Abstract
Purpose
The purpose of this study was to determine the efficacy of surgical and conservative treatment in the prevention of recurrence after primary patellar dislocation.
Methods
Studies were searched on MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials and CINHAL from their inception to April 2015. All randomized controlled clinical trials comparing surgical versus conservative treatment after first patellar dislocation were included. Primary outcomes were: recurrent dislocation, subluxation, overall instability and subsequent surgery. Secondary outcomes included imaging, and subjective and objective clinical assessment tools. Methodological quality of the studies was assessed using Cochrane Collaboration’s “Risk of Bias” tool. Pooled analyses were reported as risk ratio (RR) using a random effects model. Continuous data were reported as standardized mean difference (SMD) and 95 % confidence intervals (CIs). Heterogeneity was assessed using I².
Results
Nine studies were included in the meta-analyses. Methodological quality of the studies was moderate to low. Meta-analyses showed that surgical treatment significantly reduces the redislocation rate (RR = 0.62; 95% CI = 0.39, 0.98, p = 0.04) and provides better results on Hughston VAS score (SMD = −0.32; 95% CI = −0.61, −0.03; p = 0.03) and running (OR = −0.52; 95% CI = 0.31, 0.88; p = 0.01). Conservative treatment showed less occurrence of minor complications (OR = 3.46; 95% CI = 2.08, 5.77; p = 0.01) and better results in the figure-of-8 run test (SMD = 0.42; 95% CI = 0.06, 0.77; p = 0.02) and in the squat down test (SMD = −0.45; 95% CI = −0.81, −0.10; p < 0.00001). No other significant differences could be found.
Conclusions
Based on the available data, surgical treatment of primary patella dislocation significantly reduces the risk of patella redislocation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute patellar dislocation accounts for 2–3 % of all knee injuries and its incidence is highest in adolescents and active young adult populations [1–3]. Patellar dislocations mainly occur during athletic activity [4], and the most common mechanism of injury is an internal rotation of the femur on a planted foot with a valgus component; however, patellar dislocation can also occur after low-energy trauma in people with predisposing factors [5].
Numerous anatomical risk factors have been identified, such as: patella alta, abnormal patellar morphology, trochlear dysplasia, patellar hypermobility, variations of medial patello-femoral ligament (MPFL) anatomy, generalised ligamentous hyperlaxity, hypoplasia of the vastus medialis obliquus, increased Q angle, increased femoral antiversion, valgus alignment, and tibial external rotation [1, 6–8].
Proper treatment is essential in order to minimize sequelae, such as recurrent dislocation, painful subluxation, and osteoarthritis. Historically, first line option was conservative treatment, except in presence of osteochondral fractures [5, 9]. High recurrence rate and residual symptoms of instability associated with conservative treatment (up to 44 %) [10, 11] led to increased indication to surgical treatment, and more than 100 different arthroscopic or open surgical techniques have been described in the literature to address patellar instability [12]. However, management of primary patellar dislocation is still a matter of debate. The purpose of the present systematic literature review was to determine the efficacy of surgical and conservative treatment in the prevention of recurrent instability after first patellar dislocation.
Materials and methods
This systematic review was conducted following the guidelines provided by the Cochrane Handbook [13] and according to the PRISMA guideline [14].
Eligibility criteria
All randomized and quasi-randomized (method of allocating participants to a treatment which is not strictly random, e.g., by date of birth, hospital record number, or alternation) level I and II controlled clinical trials that enrolled people of any age with primary patellar dislocation and compared any surgical treatment versus any conservative treatment were included in the study. Only published data on peer review journals were considered.
Exclusion criteria were non-randomized comparative studies, reviews, case series, expert opinions editorial pieces, and randomized trials enrolling patients with the following conditions: previous major knee injuries, previous knee surgeries, primary patella dislocation and concomitant ligament and/or meniscal injuries needing treatment, and primary patella dislocation exclusively treated by fixation of osteochondral fractures.
The diagnosis of patellar dislocation was based on the following criteria: presence of locked acute dislocation; typical clinical findings (haemarthrosis, pain on palpation of medial parapatellar structures and femoral epicondyle, and positive apprehension sign); magnetic resonance imaging (MRI) findings of effusion, medial retinacular injury, osteochondral lesions and loose bodies; dislocatable patella during examination under anaesthesia; and arthroscopic evidence of medial retinacular injury.
