Abstract
Purpose
To evaluate the clinical and radiological outcomes of unstable proximal humeral fractures (PHFs) treated with a locking plate and fibular strut allograft.
Methods
This study included 36 patients [7 men, 29 women; mean age, 68 years (range, 22–94 years)] with unstable PHFs with medial column disruption. All patients were treated with open reduction and internal fixation using a locking plate and fibular strut allograft. Post-operative assessment included clinical outcomes, shoulder range of motion, radiographic examination, and any complications. Post-operative radiological assessment including the humerus neck-shaft angle (NSA) and the humeral head height was performed.
Results
At the mean two year follow-up visit, the mean American Shoulder and Elbow Society (ASES) and University of California, Los Angeles (UCLA) scores were 77 and 28, respectively. According to the UCLA rating scale, the result was excellent in six, good in 20, fair in six, and poor in four cases. According to the Paavolainen method, 31 patients had good results with an NSA of 130 ± 10°; three patients showed fair results with an NSA of 100–120°, and two patients experienced a poor result with an NSA of <100°. When calculating the humeral head height, the mean loss of reduction was measured as 1.6 mm (from 10.8 or 9.2 mm). Varus collapse and avascular necrosis of the humeral head was noted in two patients for each condition.
Conclusions
For unstable proximal humerus fractures, particularly in elderly patients with severe osteoporosis or in younger patients with a four-part fracture, locking plate fixation with a fibular strut allograft provided rigid medial support and showed satisfactory clinical and radiological outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humeral fractures (PHFs) account for 5 % of all fractures, and they are the third most common fractures seen in patients older than 65 years of age [1]. More than 80 % of these fractures can be managed conservatively, but the treatment of displaced, unstable two-, three-, and four-part fractures still remains a clinical challenge [2]. These fractures are difficult to treat, as it is unpredictable whether they will achieve stable fixation that maintains intra-operative reduction. Locking plate fixation has the potential to provide greater fixation in the proximal humerus than standard plate fixation, offering a greater load to failure and the requirement for less soft-tissue dissection along the humeral shaft [3]. However, some studies have shown variable results, with complications ranging from 9 to 36 %, including high rates of screw penetration of the humeral head’s articular surface or varus collapse of the fracture, especially in osteoporotic bones or in fractures with medial column disruption or metaphyseal comminution [4–7]. Establishing medial column support should reduce these complications and enhance the functional results [8].
The goals of proximal humeral fracture fixation are as follows: anatomic reduction of all fracture fragments, re-establishment of the native humeral neck shaft angle (between 130 and 140°), restoration of the medial calcar, and stable fixation, which will permit early mobilization and return to normal function. Adequate mechanical support of the medial column may be obtained by achieving an anatomically stable reduction with a medial cortical contact or, in the case of medial comminution, by placing a superiorly directed oblique locking screw in the inferomedial region of the proximal fragment. Several studies have shown that fractures treated with either an anatomic reduction or screws in the inferomedial humeral head for which no medial column support was obtained had a high incidence of failure [5, 8–11]. Gardneret et al. [12] described the use of a fibular allograft that borrowed an intramedullary bone peg to act as a medial strut augment. Their initial clinical experience showed encouraging results, with seven out of seven fractures fixated with this construct proceeding to union without loss of reduction or fixation stability. Some previous biomechanical studies have also demonstrated that, under varus bending loads, the augmented construct has an increased initial stiffness and a higher ultimate failure load [13].
The purpose of this study was to evaluate the clinical and radiological outcomes of a locking plate with fibular allograft augmentation in unstable proximal humeral fractures with medial column disruption. We hypothesized that a fibular strut graft as an endosteal implant would be a safe and effective option to maintain reduction in unstable PHFs and would show low failure rates.
