Abstract
Purpose
The osteogenic potential of in vitro osteo-induced adipose-derived mesenchymal stem cells (ADSCs) combined with platelet-rich plasma (PRP) and implanted on bone mineral matrix (BMM) carrier was examined in a subcutaneous model in Balb/c mice.
Methods
In vitro osteogenic differentiation of ADSCs was monitored by relative bone-related gene expression and osteocalcin expression at the third, seventh and 15th day. Test implants consisting of in vitro osteo-induced ADSCs, PRP and BMM (OPC implants) and control implants consisting of PRP and BMM (PC implants) were examined. The relative expression of the bone-related genes encoding osterix, osteocalcin, collagen type I α1 and alkaline phosphatase was examined in implants extracted at one, two, four and eight weeks. Histochemical, immunohistochemical and histomorphometric analyses of implants extracted at two and eight weeks were performed.
Results
The highest relative expression of bone-related genes and osteocalcin expression was found at the 15th day of in vitro osteogenic induction of the ADSCs. Permanent and continuous increased expression of bone-related genes was noticed in OPC implants at eight weeks. Expression peaks of bone-related genes in PC implants were at two and four weeks, but they significantly decreased at eight weeks. The signs of resorption, formation of callus-like tissue positive for osteocalcin and increased presence of bone cells were found in OPC implants compared with PC implants. A higher percentage of infiltrated tissue and vascularisation was found in OPC than in PC implants.
Conclusions
The combination of in vitro osteo-induced ADSCs and PRP on BMM carrier represents a promising approach for bone regeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adipose-derived mesenchymal stem cells (ADSCs) are multipotent cells [1, 2] that can successfully adhere to bone substitute materials, proliferate rapidly and have osteogenic potential [3, 4], which makes them good candidates for assisted bone tissue regeneration [2].
Bone substitute material and sources of growth and differentiation factors are of crucial importance for cell-based bone tissue reparation [2, 5]. Bone substitutes serve as cell carriers that imitate the natural bone environment, promote a rapid attachment, proliferation and differentiation of ADSCs [3, 4]. Platelet-rich plasma (PRP) is frequently used as a natural source of proliferation and growth factors [6]. Addition of the activated PRP stimulates in vivo differentiation and proliferation of implanted cells [7] and simulates natural conditions during bone injury.
There is a need in clinical orthopaedic practice for an alternative to bone grafting, such as the combined use of stem cells, bone substitutes and growth and differentiation factors for bone regeneration [8]. So far, the specific roles of mesenchymal stem cells (MSCs) in bone fracture healing are not entirely clear [2]. In order to give closer insight into this concern, the osteogenic potential of in vitro osteo-induced ADSCs, combined with PRP and implanted on bone mineral matrix as a carrier, was examined in the subcutaneous mouse model. This model is a suitable and frequently used one [7] because it allows evaluation of in vivo osteogenic potential of ADSCs, thus avoiding the influence of the bone microenvironment [9].
Materials and methods
Isolation, expansion and osteogenic induction of ADSCs
Isolated epididymal adipose tissue from BALB/c mice was washed, macerated and digested using collagenase type I (Sigma-Aldrich, Hamburg, Germany) at a concentration of 2,000 I.U. per ml of Dulbecco’s Modified Eagles Minimal Essential Medium (DMEM; PAA Laboratories, Pasching, Austria). Digestion lasted for 45 minutes at 37 °C and then the homogenate was filtered and centrifuged at 1,500 rpm, ten minutes. The pellet that contained the stromal vascular fraction (SVF) was re-suspended and cells were counted using the trypan blue dye exclusion method and seeded at a density 1 × 106 per flask (25 cm2). ADSCs derived from SVF were cultivated in DMEM, supplemented with 10 % fetal bovine serum, antibiotic-antimycotic solution and 2 mM L-glutamine (all from PAA Laboratories, Pasching, Austria), in a humidified atmosphere containing 5 % CO2, at 37 °C. The media was replaced every two to three days until reaching confluency of 80 %.
At the third passage, ADSCs were subjected to osteogenic differentiation. The cells were seeded in 24-well plates (Greiner Bio-One, Frickenhausen, Germany), at density 1 × 104 per well, and cultivated in osteoinductive media (OM) up to 15 days prior to the preparation of implants for in vivo experiment. The OM contained 10−8 M dexamethasone, 50 μg/mL ascorbic acid and 10 mM β-glycerophosphate in DMEM supplemented with 10 % FBS, antibiotic-antimycotic solution and L-glutamine [10]. To monitor the change of bone-related gene expression during the osteogenic induction, cells were placed in RNAlater® (Ambion, Life Technologies, Paisley, UK) at the third, seventh and 15th day and stored at −80 °C until RNA purification step.