Surgical treatments included both open and arthroscopic MPFL repair or reconstruction, lateral retinacular release (LRR) and extensor mechanism realignment procedures. Conservative treatment strategies following patellar dislocation included bracing or splinting, manual therapy, exercise-based rehabilitation, education and advice, electrotherapeutic modalities and taping techniques.
Primary outcomes of the present review were: recurrent patellar dislocation, recurrent patellar subluxation, overall instability (combination of redislocation, subluxation and minor symptoms of instability, such as giving way), and subsequent surgery. Secondary outcomes were any other outcome measurements reported by each included study.
Search strategy
Studies were identified by searching electronic databases. There were no restrictions on the date of publication or the language. This search was applied to MEDLINE (1948 to April 2015), and adapted for EMBASE (1988 to April 2015), Cochrane Central Register of Controlled Trials and CINHAL (1982 to April 2015). See Appendix for the MEDLINE search strategy.
Data management
Two review authors independently selected eligible trials from title and abstract. Subsequently, they analysed the full text to confirm the inclusion in the study and extracted the data using a piloted form. Titles of journals, names of authors or supporting institutions were not masked at any stage. No attempt was made to contact trialists regarding trial methodology and findings. Disagreements at any stage of the review process were resolved by consensus or a third party adjudication. Where possible, the data were pooled and a meta-analysis was performed. Incomplete data (e.g., means without standard deviation) could not be used and were excluded from meta-analysis.
Quality appraisal
The methodological quality of included studies was assessed, independently and without masking, by two review authors using The Cochrane Collaboration’s “Risk of Bias” tool [13]. This tool incorporates assessment of randomization (sequence generation and allocation concealment), blinding (participants, personnel and outcome assessors), completeness of outcome data, selection of outcomes reported and other sources of bias. According to the above assessment, the risk of bias was categorized as low, unclear or high for each of the included studies.
Statistical analysis
Meta-analysis was performed by using RevMan 5.3.5 software from the Cochrane Collaboration [15].
Dichotomous data were reported as risk ratio (RR) using a random effects model. Continuous data were reported as standardized mean differences (SMD) and 95 % confidence intervals (CIs). Ordinal data were reported as generic inverse variance. Subjective outcomes were dichotomized (good/poor results). Fixed and random effects models were compared as appropriate, according to the results of heterogeneity tests and finally a random effects model was chosen because the estimates were similar.
Only the subsets of the data matching review’s inclusion criteria were extracted and included in the analysis. In this review, conservative treatment was considered as the control intervention.
Heterogeneity was assessed using I² for each meta-analysis. According to the guidelines provided by the Cochrane Handbook for Systematic Reviews of Interventions, heterogeneity was considered not important between 0 and 40 %; moderate between 30 and 60 %; substantial between 50 and 90 % and considerable between 75 and 100 % [14]. Therefore, an I² of less than 60 % was the cut off for homogeneity of the data, justifying pooling.
Results
Search strategy
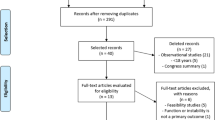
The electronic search resulted in 221 hits, 88 for Medline, 71 for Embase, 43 for CINHAL and 19 for Cochrane. After removing the duplicates, 152 studies remained. Of these, 137 were excluded based on their abstract and one additional study was excluded based on the full text article. Nine studies were included in the review (Fig. 1). We found two studies published by the same authors [16, 17]. The authors reassessed the same patients at longer follow-up by questionnaire and therefore, when possible, we included in the review only the last follow-up.
Study characteristics
All nine studies finally selected for the review were published in English [16–24]. Study characteristics are summarized in Table 1.
A total of 430 knees were included. Time between injury and treatment was less than 14 days in three studies [17, 19, 21] up to three weeks in one study [22], less than one month in one study [20] and 50 days on average in one study [18]. Only two studies [23, 24] did not report the time between injury and treatment.
Conservative treatment was similar in all of the selected studies, consisting of bracing for two to six weeks and an early rehabilitation. Only one study [23] reported no rehabilitation program after brace removal. Most of the studies [16–19, 21] included patients who underwent diagnostic arthroscopy and/or arthroscopic loose body removal in the conservative treatment. Moreover, in one study [18] arthroscopic osteochondral fragment refixation was performed before treatment allocation, and both treatment arms had one patient who underwent refixation.
