Abstract
Bone loss is frequently encountered in severely deformed knees undergoing a total knee arthroplasty. Contained defects can be filled with morselized autograft. Large uncontained postero-medial defects in proximal tibia seen in varus knees can be addressed using cement, cement with screw augmentation, autografting, structural allografts, impaction bone grafting, metal augments and metaphyseal sleeves. The aim of reconstruction is to provide a stable bone bed for implantation of prosthesis, to restore the joint line and preserve bone for future revisions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Bone defects encountered in primary total knee arthroplasty are commonly observed in severe deformities. As the severity of osteoarthritis increases, the varus deformity progressively causes the bone on the postero-medial aspect of tibia to get eburnated creating a bone defect. It is usually the opposite in a valgus knee where the deforming force causes a progressive wear of the lateral femoral condyle and sometimes the postero-lateral proximal tibia (contained defect). Bone loss observed in primary total knee arthroplasty can be due to bone cysts, inflammatory arthritis, previous malunited fractures, osteonecrosis and previous osteotomies. These defects are a challenge to the operating surgeon because for a prosthesis to be stable and positioned in a good coronal alignment, you need a healthy stable bone bed. Resecting more bone (12 mm beyond tibial plateau) is not a favourable option as it compromises the attachment of collateral ligaments, iliotibial band and patellar tendon. Moreover, the quality of bone decreases as we go into the metaphysis. There are multiple options to address these defects depending upon their size and location. The principles guiding the management of these bone defects are based upon the location, size, depth of defects and percentage involvement of bone loss in the tibial or femoral condyles. Other considerations taken into account while dealing with these bone defects are the ligament stability, age, activity and life expectancy of the patient. This chapter deals with the intricacies of bone defect management in such a complex primary situation.
2 Classification
Bone defects can mainly be classified into contained and uncontained (peripheral) defects [1]. Contained defects with bone all around can simply be filled with morselized bone grafts obtained from bone chamfers during the process of total knee replacement (Fig. 14.1a, b). The uncontained defects are commonly seen in severe varus knees on the postero-medial aspect of proximal tibia. These are usually addressed depending upon their size, depth and percent involvement of tibial condyle. In contrast, the defects seen in proximal tibia in a valgus knee are centrally located (essentially contained). Rand in 1991 classified the defects based upon the percentage involvement of tibial plateau and depth of defect [2] (Table 14.1).
The most useful and frequently used classification is the Anderson Orthopedic Research Institute (AORI) Classification. This mainly classifies defects based upon the involvement of metaphysis and is subclassified based on single/both plateau involvement. It is mainly described for severity of bone loss in revision knee arthroplasty but stands true for bone loss in primary situations as well [3] (Table 14.2).
3 Management of Bone Defects
The defect can be reduced by the following means:
-
(a)
Lateralizing the tibial component
-
(b)
Undersizing the tibial component
-
(c)
Cutting more than usual (8 mm) of proximal tibia (maximum acceptable is 12 mm) to reduce the defect.
The main options available to reconstruct the remaining defect are
-
1.
Cementoplasty
-
2.
Cement with screw augmentation
-
3.
Autograft reconstruction
-
4.
Impaction bone grafting
-
5.
Structural Allograft
-
6.
Metal Augments
Aim:
-
1.
To build up the defect
-
2.
Axial implantation in neutral alignment over good base of bone
-
3.
Restoration of joint line
-
4.
Conserve bone for future revisions
4 Pre-Operative Planning
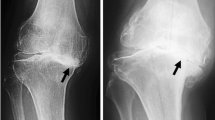
Standard weight bearing anteroposterior (AP) X-rays of knee joints are advised. The AP view (Fig. 14.2a) shows the defect in the medial proximal tibia and the amount of varus. The lateral view (Fig. 14.2b) helps in delineating the defect which is seen as a crater. The radiographs may underestimate the size of bone defects and so final assessment of bone loss is always done intra-operatively. CT Scans may be warranted for actual and detailed assessment. An MRI scan may be warranted in extreme deformities to assess the condition of collateral ligaments. During pre-operative clinical examination it is necessary to assess whether the deformity is correctable or not on a valgus stress and assess the amount of fixed flexion deformity.
