively. Various methods to manage medial tibial defects in primary or revision TKA [5–18] have been reported. Vail et al. [19] recommended method selection based on defect depths. Panegrossi et al. [21] stated that the choice between different surgical options depended on defect dimension, bone quality and patient’s quality of life. Lotke et al. [5] and Ritter et al. [6] reported favourable results using methylmethacrylate for large tibial defects in primary TKA. Favourable clinical and/or radiological results using metal augmentation have also been reported by several authors [14–18]. However, using both bone cement and metal augmentation is more disadvantageous than autogenous or allogenous bone graft for preserving bone stock. The bone–implant interface in knees with metal augmentation forms a complex shape, which creates continuing concern regarding implant loosening. Rawlinson et al. [22] used cadaver knees to biomechanically confirm that the use of a tibial stem reduced bone stress and limited micromotion between the metal wedge and surrounding bone; they recommended using a tibial stem. When a tibial stem is used, additional concern regarding any further loss in bone stock will occur during revision surgery.
For preserving bone stock, an autogenous or allogenous bone graft has been well established as being superior to bone cement and metal augmentation. Many authors reported favourable results following an autogenous block bone graft in primary TKA [7–11]. However, it is difficult to obtain a bone block ≥10-mm thick from a resected femoral or tibial bone. Internal fixation devices were used for these block bone grafts. Moreover, Mullaji et al. [11] used a tibial stem extender when bone grafting was performed for defects ≥10 mm. An allogenous block bone graft was used primarily for revision TKA [12, 13]. For both autogenous and allogenous block bone grafting, additional bone cuts in the defect and a block bone to adjust for shape are required. However, some authors used autogenous morcellised bone [20, 23, 24]. Watanabe et al. [20] reported five TKAs with slant peripheral defects using two bones resected from the femoral condyle. They were driven like pegs into two gutters created on the floor of the tibial defect, with bone chips impacted around the pegs. Kharbanda et al. [23] reported six TKAs with larger bone defects (>25-mm deep) using morcellised impaction autograft supported by wire mesh fixed with screws, as well as tibial stem extenders.
We previously reported our experience using two bone-grafting techniques: (1) Two resected subchondral bone plates from the lateral tibial plateau were driven into two gutters made on the floor of the medial tibial defects to create bony support posts, and morcellised cancellous bone was impacted around the posts (in 19 TKAs); (2) Morcellised cancellous bone was impacted to fill the defect (in 26 TKAs) [24]. Internal fixation devices, metal mesh support and stem extender were not used in our procedures. We further reported that remodeling of grafted bone was faster in the latter 26 TKAs than in the former 19 procedures. Accordingly, 44 TKAs using only morcellised cancellous bone impaction were assessed in the study we report here.
This study revealed that our technique has several advantages over others: Firstly, as much bone as possible can be preserved for future revision surgery. Moreover, the bone–implant interface in knees with metal augmentation forms a complex shape, causing continuing concern regarding implant loosening. Thus, this technique can be considered for patients undergoing standard TKA without bone graft, as trabeculae were clearly depicted on radiograms after a maximum of one year. In addition, this technique provides a “biologic reconstruction” and “physiologic load transfer,” as described by Hanna et al. [25]. Secondly, this technique is cost effective and simple to perform, because metal augments, internal fixation devices, mesh supports and stem extenders are not required. Toms et al. [26] experimentally revealed that if support of rim of defects was sufficient or if a long stem was used, an impacted morcellised bone graft achieved adequate initial stability. However, we discovered that a morcellised bone graft for a slant peripheral defect without a wire mesh supporter and a stem extender demonstrated favourable radiological outcomes. We believe the medial soft tissue wall plays a role in preventing the grafted bone from crumbling after surgery. Thirdly, autogenous morcellised bone grafts can be used for any defect ≥3-mm depth in the same manner without any special preparation. In contrast, additional bone cuts are required in order to adjust defect shape to the metal augmentations or block bone.
A relatively short follow-up period and a small number of patients represent limitations. Because knees undergoing TKA with a bone graft could be considered similar to standard TKA without a bone graft, and because trabeculae were clearly depicted on radiograms after a maximum of one year, a minimum of a two year follow-up period following a morcellised cancellous bone graft, as in this study, could be sufficient. Because only 47 (4.9%) of 967 TKAs during June 2003–April 2014 had a medial tibial defect of ≥10-mm depth, such defects can be considered rare. The number of patients reported by Ahmed at al. for an autogenous block bone graft in primary TKA [8] and by Lee et al. for a metal augmentation in primary TKA [16] was 18 and 46, respectively. Another limitation is that no clinical data were reported. Although a single surgeon (TS) performed all TKAs, some were performed at different hospitals as invited surgeries. Because the clinical evaluation scales differed among hospitals, the same clinical scoring data could not be collected. Accordingly, only radiological outcomes were focused on in this study.
Conclusion
Because this bone-grafting technique provided favourable radiological outcomes and had some advantages compared with metal augmentation, block bone grafting or filling with bone cement, it can be considered an acceptable and reproducible alternative to those procedures.