Immunocytochemistry
After the third passage, anti-integrin β1, CD29 (1:400, ab52971; Abcam, Cambridge, UK) antibody was used as a positive MSC marker. To assess the osteogenic phenotype at the 15th day of in vitro osteogenic differentiation, antibody to osteocalcin (1:200, ab93876; Abcam) was used. Primary antibodies were applied overnight at 4 °C. An HRP/DAB detection kit (ab64261; Abcam) was used for visualisation, according to the manufacturer’s instructions. Cells were counterstained with Mayer’s haematoxylin (1 min, room temperature) and mounted.
Experimental animals
Syngeneic male Balb/c mice, 22–24 g in weight and 8 weeks old were used. During the experiment, animals were held in standard conditions and access to food and drink ad libitum. All procedures on animals were performed in accordance with the ethical standards of the Animal Welfare Act of the Republic of Serbia. Approval for the experiment was obtained by the Local Ethical Committee of the Faculty of Medicine, University of Niš, Serbia (approval 01-5518-7).
Preparation of PRP
The PRP was prepared by a two-step method [11]. Blood was collected from the orbital plexus of one group of mice into tubes with anticoagulant sodium citrate. Prepared PRP had two to six times higher concentration of platelets than normal physiological level. Platelets number was established by Malassez counting chamber (Paul Marienfeld, Lauda-Königshofen, Germany) and it was 1.48 ± 0.3 × 106 μl−1.
Preparation of implants and implantation procedure
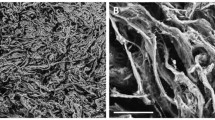
Bone substitute material Bio-Oss®, size S (Geistlich-Pharma, Wolhusen, Switzerland), which represented the bone mineral matrix (BMM) was used as a cell carrier. Two types of implants were prepared: (1) OPC implants consisted of in vitro osteo-induced ADSCs, numbered 5 × 105 ml−1, mixed with activated PRP (activated with calcium chloride) and loaded onto BMM and (2) PC implants as a control group consisted of activated PRP mixed with DMEM and loaded onto BMM. Each implant consisted of 10 mg (0.02 cm3) of BMM. The PRP at concentration of 10 % was used per one implant as the most optimal concentration for combining with osteoprogenitor cells [5]. Before implantation the cells were allowed approximately 15 minutes to attach to BMM and fibrin fibres to be formed within the implants [12].
The animals were divided into two experimental groups, based on the type of implant, each consisted of 16 animals. We had four experimental periods (1, 2, 4 and 8 weeks) with four animals per each. Immediately after extraction, the implants were stored in the RNAlater® at −80 °C. For histochemical and immunohistochemical analysis we used implants extracted two and eight weeks after implantation.
Assessment of bone-related gene expression
The total RNA was isolated from the extracted implants and in vitro osteo-induced ADSCs by using RNeasy Mini Kit (Qiagen, Hilden, Germany) and Dnase I RNase-free set (Qiagen) for residual DNA digestion, according to the manufacturer’s instructions. The RNA concentration was determined immediately after isolation by using Qubit® RNA assay kit and Qubit® 2.0 fluorometer (Invitrogen, Thermo Fisher Scientific, Waltham, MA, USA), according to manufacturer’s instructions.
Whole RNA was reversely transcribed into single-stranded cDNA by using a High-capacity cDNA Reverse Transcription Kit (Applied Biosystems®, Thermo Fisher Scientific, Waltham, MA, USA). The reactions were performed and tracked in the PCR thermal cycler (SureCycler8800; Agilent Technologies, Santa Clara, CA, USA), according to the manufacturer’s instructions.
Quantitative real-time PCR reactions were performed, monitored and analysed by the real-time termal cycler, Stratagene MxPro-Mx3005P (Agilent Technologies, Santa Clara, CA, USA). The reactions were prepared by using Kapa Sybr® Fast Universal 2× qPCR Master Mix (Kapa Biosystems, Wilmington, MA, USA), according to manufacturer’s instruction. A mix of reverse/forward primers for mice (Quantitect primer assays; Qiagen, Hilden, Germany) was used for bone-related genes transcription factor osterix (SP7), osteocalcin (BGLAP), collagen type I α1 chain (COL1A1) and tissue non-specific alkaline phosphatase (ALPL) (Table 1). The results were expressed relative to the bone-related gene expression levels in SVF (initial source of the cells) and normalised to the expression of housekeeping gene β-actin.