Surgical treatment included many different techniques: open or arthroscopic repair of medial retinaculum (suture, duplication, adductor magnus augmentation, femoral reinsertion of MPFL), reconstruction of MPFL with patellar tendon, Roux-Goldthwait procedure, and LRR.
Quality appraisal
The methodological quality of the eligible trials was moderate to low. All the studies had one or more limitations in study design (Fig. 2).
Risk of bias summary. Authors’ judgment about each risk of bias item from each of the studies included according to the Cochrane Collaboration’s “Risk of Bias” tool. a The figure presents all the judgments in a cross-tabulation of studies. b The figure illustrates author’s judgment as a percentage across all studies included (green low risk, yellow unclear, red high risk)
Only five studies showed a correct random sequence generation [18, 20–23]. Nikku et al. [16, 17] and Palmu et al. [19] based randomization and allocation on year of birth (even/odd). Regalado et al. [24] did not describe the method used to generate the allocation sequence. Evaluators and participants were not blinded in all the included studies. The majority of the studies also displayed inconsistencies, such as difference in baseline data between groups, lack of analysis of predictors, small sample size or underpowered design.
Primary outcomes
Redislocation was assessed in all the studies included. Four hundred thirty knees (230 and 200 underwent surgical and conservative treatment, respectively) were available for meta-analysis, which showed a significantly greater redislocation rate in the conservative group (RR = 0.62; 95% CI = 0.39, 0.98, p = 0.04). Heterogeneity was moderate (I² = 51 %, χ² = 14.16, df = 7, p = 0.05) (Fig. 3).
For subluxation, 239 knees were evaluated in four studies [17, 20–22] (125 and 114 underwent surgical and conservative treatment, respectively). No significant difference was observed in the subluxation rate between the two treatments (RR = 0.54; 95% CI = 0.18, 1.60, p = 0.26). Meta-analysis showed a moderate heterogeneity (I² = 45 %, χ² = 5.41, df = 3; p = 0.14) (Fig. 4).
Overall instability was analysed on 259 knees (137 and 122 underwent surgical and conservative treatment, respectively) from five studies [17, 20–23]. Meta-analysis showed no significant difference in the rate of overall instability between surgical and conservative treatment, albeit the CI was very narrow and shifted in favour of surgical treatment (RR = 0.39; 95% CI = 0.14, 1.11; p = 0.08). Heterogeneity was very high (I² = 80 %, χ² = 20.40, df = 4; p = 0.0004) (Fig. 5a). After a retrospective assessment of heterogeneity, two studies were identified as different from the others [17, 23]. Exclusion of these studies removed the statistical heterogeneity and affected the result of meta-analysis. Surgical treatment showed significantly better results than conservative treatment with a narrow CI (RR = 0.13; 95% CI = 0.04, 0.46; p = 0.001; I² = 10 %) (Fig. 5b). The study by Nikku et al. [17] had a large sample size (53 % of total knees included in this comparison) with a high prevalence of overall instability (73 % of total number of episodes), but it was judged at high risk of bias on account of sequence generation and allocation; in fact, gender distribution was different in the two groups, with higher prevalence of females in the surgical group. The study by Petri et al. [23] was also considered as high risk of bias because the outcome “instability” was not specified in the method section. Moreover, the meaning of “episode of instability” was not addressed in the manuscript. Finally, the study was underpowered as recognized by the authors.
Two hundred fifty-nine knees (138 and 121 underwent surgical and conservative treatment, respectively) from four studies [16, 19, 21, 24] were evaluated for subsequent surgery. No significant difference was observed at meta-analysis between surgical and conservative treatment (RR = 0.98; 95% CI = 0.53, 1.83; p = 0.95). Heterogeneity was low (I² = 35 %, χ² = 4.59, df = 3; p = 0.20) (Fig. 6).
Secondary outcomes
The reported secondary outcomes varied between the included studies (Table 2).