References
Callaghan JJ, Wells CW, Liu SS, Goetz DD, Johnston RC (2010) Cemented rotating-platform total knee replacement: a concise follow-up, at a minimum of twenty years, of a previous report. J Bone Joint Surg Am 92(7):1635–1639
Gill GS, Joshi AB, Mills DM (1999) Total condylar knee arthroplasty: 16- to 21- year results. Clin Orthop Relat Res 367:210–215
Ranawat CS, Flynn WF Jr, Saddler S, Hansraj KK, Maynard MJ (1993) Long-term results of the total condylar knee arthroplasty: a 15-year survivorship study. Clin Orthop Relat Res 286:94–102
Victor J, Ghijselings S, Tajdar F, Van Damme G, Deprez P, Arnout N, Van Der Straeten C (2014) Total knee arthroplasty at 15–17 years: does implant design affect outcome? Int Orthop 38(2):235–241
Lotke PA, Wong RY, Ecker ML (1991) The use of methylmethacrylate in primary total knee replacements with large tibial defects. Clin Orthop Relat Res 270:288–294
Ritter MA, Keating EM, Faris PM (1993) Screw and cement fixation of large defects in total knee arthroplasty: a sequel. J Arthroplasty 8(1):63–65
Aglietti P, Buzzi R, Scrobe F (1991) Autologous bone grafting for medial tibial defects in total knee arthroplasty. J Arthroplasty 6(4):287–294
Ahmed I, Logan M, Alipour F, Dashti H, Hadden WA (2008) Autogenous bone grafting of uncontained bony defects of tibia during total knee arthroplasty: a 10-year follow up. J Arthroplasty 23(5):744–750
Altchek D, Sculco TP, Rawlins B (1989) Autogenous bone grafting for severe angular deformity in total knee arthroplasty. J Arthroplasty 4(2):151–155
Dorr LD, Ranawat CS, Sculco TA, McKaskill B, Orisek BS (1986) Bone graft for tibial defects in total knee arthroplasty. Clin Orthop Relat Res 205:153–165
Mullaji AB, Padmanabhan V, Jindal G (2005) Total knee arthroplasty for profound varus deformity: technique and radiological results in 173 knees with varus of more than 20°. J Arthroplasty 20(5):550–561
Engh GA, Herzwurm PJ, Parks NL (1997) Treatment of major defects of bone with bulk allografts and stemmed components during total knee arthroplasty. J Bone Joint Surg Am 79(7):1030–1039
Harris AI, Poddar S, Gitelis S, Sheinkop MB, Rosenberg AG (1995) Arthroplasty with a composite of an allograft and a prosthesis for knees with severe deficiency of bone. J Bone Joint Surg Am 77(3):373–386
Brand MG, Daley R, Ewald FC, Scott RD (1989) Tibial tray augmentation with modular metal wedges for tibial bone stock deficiency. Clin Orthop Relat Res 248:71–79
Hamai S, Miyahara H, Esaki Y, Hirata G, Terada K, Kobara N, Miyazaki K, Senju T, Iwamoto Y (2015) Mid-term clinical results of primary total knee arthroplasty using metal block augmentation and stem extension in patients with rheumatoid arthritis. BMC Musculoskelet Disord 16:225–230. doi:10.1186/s12891-015-0689-9
Lee JK, Choi CH (2011) Management of tibial bone defects with metal augmentation in primary total knee replacement: a minimum five-year review. J Bone Joint Surg (Br) 93(11):1493–1496
Pagnano MW, Trousdale RT, Rand JA (1995) Tibial wedge augmentation for bone deficiency in total knee arthroplasty: a followup study. Clin Orthop Relat Res 321:151–155
Tsukada S, Wakui M, Matsueda M (2013) Metal block augmentation for bone defects of the medial tibia during primary total knee arthroplasty. J Orthop Surg Res 8:36–41. doi:10.1186/1749-799X-8-36
Vail TP, Lang JE, Sikes CV (2012) Surgical techniques and instrumentation in total knee arthroplasty. In: Scott WN (ed) Insall & Scott surgery of the knee, 5th edn. Churchill Livingstone, New York, pp 1042–1099
Watanabe W, Sato K, Itoi E (2001) Autologous bone grafting without screw fixation for tibial defects in total knee arthroplasty. J Orthop Sci 6(6):481–486
Panegrossi G, Ceretti M, Papalia M, Casella F, Favetti F, Falez F (2014) Bone loss management in total knee revision surgery. Int Orthop 38(2):419–427
Rawlinson JJ, Closkey RF Jr, Davis N, Wright TM, Windtsor R (2008) Stemmed implants improve stability in augmented constrained condylar knees. Clin Orthop Relat Res 466:2639–2643
Kharbanda Y, Sharma M (2014) Autograft reconstructions for bone defects in primary total knee replacement in severe varus knees. Indian J Orthop 48(3):313–318
Sugita T, Aizawa T, Sasaki A, Miyatake N, Fujisawa H, Kamimura M (2015) Autologous morselised bone grafting for medial tibial defects in total knee arthroplasty. J Orthop Surg 23(2):185–189
Hanna SA, Aston WJS, de Roeck NJ, Gough-Palmer A, Powles DP (2011) Cementless revision TKA with bone grafting of osseous defects restores bone stock with a low revision rate at 4 to 10 years. Clin Orthop Relat Res 469:3164–3171
Toms AD, McClelland D, Chua L, de Waal Malefijt M, Verdonschot N, Jones RS, Kuiper J-H (2005) Mechanical testing of impaction bone grafting in the tibia: initial stability and design of the stem. J Bone Joint Surg (Br) 87(5):656–663
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
Not required.
Informed consent
Informed consent was obtained from all participants.
Rights and permissions
About this article
Cite this article
Sugita, T., Aizawa, T., Miyatake, N. et al. Preliminary results of managing large medial tibial defects in primary total knee arthroplasty: autogenous morcellised bone graft. International Orthopaedics (SICOT) 41, 931–937 (2017). https://doi.org/10.1007/s00264-016-3339-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3339-4