Materials and methods
Institutional Review Board approval was obtained for this investigation. We retrospectively evaluated 36 patients (7 men and 29 women) with unilateral displaced unstable PHFs treated at our institute by a single surgeon between March 2008 and March 2013 using locking plate fixation with intramedullary fibular strut allograft. The inclusion criteria involved unstable PHFs with metaphyseal comminution regardless of their Neer classification (Fig. 1). We included closed, displaced two-, three-, and four-part PHFs with a disrupted medial hinge, significant metaphyseal comminution with insufficient osseous contact between fracture fragments or head-splitting fracture. The exclusion criteria were open fractures, pathological fractures, an unreconstructable head, and/or tuberosity fragments, and stable fractures without medial hinge disruption or metaphysical comminution. The mean age of the patients at the time of surgery was 68 years (range, 24–94 years). The dominant arm was involved in 13 patients. The pre-operative evaluation included plain anteroposterior (AP) and lateral radiographs and a computed tomography (CT) scan in a three-dimensional reconstruction to evaluate the fracture configuration. Pre-operative assessment in terms of the shoulder’s range of motion and the clinical scores was not possible due to the severe pain associated with the fracture. The Neer classifications [14] of these fractures were as follows: two-part fractures, 13; three-part fractures, 16; four-part fractures, 7.
An 82-year-old woman sustained an unstable proximal humerus fracture with severe neck comminution from a fall. The pre-operative plain radiograph and CT scan showed severe neck comminution (a, b). Under c-arm guidance, a fibular allograft was inserted in the medial bony defect (c). The final radiograph showed a 110° neck shaft angle of the proximal humerus, and an evaluation of the Paavolainen method showed fair result. One cortical screw pushed the fibular allograft for the medial buttress (d)
Patients were regularly followed-up in the outpatient clinic (Table 1).
Post-operative assessment included the American Shoulder and Elbow Society (ASES) score and the University of California, Los Angeles (UCLA) score. Passive shoulder range of motion in terms of forward flexion, abduction, external rotation at the side, and internal rotation at the back were measured by a single examiner at the final using a goniometer follow-up visit. According to the UCLA rating scale, the results were categorized as follows: poor, 0–20; fair, 21–27; good, 28–33; excellent, 34–35. An excellent/good UCLA score indicates satisfactory results, whereas a fair/poor UCLA score suggests unsatisfactory results.
Radiographic follow-up was performed at immediate, one month, six months, and one year post-operatively. The radiologic follow-up included AP and lateral plain radiographs and measurement of the angle between the humeral head and the shaft in the AP view (the humeral neck-shaft angle). According to the Paavolainen method [15], restoration of the humeral neck-shaft angle to 130 ± 10° was considered to be good; a neck-shaft angle from 100 to 120° was considered to be fair, while a neck-shaft angle of <100° was thought to be a poor outcome.
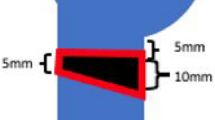
The “humeral head height” relative to the plate was measured on AP radiographs both on immediate post-operative radiograph and on the radiograph taken at the final follow-up visit, which allowed for subsequent analysis of any loss of reduction. This measurement was obtained by drawing two lines that ran perpendicular to the shaft of the plate; one was placed at the top edge of the plate, and the other was placed on the superior edge of the humeral head. The distance between these two lines was measured and designated as the head height [5] (Fig. 2). A difference in the humeral head height of >3 mm on the AP shoulder radiograph that was taken immediately following the operation and that obtained at the final follow-up was considered to indicate a loss of reduction. Complications were recorded, such as a collapse of the fracture, screw penetration, humeral head avascular necrosis (AVN), peri-implant fracture, infection, adhesive capsulitis, and the need for further surgery.