Surgical treatment showed significantly better results than conservative treatment on evaluation of mean Hughston VAS score and running. On the contrary, analysis of performance tests (figure-of-eight run and squat-down test) showed significantly better results after conservative treatment. Minor complications (superficial nerve injuries, superficial wound infection, dermatitis of surgical dressing, cosmetically unsatisfactory scars and early loss of motion) occurred more frequently in the surgical group with a statistically significant difference. There was no significant difference between the two treatment arms with respect to the following outcomes: subjective results, Kujala score, Lysholm score, Tegner activity score, subjective assessment of pain and functional knee limitation (except for running), KOOS, pre-injury activity level, radiological findings, clinical exam and major complications. The assessment of Kujala score and Tegner activity score showed a considerable heterogeneity with I² values of 82 and 75 %, respectively. After conducting a retrospective assessment of heterogeneity, two of the studies that analysed the Kujala score were different from the others [20, 22]. They both showed significant differences between the two groups in favour of surgical treatment. However, both studies had sample size and included older patients (range, 12–74 years). Moreover, the study by Bitar et al. [22] differed from the others for surgical treatment, as it consisted of MPFL reconstruction, while other authors reported MPFL repair. This might be another clinical reason for heterogeneity. Excluding these studies removed statistical heterogeneity, but did not affect finding of no evidence of significant difference between the two treatment arms (SMD = 0.20; 95% IC = −0.11, 0.52; p = 0.20; I² = 0 %).
A retrospective assessment of heterogeneity was also conducted for Tegner activity score. Both studies [16, 19] included in the meta-analysis were judged at high risk of bias on account of sequence generation and allocation. Two other studies [16, 21] reported incomplete data, therefore, they were not included in the meta-analysis.
Discussion
The present systematic literature review and meta-analysis combined data across studies in order to estimate treatment effects after primary patellar dislocation with more precision than was possible in every single study. The principal finding of the present study is that surgical treatment after acute primary patellar dislocation significantly reduces the redislocation rate. On analysing secondary outcomes, surgical treatment also showed better results than conservative treatment on evaluation of mean Hughston VAS score and running. On the contrary, analysis of performance tests (figure-of-eight run and squat-down test) showed significantly better results after conservative treatment. Minor complications were significantly greater in the surgical group.
However, the overall quality of the body of evidence and strength of recommendations for each outcome across studies in the present meta-analysis was moderate because all the included studies showed some weaknesses mainly related to sample size and randomization, with only three studies having reported sample size calculation [18, 19, 24]. Moreover, predisposing factors for acute patellar dislocation (increased Q angle, patella alta, trochlear dysplasia) were not equally distributed in the two treatment arms in most of the studies [16–23], and age and surgical treatments varied across the studies.
Two studies [19, 24] reported exclusively on patients under 16 years and one of those showed lower risk of redislocation and slightly better functional results after surgical treatment [24].
It was not possible to compare efficacy of different surgical interventions for many reasons. Patients were treated with different procedures, ranging from medial reefing to extensor mechanism realignment procedures, and surgical techniques were not always adequately described. The majority of the selected studies [16–21] performed repair of the medial retinaculum in different ways. Only in the study by Bitar et al. [22] did patients undergo MPFL reconstruction, and surgical treatment showed significantly better results on evaluation of redislocation rate and Kujala score.
In three studies [16, 23, 24], some patients underwent isolated LRR. Biomechanical studies [25–28] showed that LRR reduces patellar tilt resulting from a tight lateral retinaculum and increases passive medial and lateral patellar mobility. Therefore, isolated LRR is indicated only to reduce pain secondary to lateral patella hyperpressure, increased patellar tilt (negative passive patellar tilt test), and medial and lateral patellar glide of two quadrants or less without bone abnormalities [29–31]. Several studies have been recently published on this topic: three narrative reviews [32–34], one systematic review without meta-analysis [35], six systematic reviews and meta-analysis [36–41] and one systematic review of overlapping meta-analysis [42], which actually included only four previous meta-analysis [36–38, 40]. It is therefore clear that there is a growing interest around the subject, but at the same time no definitive conclusions have been reached. Reviews without meta-analysis [32–35] recommended conservative treatment except in several specific circumstances, such as presence of osteochondral fractures. On the contrary, recent meta-analysis [37–42], showed that surgical treatment significantly reduces the risk of redislocation. Moreover, surgical treatment was shown to improve Hughston VAS [36–38, 40] and Tegner [38, 39] scores. Two papers [39, 41] also reported higher Kujala score in short term (<5 years) follow-up, while evidence at six to nine years follow-up shifted towards conservative treatment. Finally, only one paper [37] reported higher risk of patellofemoral osteoarthritis after surgical treatment. The main limitations of some of the previous reviews are that non-randomized comparative studies were analysed along with RCTs [37, 40], and also studies reporting outcomes of patients affected by recurrent dislocations were included [37].