5 Surgical Considerations
After a standard para patellar midline exposure, make sure that the initial release of medial soft tissue sleeve is done sequentially and in a staggered way, regularly checking the opening of the medial joint space. The proximal tibial cut has to be very conservative, may be <8 mm (Fig. 14.3a, b). The tibial base plate preparation has to be lateralized as much as possible, without any lateral overhang and a reduction osteotomy can be performed (this helps in reducing the size of the defect and balancing the varus deformity). Another option is to downsize the tibial plate. The residual defect is measured and quantified in mm and as a percentage of the proximal tibial condyle and can be managed in the following manner.
-
1.
Cementoplasty: for defects <5 mm, simply filling the defects with bone cement [4].
-
2.
Cement and screw augmentation: should be used in defects 5 mm deep and <25% of tibial condyle. The cement mantle can break under load if the thickness is more than 5 mm, so it is reinforced with a 3.5 mm cortical screw (it is similar to the concrete being reinforced using an iron frame).
-
3.
Bone grafts: Bone grafts are available from the cut proximal tibia and distal femur during primary total knee arthroplasty. They are both osteoinductive and osteoconductive. Autografts are preferred to fill defects which are >5 mm in depth (range 5–25 mm) and 25–40% of cut surface of the tibial condyle [5]. The defect is denuded of any residual cartilage and the base of defect is drilled with a 2 mm drill to make the sclerotic bone to bleed (Fig. 14.3c). This helps in graft incorporation. Autograft available from the cut proximal tibial and distal femur is prepared according to the technique described by Windsor et al. [6]. Similar technique has been described by Dorr, Ranawat, and Sulco et al. [7]. The bone is placed onto the raw defect and stabilised with cortical screws (Fig. 14.4a–c). The tibia implant is prepared in a standard fashion. A stem extender is recommended to protect the graft if the keel of the implant is cutting into the defect (Fig. 14.5c). A ‘step cut technique’ has also been described where the defect is fashioned into a step cut and bone graft is fixed using screws as described in the previous technique [8]. Autograft is the best cost-effective option for such defects as it is readily available, preserves bone for future revisions and incorporates well. There can be multiple reasons for failure of graft incorporation like varus alignment, avascular host bed, incomplete coverage of graft by tibial component, inadequate compression at graft bone junction and cement interposition between proximal tibia and graft causing failure of graft to incorporate.
-
4.
Impaction bone grafting: Lonner initially and then Lotke have described the use of impaction bone grafting along with a mesh for use in revision total knee replacement [9, 10]. Impaction bone graft (auto/allograft) is used to fill in large vertically oriented defects measuring >25 mm in depth and involving >40% of cut surface of tibial condyle. The defect is prepared in a standard way and a v-shaped stainless steel mesh (stryker) is fixed with cortical screws to stabilise the mesh (Fig. 14.6a). Now the contained defect is filled with morselized autograft obtained from the bone cuts. The recommended size of grafts is 5–7 mm and they are impacted in a cobblestone manner to obtain stability (Fig. 14.6b, c). This construct is always stabilised with a stem on the tibial side (Fig. 14.7a, b) [5].
-
5.
Structural Allograft: The need to use allografts rarely arises in primary situations, as autografts are readily available from the bone cuts obtained during primary knee arthroplasty. Structural allograft like a femoral head can be fashioned to fill the defect in a similar manner as described for autografts and stabilised with screws or can be mixed with autograft and used for impaction bone grafting. The advantages include bone restoration for revisions, biocompatibility and low cost. Major disadvantages are risk of disease transmission, resorption, non-union and late collapse.
-
6.
Metal Augments: These can be used in place of bone graft. Brooks described them to be biomechanically equivalent to customised implants [4]. These wedge and tibial base plate construct behave similar to a customised prosthesis. They can be cemented after the tibia is prepared to match them. They provide immediate stability but do not conserve bone and ideally should be augmented with a stem extender. The advantages of the metal augments are that they are available in different shapes like wedges, hemi-wedges, blocks, full tibial plates and can be customised on table according to the defect to be filled. There is no need for these to be incorporated into bone and carry no risk of collapse or non-union in comparison to a bone graft. They can be used to fill defects up to 20 mm deep. Their main disadvantages are the cost, associated metallosis and inability to restore bone stock. Metal augments should be preferably used in elderly as revision may not be required in the near future (refer to Chap. 1).
Recently the focus has shifted towards use of tantalum metal augments. Their porosity provides a scaffolding for the osteoblast mediated bone ingrowth and they have a good biocompatibility and low modulus of elasticity. Their use is commonly restricted to revision scenario.
6 Complications
Commonly seen complications are related to graft non-union and failure of graft to incorporate and late collapse.