Calculation of the humeral head height. The two lines drawn running perpendicular to the shaft of the plate; one was placed at the top edge of the plate, and the other was placed at the superior edge of the humeral head. The distance between these two lines was measured and designated as the head height
Surgical technique
The patient was placed in a “beach chair” position on a radiolucent operating table under general anesthesia. The deltopectoral approach was used in all cases. The proximal humerus was exposed by retracting the deltoid muscle laterally and the pectoralis major muscle medially. The long head of the biceps was isolated and was detached proximally. The greater tuberosity (GT) fracture fragment was retracted by placing no. 2 nonabsorbable sutures (Ethibond®, Ethicon, USA) through the bone-tendon junction of the rotator cuff muscles. The fibula allograft was inserted into the humeral canal through the fracture site and pushed distally into the humeral shaft (Fig. 3a, b). It was then medialized maximally towards the calcar to indirectly reduce the medial column and advance in a retrograde fashion into the subchondral bone to lift the head superiorly (Fig. 3c). Thus, the proximal 2.5–3 cm of the fibular allograft was inserted into the proximal fracture fragment (humeral head), while the distal 3.5–4 cm of the allograft was placed into the distal fracture fragment (humeral shaft). If the diameter of the fibular allograft was similar to or less than the diameter of the humeral canal, it was relatively easy to insert the fibular allograft inside the humeral shaft. However, if the diameter of the fibula was more than the humeral canal diameter, we used a reciprocating saw to cut the graft and to achieve an adequate graft diameter. After confirming the anatomical reduction using a c-arm, a proximal humeral locking plate was used to fix the fracture fragments. If anatomical reduction was successful under c-arm guidance and medial column support was re-established, then locking screws were placed through the fibula into the humeral head and shaft to secure the plate’s position (Fig. 3d). If the medial column reduction could not be restored, the fibular allograft was used as an indirect reduction tool. We used a simple cortical screw through the plate to push the fibula medially until it apposed the medial cortex of the humerus and indirectly reduced the medial column. Even though the four-part fractures occurred in younger patients, we still performed an open reduction with fibular allograft in these patients. Initially, we inserted the fibular allograft into the humeral canal and then reduced the humeral head and shaft. The inserted fibular graft maintained a good alignment of the fracture, and the locking plate was easily applied to the fracture site. No. 2 Ethibond sutures were used to attach the humeral head fracture fragment to the lesser tuberosity and also the lesser tuberosity to the greater tuberosity. Chip bone allograft could be used in the bone defect site. Using no. 2 Ethibond sutures, meticulous repair of the rotator cuff to the plate was carried out (Fig. 4). In all cases, an infero-medial calcar screw was also inserted to provide additional support to the disrupted medial column. The wound was closed in layers, and a drain was placed under negative suction; this drain was removed after 48 hours.
Surgical procedure. a A severe bone defect was found in the unstable proximal humerus fracture with severe metaphyseal comminution. A fibular allograft is inserted to provide a medial buttress. b Under c-arm guide, a PHILOS locking plate was applied to the lateral aspect of the proximal humerus. c One locking screw pushes the fibular allograft to the fracture site to buttress the medial bone defect of the humerus. d Multiple non-absorbable sutures are passed to compress comminuted fragments to the bony defect of the proximal humerus
a In four-part proximal humerus fractures, impacted humeral head fragment was retrieved under the greater tuberosity fragments. b The fibular allograft is inserted into the humeral canal and helps in achieving satisfactory anatomical reduction. No. 2 Ethibond sutures were used to attach the humeral head fracture fragment to the lesser tuberosity and subscapularis tendon. c The construct is fixed with a PHILOS plate and screws and the tuberosity fragments are tied with the plate with the help of sutures passed through rotator cuff muscles and available holes in the plate. d Post-operative radiograph showing good anatomical reduction
An abduction brace was provided during the first four weeks post-operatively. Continuous shoulder passive motion, pendulum, and range of motion exercises of the elbow and wrist were allowed as tolerated from the second post-operative day. Active assisted elevation and further stretching was started at four weeks, and normal daily activities were gradually resumed as per the patient’s tolerance level and fracture union status on post-operative radiographs.