The present review updated the previous literature and included only RCTs comparing surgical versus conservative treatment after primary patellar dislocation. Moreover, all the outcomes reported by the included studies were analysed. Nevertheless, the present review has several limitations. First, studies were identified only by searching major electronic databases without looking for hand search or unpublished data. Second, no attempt was made to contact trialists to obtain original study data in case of missing data or unclear findings. Third, no sensitivity analysis was performed due to limited methodological quality of all the included studies. Furthermore, a subgroup analysis according to age or surgical procedure was not possible, due to the limited number of included studies. For the same reason, publication bias was not investigated. Indeed, according to the Cochrane’s recommendations, tests for funnel plot asymmetry should not be used when less than ten studies are included in the meta-analysis because the power of the tests is too low to distinguish chance from real asymmetry [15].
In conclusion, the present meta-analysis showed that surgical treatment significantly reduces the risk of redislocation and provides better results on the evaluation of Hughston VAS and running. Conservative treatment provides significantly lesser risk of minor complications and better results on performance tests (figure-of-eight run and squat-down test).
References
Atkin DM, Fithian DC, Marangi KS et al (2000) Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med 28:472–479
Fithian DC, Paxton EW, Stone ML et al (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32:1114–1121
Merchant ND, Bennett CH (2007) Recent concepts in patellofemoral instability. Curr Opin Orthop 18:153–160
Waterman BR, Belmont PJ Jr, Owens BD (2012) Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg 25:51–57
Aglietti P, Givin F, Cuomo P (2006) Disorders of the patellofemoral joint. Churchill Livingstone Elsevier, London
Larsen E, Lauridsen F (1982) Conservative treatment of patellar dislocations: influence of evident factors on the tendency to redislocation and the therapeutic result. Clin Orthop Relat Res 171:131–136
Mäenpää H, Lehto MU (1996) Patellar dislocation has predisposing factors. Knee Surg Sports Traumatol Arthrosc 4:212–216
de Oliveira V, de Souza V, Cury R et al (2014) Medial patellofemoral ligament anatomy: is it a predisposing factor for lateral patellar dislocation? Int Orthop 38:1633–1639
Cofield RH, Bryan RS (1977) Acute dislocation of the patella: results of conservative treatment. J Trauma 17:526–531
Mäenpää H, Huhtala H, Lehto MU (1997) Recurrence after patellar dislocation. Redislocation in 37/75 patients followed for 6–24 years. Acta Orthop Scand 68:424–426
Mäenpää H, Lehto MU (1997) Patellar dislocation. The long-term results of nonoperative management in 100 patients. Am J Sports Med 25:213–217
Arendt EA, Fithian DC, Cohen E (2002) Current concepts of lateral patella dislocation. Clin Sports Med 21:499–519
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org. Accessed 05 July 2015
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–34
The Cochrane Collaboration (2014) Review Manager (RevMan) [Computer program], version 5.3. The Nordic Cochrane Centre, Copenhagen
Nikku R, Nietosvaara Y, Kallio PE et al (1997) Operative versus closed treatment of primary dislocation of the patella. Similar 2-year results in 125 randomized patients. Acta Orthop Scand 68:419–423
Nikku R, Nietosvaara Y, Aalto K et al (2005) Operative treatment of primary patellar dislocation does not improve medium-term outcome: a 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop 76:699–704
Christiansen SE, Jakobsen BW, Lund B, Lind M (2008) Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy 24:881–887
Palmu S, Kallio PE, Donell ST et al (2008) Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am 90:463–470
Camanho GL, Viegas Ade C, Bitar AC et al (2009) Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy 25:620–625
Sillanpää PJ, Mattila VM, Mäenpää H et al (2009) Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation. A prospective randomized study. J Bone Joint Surg Am 91:263–273