Case discussion: A 70 year old female presented with severe varus in both knees and inability to walk. Radiographs of knee showed advanced medial compartment osteoarthritis with postero-medial bone defects in tibia. Reconstruction was done using a conservative tibial cut. Cement with screw augmentation sufficed on the right side and left side had to be grafted with autografts. Stem extenders were used on tibial side on both sides (Fig. 14.8).
7 Tips and Pearls
-
1.
Always raw the base of crater to get a bleeding bone.
-
2.
Morselized graft should be washed with saline to remove blood and cartilage should be removed.
-
3.
Preferably use stem extenders to protect the bone graft.
-
4.
Weight bearing should be encouraged soon as graft incorporates under load.
-
5.
There should be no contact between the screw (SS) and the tibial base plate (titanium/CoCR), as it may lead to loosening due to battery effect.
8 Current Concept
Metaphyseal sleeves (commonly used in revision situations) may be used in the large bone defects as they provide immediate scratch fit in zone 2. Such defects are rarely seen in primary total knee replacements, but may sometimes be encountered in post-traumatic situations.
9 Discussion
Among the techniques available for filling bone defects in primary TKA, autografts are a cost effective, readily available and easy to use option for large uncontained postero-medial defects in tibia. Table 14.3 describes the options available for reconstructing the defects according to size and involvement of condyles.
Kharbanda and Sharma have reported successful outcomes in 54 knees reconstructed using autografts and impaction grafting. They did not find graft failure in any patient followed over a period of 5 years [5]. Dorr has reported use of bone grafts in 24 knees and it is incorporated in 22 knees [7]. Laskin reported failure of graft incorporation in four cases out of 26 patients he operated for bone defects [11]. Whereas Liu et al. operated 50 cases of bone defects and used screws to fix the graft, Pei et al. used a step cut bone graft to treat 19 knees with bone defects and no screws were used [12, 13]. Quantifying the defect guides in better management of defects using either structural or impaction bone grafting and/or use of sleeves and mega prosthesis (Table 14.3). Use of stem extenders has been shown to reduce the micromotion between implant and bone interface and thereby reducing stress on the graft [14]. Brooks et al. showed that a 70 mm stem used in conjunction with bone grafts carried 23–38% of axial load thereby protecting the graft [4]. Stems may be fixed using a fully cemented (short stubby stems), press fit uncemented (long with a diaphysial purchase) or hybrid techniques (prosthesis and metaphyseal region of stem is cemented and rest of the stem is uncemented). Meneghini et al. have suggested the use of cemented stems as they allow load sharing and protect the graft and help in bone incorporation into cones if used [15]. Cemented stems are useful in osteoporotic bones with large canals and can be adjusted intra-operatively. The problem with these is that they are difficult to remove at the time of revision and are not helpful in component alignment [16, 17]. Cementless stems are helpful in component alignment and provide stable fixation at the diaphysis [18]. Our preferred way is to use a hybrid fixation of stems.
Impaction bone grafting has been used by Cai et al. in 74 knees to fill bone defects in varus and valgus knees. He used pulverised 5 to 8 mm bone grafts to impact into the defect [19]. Bradley has used impaction allografting in revision knee arthroplasty and he advocated that specific to the technique, a solid support of implant-graft interface, graft-host bone interface and the use of a tight supportive stem is imperative [20]. The same principles apply while using allografts (if needed in primary situation). Tigani et al. used structural allografts in primary total knee for reconstruction of bone defects after proximal tibial plateau fractures and reported excellent results without any loosening or graft collapse [21].
Recently metaphyseal sleeves have been used to address severe bone loss encountered in primary total knee arthroplasty, especially after post-traumatic bone loss in proximal tibia. Hernandez has reported a 100% survival rate at mean follow-up on 79 months in 25 patients who underwent total knee arthroplasty using metaphyseal sleeves to fill defects in the proximal tibia [22]. Gill et al. have used metaphyseal sleeves for reconstruction of bone defects in primary (n = 12) and revision (n = 31) total knee arthroplasties followed for a mean 5.42 years and reported no failures due to aseptic loosening [23]. Metaphyseal sleeves definitely hold the future for management of severe bone loss encountered during knee arthroplasty.
10 Summary
Use cement and screw for small defects, autografts for larger defects in young since they are readily available in a primary knee replacement and preserve bone for future revisions. A metal wedge may be used in elderly where a future revision is not contemplated.
References
Dorr L. Bone graft for bone loss with total knee replacement. Orthop Clin North (Am). 1989;20(2):179–87.