Results
All fractures healed clinically and radiologically. At the final follow-up, the average ASES and UCLA scores were 80.4 ± 13.7 (range, 45–100) and 28.8 ± 5.1 (range, 16–35), respectively. According to the UCLA rating scale, the result was excellent in six, good in 20, fair in six, and poor in four cases. Thus, a satisfactory result (excellent, good, fair) was seen in 32 (89 %) patients. Regarding the range of motion, the mean forward flexion, abduction, external rotation at the side, and internal rotation at the back were 143 ± 18° (90–180°), 141 ± 21° (70–180°), 26 ± 18° (0–70°), and at the T12 level (L4–T5), respectively.
Radiological results
The mean humeral NSA in the participants was 129 ± 14° (range, 87–154°). According to the Paavolainen method, 31 (68 %) patients had a good result with an NSA of 130 ± 10°, while 3 (23 %) patients showed a fair result with a neck-shaft angle of 100–120°, and 2 (9 %) patients experienced a poor result with a neck-shaft angle <100°. According to the calculations of the difference in the humeral head height on immediate post-operative radiograph and on final follow-up radiograph, the mean loss of reduction was 1.6 mm (from 10.6 ± 3.8 mm to 9.2 ± 3.5 mm). Five cases were found to have more than a 3-mm difference from the immediate post-operative measurement to the last follow-up measurement (Table 2).
Complications
Two major complications were noted: varus collapse and AVN (Fig. 5). Varus collapse was observed in two patients on the two month follow-up radiograph (Fig. 6), and AVN of the humeral head was seen in two patients, 30 and 9 months after the operation. Both patients were advised to pursue further surgical intervention, such as refixation or arthroplasty, but they both refused to undergo any treatment.
Two patients developed adhesive capsulitis, and the final outcome of these patients showed satisfactory results after plate removal. There were two cases in which the distal part of the drill bit broke while drilling through the fibula, but there was no further migration of the drill bit during the final follow-up period; both these patients had uneventful recoveries (Fig. 7). None of the patients presented with any major complications, such as subacromial impingement, neurovascular injury, loosening of the implant, or peri-implant fracture.
A 44-year-old woman sustained an unstable proximal humerus fracture with severe neck comminution from a traffic accident. The preoperative plain radiograph and CT scan showed severe neck comminution (a, b) The postoperative plain radiograph showed good medial support by the fibular strut allograft and locking plate (c). The one year follow-up radiograph showed a 130° neck shaft angle of the proximal humerus and the evaluation on the Paavolainen method showed a good result, and breakage of the drill bit due to the hard cortical bone of fibula allograft was shown (d)
Discussion
The purpose of this study was to analyze the clinical and radiographic outcomes of unstable PHFs treated with a locking plate and fibular allograft augmentation. As assessed by the UCLA rating scale, the results were excellent in four, good in 19, fair in six, and poor in two cases. According to the Paavolainen method, 21 (68 %) patients showed a good result, seven (23 %) had a fair result, and three (9 %) experienced a poor result. Varus collapse of the humeral head and AVN of the humeral head were each noted in two patients. When the humeral head height was measured using the immediate post-operative and final follow-up radiographs, a loss of reduction (>3 mm difference) was noted in four patients.
PHFs account for approximately 4–5 % of all fractures and approximately 10 % of all fractures in patients above 60 years of age, with an incidence of 6.6 in 1,000 persons [1, 16]. High rates of osteonecrosis and fracture collapse have led some authors to advocate for hemiarthroplasty as the treatment of choice for “at-risk” fractures [17]. However, the range of motion after hemiarthroplasty is highly variable, and two studies have reported no functional difference between hemiarthroplasty and nonsurgical treatment [18]. Internal fixation can produce better functional outcomes than hemiarthroplasty [19], particularly when complications are avoided [20]. Gradl et al. [21] concluded that patient’s age, sex, activity level, physical status and the presence of angular displacement were associated with a recommendation for internal fixation.
