Abstract
Purpose
The goal of this study is to compare the characteristics, clinical course, and mortality rates of acetabular fractures in the elderly population with respect to two types of injury.
Methods
We reviewed 183 consecutive patients with acetabular fractures aged 60 years old and older. One hundred eighty-three patients (129 men and 54 women) were included in the study with an average age of 70.2 years. There were 186 fractures, which included three cases of bilateral fractures. Patients were divided into two groups: low-energy injuries (group I), 56, and high-energy injuries (group II), 130. Patient characteristics and fracture pattern, as well as in-hospital mortality rates were compared between the low-energy and high-energy groups.
Results
Patient demographics and comorbidities were significantly different between the groups. In group I, the average age was 74.9 years, versus 68.2 years in group II (p < 0.001). The percent of females in each group was 39.3 % and 24.6 %, respectively (p = 0.043), and the average body mass index (BMI) was 25.6 and 28.4, respectively (p = 0.001). The Charlson comorbidity index was higher in group I (1.98 vs 0.95 in group II, p < 0.001). However, the American Society of Anesthesiologists physical status (ASA) was similar between groups (2.56 vs 2.53, respectively, p = 0.808). The proportion of surgical treatment was 44.6 % in group I and 61.6 % in group II (p = 0.019). Group II had a longer hospital stay (10.4 days vs 14.5 days, p = 0.025), but in-hospital death was not significantly different (5.3 % vs 7.9 %, respectively, p = 0.567).
Conclusion
Patients with acetabular fractures resulting from low-energy injuries were older and had lower BMI with more comorbidities. This study may highlight characteristics of fragility fractures of the acetabulum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acetabular fractures in the elderly represent the fastest growing type of fracture in this population [1]. This is due to the prolonged life expectancy, continued automobile use, and active lifestyle in today’s modern society. As defined by the World Health Organization in 1998, a “fragility fracture” is one caused by a mechanism that would be insufficient to fracture a normal, healthy bone [2]. The majority of reports on fragility fractures have focused on the proximal femur, vertebrae and wrist [3–8]. There is a paucity of literature that considers acetabular fractures in the elderly as a fragility fracture.
There have been several studies on acetabular fractures in elderly populations. However, these studies have included both high-energy and low-energy acetabular fractures in elderly patients, and there have been no studies comparing acetabular fractures resulting from low-energy and high-energy mechanisms. Because fragility fractures of the acetabulum should occur only from low-energy injuries or without trauma [9], the previously described acetabular fracture characteristics in elderly patients should be re-assessed to see if they still hold true in cases of low-energy fragility fractures.
Therefore, we conducted a retrospective descriptive study comparing two different types of acetabular fractures: those resulting from low-energy mechanisms, and the others from high-energy mechanisms. The aim of this study was to compare the characteristics, clinical course, fracture pattern, and mortality rates of acetabular fractures in the elderly population with respect to these two different mechanisms.
Patients and methods
The medical records of patients who presented with acetabular fractures between 2001 and 2012 were retrospectively extracted from an institutionally approved, single-centre orthopedic database. The inclusion criteria were patients with acetabular fractures, aged 60 years or older. The exclusion criteria were pathologic fractures, prisoners, or patients pronounced dead on arrival at the emergency room. Data regarding age, sex, body mass index (BMI), mechanism of injury, comorbidities using the Charlson comorbidity index (CCI) [10] and American Society of Anesthesiologists (ASA) physical status classification [11] were evaluated. The reviewed clinical course involved hospital stay, in-hospital death, and treatment methods. Treatment methods were categorized into non-operative or surgical treatment; surgical treatment was subdivided into minimally invasive surgery, open reduction and internal fixation (ORIF), and arthroplasty. Displacement of each fracture was measured and the fracture pattern was classified using Letournel’s classification [12]. Radiologic findings were assessed by an experienced orthopedic surgeon using operative records, radiologic reports, and re-evaluation of pelvis X-ray and/or CT. The PACS system of our institution was established in 2006, so radiologic findings obtained before 2006 were evaluated utilizing only medical records’ review. We defined minimal displacement as being 3 mm or less.
The patients were divided into two groups: low-energy injury (group I) and high-energy injury (group II). Falls from heights of one metre or less were defined as “low-energy mechanism of injury” [13].
All statistical analyses were performed using PASW Statistics version 18.0 (IBM, Armonk, NY, USA). Statistical significance was set at p < 0.05. Patient demographics and fracture characteristics of the two groups were compared using a Chi square test or Fisher’s exact test for categorical variables and independent t-test and Mann-Whitney U test for parametric and non-parametric continuous variables, respectively. For fracture classification, we performed Bonferroni correction to control the familywise error rate [14].
