Abstract
To estimate the effect of delay to surgery for hip fracture on 30-day mortality using a risk adjustment strategy to control for the effect of demographic and clinical confounders. This observational study was carried out on all patients admitted with a hip fracture and discharged between January 2004 and December 2007 from a teaching hospital. Gender, age, time to surgery, mortality and medical comorbidities were derived from hospital discharge records (SDO), while International Normalised Ratio (INR) and American Society of Anaesthesiologists (ASA) score were retrieved from clinical records. Backward stepwise logistic regression was used to identify potential confounders in the relationship between time to surgery and mortality. A final multivariate logistic regression analysis was carried out controlling for the effect of confounders. In the 1320 patients who underwent surgery (mean age = 83 years, % female = 76.8%), time to surgery was two days or less in 746 (56.5%) patients and 30-day mortality was 3.5%. The interventions included partial or total hip replacement (N=820, 62.1%) and reduction and internal fixation (N=500, 37.9%). Multivariate logistic regression analysis showed that patients with a time to surgery greater than two days had a 2-fold increase in 30-day mortality after adjusting for age, gender, and comorbidity (OR=1.992, 95% CI 1.065-3.725). In a second model also including ASA score the odd ratio decreased to 1.839 (95% CI 0.971-3.486). Patients with a hip fracture should have surgery within two days from admission in order to reduce 30-day mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In-hospital mortality in patients admitted for hip fracture ranges between 2% and 24% [1–3], whereas mortality for any cause after one year from the event is reported to range between 14 and 36% [4] and may depend on the health and functional status before fracture [5, 6].
New Zealand and Scottish guidelines for the management of hip fracture [7, 8] recommend that surgery be performed within 24 hours of the fracture event in order to decrease postoperative mortality. However, such recommendations are graded only as C and are based on case control or cohort studies (see for instance [9, 10]) with a moderate probability that the relationship between time to surgery and mortality is causal [8].
Although two Italian studies failed to demonstrate a relationship between timing of surgery and postoperative mortality [11, 12], the meta-analysis by Shiga et al. [13] showed that if surgery is performed more than 48 hours after the fracture event, there is an expected 41% increase in mortality (within 30 days of fracture) and a 32% increase in mortality at one year. This finding strongly supports the importance of early intervention after hip fracture. Medical or system-related reasons may account for operative delay, including the number of available theatre sessions and the volume of trauma work faced by the hospital [13].
Two studies based on the Scottish Hip Fracture Audit emphasised the importance of the case mix over timing of surgery in determining postoperative mortality [14, 15]. In fact, healthy individuals who sustain a hip fracture undergo surgery shortly after the event, whereas most patients with an unstable or deteriorated clinical status have to undergo a more thorough preoperative evaluation as well as a possible correction of some fundamental parameters, such as anaemia or electrolyte imbalance, before surgery.
Lastly, a systematic review of 52 published studies failed to identify a clear relationship between timing of surgery and mortality rate, but suggested that a procedure performed within 48 hours of the fracture event can shorten hospital stay and decrease the complication rate [16]. A recent study showed that time from hospital admission to surgery can be reliably used as a surrogate of the actual time from fracture to surgery when studying hip fracture mortality [17].
In view of the ongoing controversy on this topic, many authors are calling for new studies to specifically address whether delaying surgery beyond 48 hours from the event of fracture is in fact an independent risk factor for higher mortality [18] and the extent to which the relationship between timing of surgery and mortality is accounted for by the case mix. In addition to demographic and clinical characteristics, process variables may account for surgical delay and play a role in the causal chain leading to mortality, for instance, the time necessary to optimise patient’s medical conditions and the availability of the operating theatre [19].
The aim of this study was to analyse the relationship between timing of surgery for hip fracture (over two days) and mortality within 30 days of the event in patients discharged between January 2004 and December 2007 from a teaching hospital in Italy, using a risk adjustment strategy to control for the potential confounding effects of demographic and clinical variables.
Patients and methods
The study population included all patients over the age of 65 years with primary or secondary ICD codes of hip fracture (ICD-9 CM codes 820 and 821) that underwent partial or total hip replacement, reduction and internal fixation (ICD-9 CM codes 81.51, 81.52, 79.05, 79.15, 79.25, 79.35, 79.45, 79.55) and were discharged between January 1, 2004 and December 31, 2007 from the Unit of Orthopaedics and Traumatology of a teaching hospital in Italy. In order to exclude repeated admissions for existing hip fractures, we did not include patients that had a hip fracture or a hip replacement in the previous two years. We chose a four-year period in order to be able to detect a difference of 3% in 30-day mortality between patients with time to surgery under two and over two days, by setting the power at ≥80% and alpha level at 0.05.
Regional hospital discharge records were used to retrieve ICD-9 CM (International Classification of Disease, 9th revision) diagnostic codes, admission and discharge dates, date and type of intervention, demographic characteristics, and comorbidities at the index admission and in the previous three years in any hospital of the region.
There are several reasons for surgical delay, including the time necessary to optimise patient’s medical conditions, for example, in patients undergoing anticoagulation treatment [20] or suffering from anaemia and requiring transfusion. In principle, relatively healthy patients (American Society of Anaesthesiologists [ASA] grades I and II) undergo surgery sooner than patients who require more preoperative evaluation and preparation. Therefore, we gathered from patients’ records the INR, haemoglobin (HB) and the ASA score (as recorded by the consultant anaesthesiologist at the time of surgery).