Fixed angle locking plates are now generally used for proximal humeral fractures, particularly in cases with severe osteoporosis and a distinct proximal bone detect. The anatomical locking plate (Synthes, Solothurn, Switzerland), such as the Proximal Humeral Internal Locking System (PHILOS), has also recently been favored. Several previous reports have identified reconstruction of the medial column as an important factor in minimizing the complications following surgical treatment of unstable proximal humeral fractures, especially varus collapse of the humeral head and loss of fixation [5, 8]. Zhang et al. [22] compared the clinical outcomes and complications after ORIF (open reduction and internal fixation) of proximal humeral fractures using either an S3 plate or a PHLP (proximal humeral locking plate) and found that the S3 humerus plate can be considered as an effective implant for ORIF of displaced unstable proximal humeral fractures.
Use of an endosteal strut allograft can re-establish medial support, even in the comminuted osteoporotic bone commonly found in these patients. The first clinical experience of this technique was reported in the literature by Gardner et al. [11] and showed encouraging results; seven out of seven fractures healed completely without a loss of reduction or fixation stability. Later, Neviaser et al. [23] reported low rates of reduction loss (2.6 %), screw cut-out (0 %), and osteonecrosis (2.6 %), as well as high clinical outcome scores in a series of 38 patients with displaced PHFs treated with locking plate fixation and an endosteal strut augment. Biomechanical testing showed that medial support with an intramedullary fibular graft and angular stable fixation increased the overall stiffness of the bone-implant construct and reduced migration of the humeral head fragment compared with the locking plate alone [24, 25]. Recently, Mostafa et al. [26] conducted a prospective study to evaluate the use of intramedullary non-vascularised autogenous fibular strut graft without internal fixation in patients with humeral aneurysmal bone cyst with varus deformity and found the technique to be effective in controlling deformity and improving function.
In cadaveric specimens, Chow et al. [24] showed how fibular allograft augmentation could increase the strength of the locking plate to withstand repetitive varus loading. None of the augmented constructs failed prior to 25,000 cycles, while six of the eight nonaugmented constructs failed at an average of 6,604 cycles. Neviaser et al. [20] examined outcomes of geriatric patients treated with open reduction and internal fixation using endosteal fibular strut allograft. These 31 patients were all older than 70 years, and only one case experienced a loss of reduction. No cases experienced screw penetration or AVN. This outcome demonstrates the utility of the endosteal support, even in older individuals with poorer bone quality.
We considered that the fibula might be the most suitable donor bone for reconstructing the medial support in these types of fractures. Its length, geometrical shape, and mechanical strength might also be appropriate for these fractures (Fig. 3). The cortical bone of the fibula provides immediate structural continuity and stability at the fracture site. When used as an intramedullary bone graft, it also has some osteogenic potential in addition to acting like a strut across the fracture site. The functional scores of our patients were superior to those reported after PHFs treated with hemiarthroplasty alone [27, 28]. The stability provided by the use of an endosteal fibula allograft permits an early and aggressive rehabilitation program, which improves function after fracture reconstruction [8]. The added stability also indirectly improves functional outcome scores by reducing complications and the functional deficits they incurred. In our series, we found lower rates of reduction loss (2.6 %), screw cutout (0 %), and osteonecrosis (2.6 %) than are typically reported for locking plates alone [4].
The fibular strut allograft may also minimize postoperative osteonecrosis by increasing the biomechanical strength of the construct and resisting a loss of reduction. Maintenance of reduction may permit revascularization of head pieces rendered ischemic at the time of injury. On the other hand, the disadvantages of a fibular allograft are the possibility of drill bit breakage due to the hard cortical bone of the fibula (Fig. 2), the high cost associated with the procedure, and a risk of infection. Although Vidyadhara et al. [29] showed concern regarding slow revascularization of the dead graft by creeping substitution or graft resorption, we did not encounter such problems.
The limitations of our study are as follows. First, we had no control group with similar fractures that was treated with alternative methods; therefore, we cannot make direct comparisons of any treatment methods. Second, the duration of the follow-up was also relatively short; conditions including osteonecrosis may appear with longer monitoring. There is no established standard for monitoring osteonecrosis in the reconstructed proximal humerus, but post-fracture osteonecrosis occurring in the femoral head has been reported to occur even after a long duration. Also, appropriate length of fibula allograft for the fracture stability was not standardized, so that further biomechanical study will be needed.