Results
One-hundred eighty-three patients aged 60 years and older treated for acetabular fractures were included in this retrospective data analysis. There were 186 fractures, which included three cases of bilateral fractures. There were 129 men (70 %) and 54 women (30 %), with an average age of 70.2 years (range, 60–96 years).
The most common mechanisms of injury in the study were falls (49.5 %), followed by motor vehicle accidents (29.0 %; Table 1). Low-energy falls occurred in 30.1 % of the patients, while high-energy falls were seen in 19.4 %. There were 56 cases in group I, with an average age of 74.9 years (range, 60–96 years); 39.3 % of which were women (Table 2). Group II had 130 cases, with an average age of 68.2 years (range, 60–88 years); 24.6 % of which were women. The average BMI was 25.6 in group I and 28.4 group 2 (p = 0.001). The CCI was higher in group I than in group II (1.98 vs 0.95, p < 0.001), but the ASA scores were similar between the two groups (2.56 vs 2.53, respectively, p = 0.808).
The average length of hospital stay was 10.4 days in group I and 14.5 days in group II, with a significant difference between these two groups (p = 0.025). In group I, three patients (5.3 %) died, at an average of 6.7 days (range, five to ten days) after injury, while ten patients (7.9 %) died in group II, at an average of 11.0 days (range, one to 26 days) after injury. The rate of in-hospital death was not significantly different (p = 0.567).
In total, 81 cases (43.5 %) were treated non-operatively, while 105 cases (56.5 %) were treated surgically. Ninety-four patients underwent ORIF, while ten underwent percutaneous screw fixation and one underwent arthroplasty. In comparison, 44.6 % of patients in group I underwent surgical management, while 61.6 % in group II were treated operatively (p = 0.019). In group I, there were 20 cases (35.7 %) of ORIF, four cases (7.1 %) of percutaneous screw fixation and one case (1.8 %) of arthroplasty. In group II, ORIF was performed in 74 cases (57.0 %) and percutaneous screw fixation was performed in six cases (4.6 %).
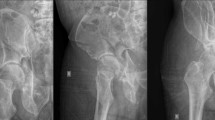
As shown in Table 3, the most common fracture pattern in each group was a both-column fracture (25.0 % vs 21.5 %, respectively). In group I, an anterior column with posterior hemitransverse fracture pattern was the second most common (19.6 %), followed by anterior column (17.9 %) and T-type (14.3 %) patterns. An anterior column fracture pattern was the second most common in group II (18.5 %), but the percentage was similar to that seen in group I. Posterior wall fracture patterns were the third most common (16.9 %) in group II, while they only accounted for 1.8 % of those in group I. The fracture patterns were different between the two groups (p < 0.001). With Bonferroni correction, the frequency of fracture patterns in group I was significantly different from group II. In group I, anterior column with posterior hemitransverse fractures were the most common (p = 0.009), and the second commonest was posterior wall fracture (p = 0.040). A total of 54 cases involved minimally displaced fractures, with 19 cases (33.9 %) in group I and 35 cases (26.9 %) in group II (p = 0.380).
Discussion
Low-energy acetabular fractures occur infrequently (about 4,000 per year in the United States) [1]. A recent epidemiologic study involving 1,309 patients at a Level I trauma center was reported by Ferguson et al. [15]. They noted that the mean age of patients with surgically treated acetabular fractures increased from 32 to 49 years, and that the proportion of patients older than 60 years of age doubled (from 10 % to 24 %). In elderly patients, between 50 % and 83 % of acetabular fractures are caused by simple falls from a standing height, a mechanism common among most fractures of the proximal femur in elderly patients [15, 16]. Ferguson et al. also reported that the most common mechanism of acetabular injuries in the elderly was from a fall (49.8 %), but they did not distinguish between low and high-energy falls. In this study, a fall, too, was shown to be the most common mechanism of injury (49.5 %). However, closer analysis of our data reveals that only 61 % of these falls (which is just 30 % of all the reported injuries) were the result of low-energy mechanisms.