Histology
The extracted implants were fixed in 10 % neutral buffered formalin and decalcified in 10 % ethylenediaminetetra-acetic acid (EDTA) solution (pH 7.4). Tissue was processed and embedded in paraffin. Tissue blocks were cut at 4 μm using a microtome Leica RM2235. Masson’s trichrome and haematoxylin and eosin (H&E) staining were performed with tissue sections. The stained slides were analysed on the Leica System Microscope DM2500 equipped with Leica DFC490 Digital Camera (Leica Microsystems, Wetzlar, Germany).
Immunohistochemistry
After deparaffinisation, tissue sections were subjected to heat-induced antigen retrieval using sodium citrate. Primary antibody to osteocalcin (1:200, ab93876; Abcam, Cambridge, UK) was applied overnight at 4 °C. For visualisation, HRP/DAB detection kit (ab64261; Abcam) was used according to the manufacturer’s instructions. Tissue sections were counterstained with Mayer’s haematoxylin (5 min, room temperature) and mounted.
Histomorphometry
Histomorphometrical measurements were performed in NIS-Elements software version 3.2 (Nikon, Chiyoda, Japan). The images were obtained by using the microscope Axio Observer.Z1 equipped with the camera AxioCam HR (Carl Zeiss, Oberkochen, Germany) at ×100 magnification. Total area of explants, total vessel area and area of material granules on H&E stained tissue sections were measured using the “Annotations and Measurements” software tool. The percentage of vascularisation was calculated as follows: (total vessel area / total area of explants) × 100, while the percentage of infiltrated tissue was calculated as follows: ((total area of explants – total area of material granules) / total area of explants) × 100.
Statistical analysis
The mean values of relative gene expression, percentage of infiltrated tissue and vascularisation ± SD, were used for analysis. Statistical analyses were conducted using the Kruskal-Wallis ANOVA and a post hoc Mann-Whitney tests in SPSS software version 15.0 (SPSS, Chicago, IL, USA). Statistically significant differences were considered for p < 0.05.
Results
Characterisation and evaluation of osteogenic differentiation of ADSCs
Isolated ADSCs expressed the CD29 marker (Fig. 1a, b). On the 15th day, ADSCs cultivated in OM exhibited pronouncedly the highest relative expression levels of bone-related genes (Fig. 1e–h) and were positive for osteocalcin (Fig. 1c, d).
Characterisation and evaluation of osteogenic differentiation of ADSCs. a ADSCs at the third passage were CD29 positive (circle); b negative control (without primary antibody). Bar 100 μm; magnification 200×. c ADSCs cultivated in OM for 15 days were positive for osteocalcin; (d) negative control (without primary antibody). Bar 20 μm; magnification 400×. e-h Prior to implantation, the dynamics of SP7, BGLAP, COL1A1 and ALPL expression within in vitro osteo-induced ADSCs was examined at the 3rd (3d), 7th (7d) and 15th day (15d)
qRT-PCR analysis of relative bone-related gene expression pattern in extracted implants
Dynamics and pattern of relative expression of bone-related genes in OPC and PC implants are shown and explained in Fig. 2.
Dynamics and pattern of relative expression levels of SP7, BGLAP, COL1A1 and ALPL in OPC and PC implants extracted at one, two, four and eight weeks of the in vivo experimental period. Significant differences between groups within the same experimental period: *p < 0.05. At one and two weeks, significantly elevated expression level of SP7 was exhibited in the PC implants compared with the OPC implants while at eight weeks it was vice versa. Significantly higher expression of BGLAP was noticed in the OPC than in the PC implants at eight weeks. At two weeks, the expression of COL1A1 was significantly higher in the PC implants than in the OPC, while at eight weeks it was vice versa. Significantly elevated expression level of ALPL was observed in the OPC implants in comparison with PC at eight weeks
Histochemical and immunohistochemical analysis
Histochemical and immunohistochemical analysis of the OPC and PC implants are shown and explained in Figs. 3 and 4.