Conclusion
Our study demonstrates that unstable, complex PHFs with medial comminution can be reliably treated with joint-preserving techniques using fibular allografts and locking plates to restore the integrity of the medial column, support the humeral head, and maintain reduction until the fracture can heal. Consistently, high functional scores can be achieved with this method even when treating three- and four-part fractures, especially in younger patients. A second column of support is easily established: the stability of the reconstruction has improved, and reduction is maintained. This minimizes the most frequent complications reported with proximal humeral locking plates and allows for early and aggressive rehabilitation with greater patient satisfaction.
References
Baron JA, Karagas M, Barrett J, Kniffin W, Malenka D, Mayor M, Keller RB (1996) Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology 7:612–618
Neer CS 2nd (2006) Displaced proximal humeral fractures. Part I. Classification and evaluation. Clin Orthop Relat Res 442:77–82
Walsh S, Reindl R, Harvey E, Berry G, Beckman L, Steffen T (2006) Biomechanical comparison of a unique locking plate versus a standard plate for internal fixation of proximal humerus fractures in a cadaveric model. Clin Biomech (Bristol, Avon) 21(10):1027–1031
Brunner F, Sommer C, Bahrs C, Heuwinkel R, Hafner C, Rillmann P, Kohut G, Ekelund A, Muller M, Audigé L, Babst R (2009) Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma 23:163–172. doi:10.1097/BOT.0b013e3181920e5b
Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG (2007) The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma 21(3):185–191
Koukakis A, Apostolou CD, Taneja T, Korres DS, Amini A (2006) Fixation of proximal humerus fractures using the PHILOS plate: early experience. Clin Orthop Relat Res 442:115–120. doi:10.1097/01.blo.0000194678.87258.6e
Ricchetti ET, Warrender WJ, Abboud JA (2010) Use of locking plates in the treatment of proximal humerus fractures. J Shoulder Elbow Surg 19 (2 Suppl):66–75. doi: 10.1016/j.jse.2010.01.001
Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS (2011) Predicting failure after surgical fixation of proximal humerus fractures. Injury 42(11):1283–1288. doi:10.1016/j.injury.2011.01.017
Hardeman F, Bollars P, Donnelly M, Bellemans J, Nijs S (2012) Predictive factors for functional outcome and failure in angular stable osteosynthesis of the proximal humerus. Injury 43(2):153–158. doi:10.1016/j.injury.2011.04.003
Lescheid J, Zdero R, Shah S, Kuzyk PR, Schemitsch EH (2010) The biomechanics of locked plating for repairing proximal humerus fractures with or without medial cortical support. J Trauma 69:1235–1242. doi:10.1097/TA.0b013e3181beed96
Gardner MJ, Boraiah S, Helfet DL, Lorich DG (2008) Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant. J Orthop Trauma 22:195–200. doi:10.1097/BOT.0b013e31815b3922
Mathison C, Chaudhary R, Beaupre L, Reynolds M, Adeeb S, Bouliane M (2010) Biomechanical analysis of proximal humeral fixation using locking plate fixation with an intramedullary fibular allograft. Clin Biomech 25(7):642–646. doi:10.1016/j.clinbiomech.2010.04.006
Neer CS 2nd (1970) Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 52:1077–1089
Paavolainen P, Bjorkenheim JM, Slatis P, Paukku P (1983) Operative treatment of severe proximal humeral fractures. Acta Orthop Scand 54:374–379
Lill H, Hepp P, Korner J, Kassi JP, Verheyden AP, Josten C, Duda GN (2003) Proximal humeral fractures: how stiff should an implant be? A comparative mechanical study with new implants in human specimens. Arch Orthop Trauma Surg 123:74–81