In our study, the low-energy injury group was characterized by older average age, higher percentage of females, and lower BMI; these characteristics are all consistent with risk factors associated with fragility fractures [17]. Females are at a higher risk for sustaining a fragility fracture [17], as the incidence of hip fractures in women in the US is three times that of men [18]. This concept was challenged by the study of Ferguson et al. [15], which revealed a constant male-to-female ratio regardless of age, with male predominance independent of age. Ferguson et al.’s study also found a male predominance in elderly acetabular fractures. However, these findings are in contrast to our results, which more closely mirror what would be expected in fragility fractures. Our results showed a higher percentage of women in the low-energy injury group compared with the high-energy injury group. We believe that our result supports that belief that women are more susceptible to fragility fractures.
It is unclear why the proportion of women with acetabular fractures is lower than that found in hip fractures, as the mechanism of fragility acetabular fractures is similar to those encountered in hip fractures in the elderly [15, 16]. Most people who suffer a fracture from a fall have fractures along the proximal femur, but it may be possible that acetabular fragility fractures occur in a subset of patients where the force is directed and transmitted to the acetabulum. Considering that fractures from falls are much higher in women, there should be an expected increase in the percentage of women with fragility acetabular fractures when compared with younger patients.
We used two methods to evaluate comorbidity: the CCI and the ASA. The CCI was derived using a population of medical patients and has been shown to be a reliable and valid predictor of mortality in a number of populations, including hospital inpatients and the critically ill [19, 20]. Alternatively, the ASA is often used to judge pre-existing diseases in a patient, regardless of whether this impact was caused by one or several disease processes [11]. Therefore the CCI does not reflect injury state, while the ASA can reflect the influence of trauma. In this study, the CCI was found to be higher in group I, whereas the ASA was similar in both groups. Therefore, we conclude that patients with fragility fractures had more previous medical co-morbidities, but the physical state after injury was similar. This may explain the lack of differences between the two groups for in-hospital mortality.
In this study, one year mortality was not measured, but in-hospital mortality was 5.3 % in the low-energy group and 7.9 % in the high-energy group. The in-hospital mortality in group I was similar to that of patients with hip fractures, with previously reported in-hospital mortality of 4.5-5.5 % [21, 22]. Bible et al. [23] reported that the one year mortality was 8.1 % in the isolated acetabular fracture group versus 23.3 % in non-isolated fractures, and mortality at 30 days was 2.3 % and 17.8 % respectively. However, the conclusions reached from this are limited, as the results do not represent the mortality rate of those who sustained acetabular fragility.
A number of researchers described the findings commonly seen in elderly acetabular fractures; these include involvement of the anterior column, quadrilateral-plate, anterocentral region (with displacement/dislocation of femoral head), and the dome (resulting in marginal impaction and the Gull sign) [24]. Anterior column displacement occurs in 64 % of cases in elderly patients, compared with only 43 % in younger patients with acetabular fractures [15]. Using Letournel’s classification system, the most common fracture pattern is the anterior column/anterior wall, with the second most common being the anterior column posterior hemitransverse pattern with medial protrusion of the femoral head [25, 15]. This study revealed that 70 % of low-energy fractures involved the anterior column; anterior column/wall, both column, and anterior column posterior hemitransverse pattern. The two fracture patterns that differed between the two groups were anterior column with posterior hemitransverse and posterior wall fracture. Our results support the notion that the anterior column combined with posterior hemitransverse fracture pattern represents the typical acetabular fracture in the elderly [25]. Additionally, posterior wall fractures should be expected in higher-energy mechanisms.
This study has several limitations. First, fracture classification was determined utilizing only medical records in 56 cases (30 %) before 2006. While these medical records reporting on fracture classification is reliable, their accuracy can be questioned unless validated by another expert. Second, one year mortality and bone mineral density was not assessed in the analysis between the two groups, as this information would help further classify and stratify the data. Also, because this study was performed at a Level I trauma center with a significant number of patients having high-energy injury, this may have subjected the data to selection bias. Lastly, an additional selection bias may have resulted from the exclusion of data from patients who were pronounced dead. These presumably were from higher-energy mechanisms, and therefore may skew the data reported for the mortality rate and the length of stay.
Conclusion
The results of this study highlight characteristics of fragility acetabular fractures. Elderly patients with acetabular fractures from low-energy injuries were older and had lower BMI with more comorbidities than high-energy injury patients.