Sections of the OPC and PC implants extracted at two weeks of in vivo experimental period. Masson’s trichrome staining of the OPC (a) and the PC implants (b). BMM bovine bone mineral matrix granules. Greater presence of multinucleated osteoclast-like cells and blood vessels (arrows) was noticed in the OPC implants compared with PC implants. More collagen fibres between BMM granules were noticed in the PC than in OPC implants. Magnification 200×; bar 50 μm. Expression of osteocalcin in the OPC implants (c) and in the PC implants (d). Expression of osteocalcin was a bit more intensive in the OPC than in PC implants (showed with ellipses). Magnification 400×; bars 20 μm
Sections of the OPC and PC implants extracted at eight weeks of in vivo experimental period. Masson’s trichrome staining of OPC (a) and PC implants (b). BMM bovine bone mineral matrix granules. Increased presence of the flattened bone lining osteoblast-like cells and larger blood vessels (arrows) were noticed in the OPC implants in comparison to the PC implants. The signs of resorption of BMM granules were more intensive (ellipses) in the OPC implants compared with the PC. In the OPC implants, the matrix consisted of mature, dense collagen fibres which formed callus-like tissue were noticed (red ellipses), while in the PC implants collagen was mostly loose. Expression of osteocalcin in the OPC implants (c) and in the PC implants (d). Stronger expression of osteocalcin at the edge of BMM granules and in extracellular matrix was noticed in the OPC compared with PC implants (squares). Magnification 200×; bars 50 μm
Histomorphometrical analysis
The percentage of infiltrated tissue and vascularisation in OPC and PC implants are shown and explained in Fig. 5.
The percentage of infiltrated tissue and vascularisation in the OPC and PC implants extracted at two and eight weeks of in vivo experimental period. Significant differences between groups: **p < 0.01. Percentage of infiltrated tissue was higher in the OPC implants compared with PC implants but statistical significance was observed only at two weeks. Percentage of vascularisation was higher in the OPC than in the PC implants but statistical significance was observed only at eight weeks
Discussion
At the third passage after isolation, the purified fraction of cells expressed CD29, a highly specific MSC marker [13] (Fig. 1a, b). Based on the literature data [1, 14], in vitro osteogenic differentiation of ADSCs was evaluated by the expression of osteocalcin and expression levels of SP7, BGLAP, COL1A1 and ALPL. Positive immunocytochemical staining for osteocalcin (Fig. 1c, d), which is a highly specific marker of bone cells [14], and pronouncedly upregulated expression of bone-related genes at the 15th day of in vitro osteogenic induction (Fig. 1e–h) indicated that ADSCs in our study were successfully induced towards osteoblasts. Our results are consistent with other studies which reported that differentiation occurred in two weeks [15].
Different dynamic and pattern of the bone-related gene expression was seen in OPC and PC implants (Fig. 2). The gene for osteoblast-specific transcription factor osterix [16] was expressed earlier in PC than in OPC implants with nearly steady expression pattern. On the other hand, a stable gradual increase in the expression level of SP7 was exhibited in OPC implants from the first to the eighth week. Low expression levels of BGLAP in implants of both groups at one and two weeks are in accordance with the fact that osteocalcin is mostly expressed during the late stage of osteoprogenitor differentiation [14].
The expression pattern of SP7 and BGLAP in OPC implants can be explained in two ways. First, after implantations, the implants were populated by resident osteoprogenitor cells under the influence of the implant components [17, 18]. Thus, the recruited cells modulated gene expression pattern in the OPC implants. Second, the ADSCs downregulated the expression levels of bone-related genes because their environment was changed by implant construction and in vivo application. This kind of response in osteoprogenitor cells was noticed earlier by Lian and Stein [19]. The in vitro osteo-induced ADSCs needed time to adapt, multiply and continue differentiation process after implantation. Nevertheless, once the expression of SP7 and BGLAP was initiated in OPC implants, it progressed gradually and continuously to the eighth week. The dynamics and patterns of the SP7 and BGLAP expression which are seen in the PC implants are not odd. Some studies have shown that the combination of PRP only with a bone substitute material has osteoinductive properties [6, 20]. Thus, the expression levels of SP7 and BGLAP was initiated earlier in the PC implants but expression decreased from the fourth to the eighth week.