Rockwood CA, Green DP (1994) Fractures in adults, vol 1, 3rd edn. J.B. Lippincott, Philadelphia, pp 871–927
Den Hartog D, Van Lieshout EM, Tuinebreijer WE, Polinder S, Van Beeck EF, Breederveld RS, Bronkhorst MW, Eerenberg JP, Rhemrev S, Roerdink WH, Schraa G, Van der Vis HM, Van Thiel TP, Patka P, Nijs S, Schep NW (2010) Primary hemiarthroplasty versus conservative treatment for comminuted fractures of the proximal humerus in the elderly (ProCon): a multicenter randomized controlled trial. BMC Musculoskelet Disord 25(11):97
Solberg BD, Moon CN, Franco DP, Paiement GD (2009) Surgical treatment of three and four-part proximal humeral fractures. J Bone Joint Surg Am 91:1689–1697. doi:10.2106/JBJS.H.00133
Resch H, Beck E, Bayley I (1995) Reconstruction of the valgus-impacted humeral head fracture. J Shoulder Elbow Surg 4(2):73–80
Neviaser AS, Hettrich CM, Beamer BS, Dines JS, Lorich DG (2011) Endosteal strut augment reduces complications associated with proximal humeral locking plates. Clin Orthop Relat Res 469:3300–3306
Gradl G, Knobe M, Pape HC, Neuhaus PV, Ring D, Guitton T (2015) Decision making in displaced fractures of the proximal humerus: fracture or surgeon based? Int Orthop 39(2):329–334. doi:10.1007/s00264-014-2630-5
Zhang F, Zhu L, Yang D, Yang P, Ma J, Fu Q, Chen A (2015) Comparison between the spatial subchondral support plate and the proximal humeral locking plate in the treatment of unstable proximal humeral fractures. Int Orthop 39(6):1167–1173. doi:10.1007/s00264-015-2705-y
Bae JH, Oh JK, Chon CS, Oh CW, Hwang JH, Yoon YC (2011) The biomechanical performance of locking plate fixation with intramedullary fibular strut graft augmentation in the treatment of unstable fractures of the proximal humerus. J Bone Joint Surg (Br) 98(7):937–941. doi:10.1302/0301-620X.93B7.26125
Chow RM, Begum F, Beaupre LA, Carey JP, Adeeb S, Bouliane MJ (2011) Proximal humeral fracture fixation: locking plate construct ± intramedullary fibular allograft. J Shoulder Elbow Surg 21(7):894–901. doi:10.1016/j.jse.2011.04.015
Reddix RN, Russell G, Woodall J, Jackson B, Dedmond B, Webb LX (2009) Relationship between intraoperative femoral head bleeding and development of avascular necrosis after acetabular fracture surgery. J Surg Orthop Adv 18(3):129–133
Mostafa MF, Fawzy SI (2015) Fibular strut graft for humeral aneurysmal bone cyst with varus deformity. Int Orthop 39(7):1391-1398. doi:10.1007/s00264-015-2746-2
Antuna SA, Sperling JW, Cofield RH (2008) Shoulder hemiarthroplasty for acute fractures of the proximal humerus: a minimum five-year follow-up. J Shoulder Elbow Surg 17(2):202–9. doi:10.1016/j.jse.2007.06.025
Kontakis G, Koutras C, Tosounidis T, Giannoudis P (2008) Early management of proximal humeral fractures with hemiarthroplasty: a systematic review. J Bone Joint Surg (Br) 90:1407–1413
Vidyadhara S, Vamsi K, Rao SK, Gnanadoss JJ, Pandian S (2009) Use of intramedullary fibular strut graft: a novel adjunct to plating in the treatment of osteoporotic humeral shaft nonunion. Int Orthop 33(4):1009–1014. doi:10.1007/s00264-008-0596-x
Acknowledgments
This study was approved by Daejeon St. Mary’s Hospital, no. DC10EISI0019.
Conflicts of interest
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Panchal, K., Jeong, JJ., Park, SE. et al. Clinical and radiological outcomes of unstable proximal humeral fractures treated with a locking plate and fibular strut allograft. International Orthopaedics (SICOT) 40, 569–577 (2016). https://doi.org/10.1007/s00264-015-2950-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2950-0