References
Mears DC (1999) Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg 7(2):128–141
WHO (1998) Guidelines for preclinical evaluation and clinical trials in osteoporosis. World Health Organization, Geneva
Dell R, Greene D, Schelkun SR, Williams K (2008) Osteoporosis disease management: the role of the orthopaedic surgeon. J Bone Joint Surg Am 90(Suppl 4):188–194. doi:10.2106/JBJS.H.00628
Lin JT, Lane JM (2004) Osteoporosis: a review. Clin Orthop Relat Res 425:126–134
Rowe SM, Yoon TR, Ryang DH (1993) An epidemiological study of hip fracture in Honam, Korea. Int Orthop 17(3):139–143
Carretta E, Bochicchio V, Rucci P, Fabbri G, Laus M, Fantini MP (2011) Hip fracture: effectiveness of early surgery to prevent 30-day mortality. Int Orthop 35(3):419–424. doi:10.1007/s00264-010-1004-x
Khan MA, Hossain FS, Ahmed I, Muthukumar N, Mohsen A (2013) Predictors of early mortality after hip fracture surgery. Int Orthop 37(11):2119–2124. doi:10.1007/s00264-013-2068-1
Saracen A, Kotwica Z (2014) Treatment of multiple osteoporotic vertebral compression fractures by percutaneous cement augmentation. Int Orthop 38(11):2309–2312. doi:10.1007/s00264-014-2470-3
Rosa MA, Maccauro G, D’Arienzo M (1999) Bilateral acetabular fracture without trauma. Int Orthop 23(2):120–121
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47(11):1245–1251
American Society of Anesthesiologists. ASA Physical Status Classification System. Available at: http://asahq.org/resources/clinical-information/asa-physical-status-classification-system
Letournel E (1980) Acetabulum fractures: classification and management. Clin Orthop Relat Res 151:81–106
Bergstrom U, Bjornstig U, Stenlund H, Jonsson H, Svensson O (2008) Fracture mechanisms and fracture pattern in men and women aged 50 years and older: a study of a 12-year population-based injury register, Umea, Sweden. Osteoporos Int 19(9):1267–1273. doi:10.1007/s00198-007-0549-z
Chuang-Stein C, Tong DM (1995) Multiple comparisons procedures for comparing several treatments with a control based on binary data. Stat Med 14(23):2509–2522
Ferguson TA, Patel R, Bhandari M, Matta JM (2010) Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br 92(2):250–257. doi:10.1302/0301-620X.92B2.22488
Vanderschot P (2007) Treatment options of pelvic and acetabular fractures in patients with osteoporotic bone. Injury 38(4):497–508. doi:10.1016/j.injury.2007.01.021
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19(4):385–397. doi:10.1007/s00198-007-0543-5
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB (2009) Incidence and mortality of hip fractures in the United States. JAMA 302(14):1573–1579. doi:10.1001/jama.2009.1462
Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW (1996) Can comorbidity be measured by questionnaire rather than medical record review? Med Care 34(1):73–84
Poses RM, McClish DK, Smith WR, Bekes C, Scott WE (1996) Prediction of survival of critically ill patients by admission comorbidity. J Clin Epidemiol 49(7):743–747
Belmont PJ Jr, Garcia EJ, Romano D, Bader JO, Nelson KJ, Schoenfeld AJ (2014) Risk factors for complications and in-hospital mortality following hip fractures: a study using the National Trauma Data Bank. Arch Orthop Trauma Surg 134(5):597–604. doi:10.1007/s00402-014-1959-y
Frost SA, Nguyen ND, Black DA, Eisman JA, Nguyen TV (2011) Risk factors for in-hospital post-hip fracture mortality. Bone 49(3):553–558. doi:10.1016/j.bone.2011.06.002
Bible JE, Wegner A, McClure JM, Kadakia RJ, Richards JE, Bauer JM, Mir HR (2013) One-year mortality after acetabular fractures in elderly patients presenting to a level-one trauma center. J Orthop Trauma 28(3):154-159. doi:10.1097/BOT.0b013e31829e801b
Ferguson TA, Patel R, Bhandari M, Matta JM (2010) Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg (Br) 92(2):250–257. doi:10.1302/0301-620X.92B2.22488
Culemann U, Holstein JH, Kohler D, Tzioupis CC, Pizanis A, Tosounidis G, Burkhardt M, Pohlemann T (2010) Different stabilisation techniques for typical acetabular fractures in the elderly—a biomechanical assessment. Injury 41(4):405–410. doi:10.1016/j.injury.2009.12.001
Conflicts of interest
The authors declare no conflict of interest in relation to the preparation of this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, J.W., Herbert, B., Hao, J. et al. Acetabular fractures in elderly patients: a comparative study of low-energy versus high-energy injuries. International Orthopaedics (SICOT) 39, 1175–1179 (2015). https://doi.org/10.1007/s00264-015-2711-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2711-0