COL1A1 expression is an important early marker of the osteogenic process [14]. An early expression of COL1A1 was exhibited in both examined groups of implants. The expression peak occurred at two weeks in PC implants and further decreased to the eighth week, while in OPC implants expression was steady at one, two and four weeks but further increased to the eighth week. This suggests different patterns of osteogenic process in the OPC and the PC implants.
An elevated expression of alkaline phosphatase is characteristic for pre-osteoblasts and differentiated osteoblasts [14] are mandatory for mineralisation [21]. Significantly elevated ALPL expression in the OPC implants at eight weeks suggests that the osteogenic process was more advanced in the OPC than in the PC implants. Negative ALPL expression in both groups indicates that freshly isolated and untreated ADSCs (calibrator) have a high expression level of ALPL. This could be due to the fact that ALPL encodes tissue non-specific alkaline phosphatase which is also present in other tissues besides bone. Despite that, ALPL was frequently used for evaluation of osteogenic process [22, 23].
The presence of in vitro osteo-induced ADSCs in OPC implants induced significantly higher percentage of infiltrated tissue compared with PC implants (Fig. 5). The characteristics of infiltrated tissue in both groups of implants had been changed over time. More collagen fibres were noticed within PC implants than OPC at two weeks (Fig. 3a, b), which is consistent with COL1A1 expression at this point. At eight weeks, collagen was present in both groups of implants, but the callus-like formation which is characteristic of early osteogenesis [24], was observed only in the OPC implants. This is supported with stronger expression of osteocalcin near BMM granules and in the matrix of OPC implants (Fig. 4). At this point, weak expression of osteocalcin in loose collagen matrix was seen in PC implants. In addition, the signs of intensive resorption and increased presence of osteoblast-like and multinucleated osteoclast-like cells were noticed in OPC compared with PC implants at each observation point (Figs. 3 and 4). The expression peaks of SP7, BGLAP and ALPL at eight weeks in OPC implants support the observation of higher activity and presence of osteoblast-like cells. The development of osteogenic process from the second to the eighth week in OPC implants was followed by a significant increase in the percentage of vascularisation (Fig. 5). All of these findings suggest a well-balanced osteogenesis in OPC implants. On the other hand, the absence of callus-like tissue, less presence of bone cells and significantly lower percentage of vascularisation indicate that osteogenic process was less expressed in PC than in OPC implants (Figs. 3, 4 and 5).
In summary, pronouncedly the highest relative expression of bone-related genes and osteocalcin expression were found at the 15th day of in vitro osteogenic induction of ADSCs. Therefore, ADSCs induced in that way were combined with PRP and BMM to evaluate their in vivo osteogenic potential in the ectopic model. Our results indicate that this combination triggered a more advanced and well-balanced osteogenic process than in the control group of implants consisting only of PRP and BMM. Thus, the combination of in vitro osteo-induced ADSCs for 15 days, PRP and BMM should be taken into consideration for the treatment of bone defects as an alternative to bone grafting. Only a few successful clinical studies, with implementation of ADSCs, were conducted [18]. Our study set the foundation for further investigation that is needed before the final translation of the presented approach to the clinical application.
References
Bourin P, Bunnell BA, Casteilla L, Dominici M, Katz AJ, March KL, Redl H, Rubin JP, Yoshimura K, Gimble JM (2013) Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: a joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy 15(6):641–648
Wang X, Wang Y, Gou W, Lu Q, Peng J, Lu S (2013) Role of mesenchymal stem cells in bone regeneration and fracture repair: a review. Int Orthop 37(12):2491–2498
Hicok KC, Du Laney TV, Zhou YS, Halvorsen YC, Hitt DC, Cooper LF, Gimble JM (2004) Human adipose-derived adult stem cells produce osteoid in vivo. Tissue Eng 10(3–4):371–380