Rand JA. Bone deficiency in total knee arthroplasty. Use of metal wedge augmentation. Clin Orthop Relat Res. 1991;271:63–71.
Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect. 1999;48:167–75.
Brooks PJ, Walker PS, Scott RD. Tibial component fixation in deficient tibial bone stock. Clin Orthop Related Res. 1984;184(4):302–8.
Kharbanda Y, Sharma M. Autograft reconstruction for bone defect in primary TKR. IJO. 2014;48(3):313–8.
Windsor RE, Insall JN, Sculco TP. Bone grafting of tibial defects in primary and revision total knee arthroplasty. Clin Orthop Relat Res. 1986;205:132–7.
Dorr LD, Ranawat CS, Sculco TA, McKaskill B. Bone graft for tibial defects in total knee arthroplasty 1986. Clin Orthop Relat Res. 2006;446:4–9.
Scuderi GR, Insall JN, Haas SB, Becker-Fluegel MW, Windsor RE. Bone grafting of tibial defects in primary and revision total knee arthroplasty. Clin Orthop. 1986;205:132–7.
Lonner JH, Lotke PA, Kim J, Nelson C. Impaction grafting and wire mesh for uncontained defects in revision knee arthroplasty. Clin Orthop Relat Res. 2002;404:145–51.
Lotke PA, Carolan GF, Puri N. Impaction grafting for bone defects in revision total knee arthroplasty. J Arthroplast. 2006;21(4 suppl 1):57–60.
Laskin RS. Total knee arthroplasty in the presence of large bony defects of the tibia and marked knee instability. Clin Orthop Relat Res. 1989;248:66–70.
Liu J, Sun ZH, Tian MQ, Wang P, Wang L. Autologous bone grafting plus screw fixation for medial tibial defects in total knee arthroplasty. Zhonghua Yi Xue Za Zhi. 2011;91:2046–50.
Pei Z, Guan ZP, Zhang SL, Li YP, Zhang Z. Autogeneous bone graft in the treatment of total knee arthroplasty for severe genu varus with tibial plateau bone defect. Beijing Da Xue Bao. 2011;43:707–13.
Rawlinson J, Closkey R, Davis N, Wright T, Windsor R. Stemmed implants improve stability in augmented constrained condylar knees. Clin Orthop Relat Res. 2008;466:2639–43.
Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. J Bone Joint Surg Am. 2008;9:78–84.
Murray PB, Rand JA, Hanssen AD. Cemented long stem revision total knee arthroplasty. Clin Orthop Relat Res. 1994;309:116–23.
Parsley BS, Sugano N, Bertulosso R, Conditt MA. Mechanical alignment of tibial stems in revision total knee arthroplasty. J Arthroplast. 2003;18(Suppl 1):33–6.
Radney CS, Scuderi GR. Management of bone loss: augments, cones, offset stems. Clin Orthop Relat Res. 2006;446:83–92.
Cai X, Wang Y, Wang JF, Zhou YG, Dong JY, Chen JY, et al. Impacted cancellous autograft for reconstructing bone defects of tibial plateau in total knee arthroplasty. Zhonghua Yi Xue Za Zhi. 2008;88:2907–11.
Bradley GW. Revision total knee arthroplasty by impaction bone grafting. Clin Orthop Related Res. 2000;371:113–8.
Tigani D, Dallari D, Coppola C, Ben Ayad R, et al. Total knee arthroplasty for post traumatic proximal tibial bone defect: three cases report. Open Orthop J. 2011;14:143–50.
Hernández CM, Floria-Arnal LJ, Blasco AG, Fernández AH, et al. Metaphyseal sleeves as the primary implant for management of bone defects in total knee arthroplasty after post-traumatic knee arthritis. Knee. 2018;25(4):669–75.
Gill UN, Ahmed N, Noor SS, Memon IA, et al. Memon ZA. Management of bone loss by metaphyseal sleeves in primary and revision knee arthroplasty: clinical experience and outcome after forty three cases. Int Orthop. 2020; https://doi.org/10.1007/s00264-020-04663-1.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Sharma, M., Anshu, A.K. (2022). Management of Bone Defects in Primary Total Knee Arthroplasty. In: Sharma, M. (eds) Knee Arthroplasty. Springer, Singapore. https://doi.org/10.1007/978-981-16-8591-0_14
Download citation
DOI: https://doi.org/10.1007/978-981-16-8591-0_14
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-8590-3
Online ISBN: 978-981-16-8591-0
eBook Packages: MedicineMedicine (R0)