Bitar AC, Demange MK, D’Elia CO, Camanho GL (2012) Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med 40:114–122
Petri M, Liodakis E, Hofmeister M et al (2013) Operative vs conservative treatment of traumatic patellar dislocation: results of a prospective randomized controlled clinical trial. Arch Orthop Trauma Surg 133:209–213
Regalado G, Lintula H, Kokki H et al (2014) Six-year outcome after non-surgical versus surgical treatment of acute primary patellar dislocation in adolescents: a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3271-3
Fulkerson JP, Schutzer SF, Ramsby GR, Bernstein RA (1987) Computerized tomography of the patellofemoral joint before and after lateral release or realignment. Arthroscopy 3:19–24
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26:59–65
Merican AM, Kondo E, Amis AA (2009) The effect on patellofemoral joint stability of selective cutting of lateral retinacular and capsular structures. J Biomech 42:291–296
Bedi H, Marzo J (2010) The biomechanics of medial patellofemoral ligament repair followed by lateral retinacular release. Am J Sports Med 38:1462–1467
Kolowich PA, Paulos LE, Rosenberg TD, Farnsworth S (1990) Lateral release of the patella: indications and contraindications. Am J Sports Med 18:359–365
Lattermann C, Toth J, Bach BR Jr (2007) The role of lateral retinacular release in the treatment of patellar instability. Sports Med Arthrosc 15:57–60
Verdonk P, Bonte F, Verdonk R (2008) Lateral retinacular release. Orthopade 37:884–889
Frosch S, Balcarek P, Walde TA et al (2011) The treatment of patellar dislocation: a systematic review. Z Orthop Unfall 149:630–645
Petri M, Krettek C, Jagodzinski M (2012) Evidence-based treatment protocol to manage patellar dislocation. Unfallchirurg 115:387–391
Sillanpää PJ, Mäenpää HM (2012) First-time patellar dislocation: surgery or conservative treatment? Sports Med Arthrosc 20:128–135
Stefancin JJ, Parker RD (2007) First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res 455:93–101
Hing CB, Smith TO, Donell S, Song F (2011) Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Database Syst Rev 11, CD008106
Smith TO, Song F, Donell ST, Hing CB (2011) Operative versus non-operative management of patellar dislocation. A meta-analysis. Knee Surg Sports Traumatol Arthrosc 19:988–998
Cheng B, Wu X, Ge H et al (2014) Operative versus conservative treatment for patellar dislocation: a meta-analysis of 7 randomized controlled trials. Diagn Pathol 9:60
Yao LW, Zhang C, Liu Y et al (2015) Comparison operative and conservative management for primary patellar dislocation: an up-to-date meta-analysis. Eur J Orthop Surg Traumatol 25(4):783–788. doi:10.1007/s00590-014-1523-z
Zheng X, Kang K, Li T et al (2014) Surgical versus non-surgical management for primary patellar dislocations: an up-to-date meta-analysis. Eur J Orthop Surg Traumatol 24:1513–1523
Smith TO, Donell S, Song F, Hing CB (2015) Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Database Syst Rev 2, CD008106
Erickson BJ, Mascarenhas R, Sayegh ET et al (2015) Does operative treatment of first-time patellar dislocations lead to increased patellofemoral stability? A systematic review of overlapping meta-analyses. Arthroscopy 31(6):1207–1215. doi:10.1016/j.arthro.2014.11.040
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Database: Ovid MEDLINE(R) <1948 to April Week 1 2015>
Search Strategy: ------------------
1 patellar dislocation/
2 patella.tw.
3 (first adj7 dislocat$).tw.
4 and/2–3
5 (acute adj3 dislocat$).tw.
6 and/2,5
7 (patella$ adj3 (dislocat$ or lux$)).tw.
8 1 or 4 or 6 or 7
9 randomized controlled trial.pt.
10 controlled clinical trial.pt.
11 randomized.ab.
12 placebo.ab.
13 drug therapy.fs.
14 randomly.ab.
15 trial.ab.
16 groups.ab.
17 or/9–16
18 (animals not (humans and animals)).sh.
19 17 not 18
20 and/8,19
Rights and permissions
About this article
Cite this article
Saccomanno, M.F., Sircana, G., Fodale, M. et al. Surgical versus conservative treatment of primary patellar dislocation. A systematic review and meta-analysis. International Orthopaedics (SICOT) 40, 2277–2287 (2016). https://doi.org/10.1007/s00264-015-2856-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2856-x