Cowan CM, Shi Y, Aalami OO, Chou Y, Mari C, Thomas R, Quarto N, Contag CH, Wu B, Longaker MT (2004) Adipose-derived adult stromal cells heal critical-size mouse calvarial defects. Nat Biotechnol 22(5):560–567
Liu Y, Zhou Y, Feng H, Ma G, Ni Y (2008) Injectable tissue-engineered bone composed of human adipose-derived stromal cells and platelet-rich plasma. Biomaterials 29(23):3338–3345
Intini G (2009) The use of platelet-rich plasma in bone reconstruction therapy. Biomaterials 30(28):4956–4966
Goto H, Matsuyama T, Miyamoto M, Yonamine Y, Izumi Y (2006) Platelet-rich plasma/osteoblasts complex induces bone formation via osteoblastic differentiation following subcutaneous transplantation. J Periodontal Res 41(5):455–462
Oryan A, Alidadi S, Moshiri A, Maffulli N (2014) Bone regenerative medicine: classic options, novel strategies, and future directions. J Orthop Surg Res 9:18
Scherberich A, Müller AM, Schäfer DJ, Banfi A, Martin I (2010) Adipose tissue-derived progenitors for engineering osteogenic and vasculogenic grafts. J Cell Physiol 225(2):348–353
Hayashi O, Katsube Y, Hirose M, Ohgushi H, Ito H (2008) Comparison of osteogenic ability of rat mesenchymal stem cells from bone marrow, periosteum, and adipose tissue. Calcif Tissue Int 82(3):238–247
Intini G, Andreana S, Intini FE, Buhite RJ, Bobek LA (2007) Calcium sulfate and platelet-rich plasma make a novel osteoinductive biomaterial for bone regeneration. J Transl Med 5:13
Muller A, Mehrkens A, Schafer D, Jaquiery C, Guven S, Lehmicke M, Martinetti R, Farhadi I, Jakob M, Scherberich A (2010) Towards an intraoperative engineering of osteogenic and vasculogenic grafts from the stromal vascular fraction of human adipose tissue. Eur Cell Mater 19:127–135
Sung J, Yang H, Park J, Choi G, Joh J, Kwon C, Chun J, Lee S, Kim S (2008) Isolation and characterization of mouse mesenchymal stem cells. Transplant Proc 40(8):2649–2654
Huang W, Yang S, Shao J, Li YP (2007) Signaling and transcriptional regulation in osteoblast commitment and differentiation. Front Biosci 12:3068–3092
Huang JI, Beanes SR, Zhu M, Lorenz HP, Hedrick MH, Benhaim P (2002) Rat extramedullary adipose tissue as a source of osteochondrogenic progenitor cells. Plast Reconstr Surg 109(3):1033–1041
Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, Behringer RR, de Crombrugghe B (2002) The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell 108(1):17–29
Amini AR, Laurencin CT, Nukavarapu SP (2012) Bone tissue engineering: recent advances and challenges. Crit Rev Biomed Eng 40(5):363–408
Barba M, Cicione C, Bernardini C, Michetti F, Lattanzi W (2013) Adipose-derived mesenchymal cells for bone regereneration: state of the art. Biomed Res Int 2013:416391. doi:10.1155/2013/416391
Lian JB, Stein GS (1995) Development of the osteoblast phenotype: molecular mechanisms mediating osteoblast growth and differentiation. Iowa Orthop J 15:118–140
Kasten P, Vogel J, Geiger F, Niemeyer P, Luginbühl R, Szalay K (2008) The effect of platelet-rich plasma on healing in critical-size long-bone defects. Biomaterials 29(29):3983–3992
Orimo H (2010) The mechanism of mineralization and the role of alkaline phosphatase in health and disease. J Nippon Med Sch 77(1):4–12
Mathews S, Bhonde R, Gupta PK, Totey S (2012) Extracellular matrix protein mediated regulation of the osteoblast differentiation of bone marrow derived human mesenchymal stem cells. Differentiation 84(2):185–192
Schwarting T, Benölken M, Ruchholtz S, Frink M, Lechler P (2015) Bone morphogenetic protein-7 enhances bone-tendon integration in a murine in vitro co-culture model. Int Orthop 39:799–805
Mehrkens A, Saxer F, Güven S, Hoffmann W, Müller AM, Jakob M, Weber FE, Martin I, Scherberich A (2012) Intraoperative engineering of osteogenic grafts combining freshly harvested, human adipose-derived cells and physiological doses of bone morphogenetic protein-2. Eur Cells Mater 24:308–319
Acknowledgments
This work was supported by the Ministry of Education, Science and Technological Development of the Republic of Serbia, Grant No. III41017.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cvetković, V.J., Najdanović, J.G., Vukelić-Nikolić, M.Đ. et al. Osteogenic potential of in vitro osteo-induced adipose-derived mesenchymal stem cells combined with platelet-rich plasma in an ectopic model. International Orthopaedics (SICOT) 39, 2173–2180 (2015). https://doi.org/10.1007/s00264-015-2929-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2929-x