ASA scores classify patients as healthy patient (grade I), patient with mild systemic disease but with no functional limitation (grade II), patient with severe systemic disease and with definite functional limitation (grade III), a patient with severe systemic disease that is a constant threat to life (grade IV), and a dying patient who is not expected to survive for 24 hours with or without surgery (grade V) [21]. There were no grade V patients.
Time to surgery was calculated as the difference between the admission date and the operation date, and subsequently dichotomised as two days or under and over two days.
In order to allow for the potential confounding role of the day of admission, we recoded the variable using three categories: Monday-Tuesday-Wednesday, Thursday-Friday and Saturday-Sunday. This was done because findings from the literature suggest that the availability of operating theatre or of the surgeon according to the week day has an impact on the delay of surgery [19].
The outcome of interest, mortality within 30 days of surgery, was obtained through record linkage of the hospital discharge records and the regional mortality register data. We choose 30-day mortality instead of in-hospital mortality because the latter may be affected by discharge policies.
Moreover, we chose a four-year period in order to be able to detect a difference of 3% in 30-day mortality between patients with time to surgery ≤2 and >2 days, by setting the power at ≥80% and the alpha level at 0.05.
Statistical analysis
The relationship between time to surgery and 30-day mortality was analysed compensating for the effect of potential confounders. To this purpose, an empirical risk adjustment model was built in three steps: first, comorbidities with a frequency >3% in the study population were selected; second, collinearity of independent variables including comorbidities, gender, age and week day of admission, ASA, INR and Hb was examined; and third, variables identified in these steps were included in backward logistic regression models (probability for removal 0.10) with mortality as the dependent variable.
Two models were fit, one including data retrieved from discharge records (N = 1,320), the second also including data retrieved from patient charts (complete data available for 1,261 cases).
In the first model, independent variables included gender, age, type of intervention, week day, and relevant comorbidities identified and empirically tested [22] (arrhythmia and heart disease including ischemic heart disease, complex heart disease, rheumatic heart disease, other heart diseases), other chronic diseases (liver, pancreas, intestine), chronic obstructive pulmonary disease (COPD), dementia, diabetes, lipid metabolism disorder, hemiplegia and paralysis, hypertension, cerebrovascular disease, haematological disease, renal failure, obesity, Parkinson’s disease, cancer, previous myocardial infarction and vascular disease. In the second model, ASA score, INR and Hb level were also included. The Hosmer-Lemeshow test was used as goodness of fit index and the pseudo-R2 Nagelkerke index was used to measure the strength of association between the independent variables and mortality.
In order to identify possible effect modifiers, we examined the effect of the interaction between each variable of interest and time to surgery on mortality in separate logistic regression models. The final multivariate logistic regression model included all variables significantly associated with mortality and all significant interactions. Statistical analyses were carried out using SAS 9.1 (SAS Institute, Cary, NC).
Results
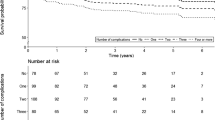
Out of the 1,377 patients discharged with a diagnosis of hip fracture, 1,320 (95.8%) underwent surgery and were included in the analyses. The study population included mainly female patients (N = 1014, 76.8%) and had a mean age of 83 years (standard deviation [SD] = 7.0) (Table 1). The interventions included partial or total hip replacement (N = 820, 62.1%) and reduction and internal fixation (N = 500, 37.9%). Thirty-day mortality was 3.5% (N = 46). Surgery was performed after a median of two days (Fig. 1). Of the 46 patients who died after surgery, 18 died before two days and 28 after two days. Time to surgery over two days predicted a two-fold increased 30-day mortality (4.9% vs. 2.4%, χ2 = 5.8, p = 0.0155, OR = 2.07, 95% CI 1.14–3.79).
Identification of confounders and risk-adjusted mortality
Model 1
Comorbidities at the index and previous admissions with a frequency >3% are provided in Table 2. In the first backward logistic regression model, age, male gender, arrhythmia and cerebrovascular diseases at the index admission and diabetes, hypertension and renal diseases in the previous admissions were associated with 30-day mortality (Table 3) and were retained in the model. The week day of admission was unrelated to mortality. The Hosmer-Lemeshow test denoted a good model fit (H-L χ2 = 9.283, p = 0.319) and the Nagelkerke r-square of 0.142 indicated that the independent variables accounted for about 14% of the variability of mortality.
When we examined the impact on mortality of the interaction between each variable retained in the model and time to surgery using logistic regression models, none of these interactions were significant. Therefore, we included in the final model only the main effects. In this model, patients with a time to surgery greater than two days had two-fold increased 30-day mortality after adjusting for age, gender and comorbidity (OR = 1.992, 95% CI = 1.065–3.725) (Table 3). The Hosmer-Lemeshow test denoted a good model fit (H-L χ2 = 4.153, p = 0.843) and the Nagelkerke r-square was 0.155.
Model 2
In the second logistic regression model, age, male gender, ASA score, and arrhythmia at the index admission, and diabetes, hypertension and renal diseases recorded in the previous admissions were significantly associated with 30-day mortality. INR and Hb and cerebrovascular disease were excluded from the model by the backward procedure. After adjusting for confounders, the association between delayed surgery and 30-day mortality approached statistical significance (OR = 1.839, 95% CI 0.971–3.486, p = 0.06) (Table 2). The Hosmer-Lemeshow test denoted a good model fit (H-L χ2 = 5.715, p = 0.679) and the Nagelkerke r-square was 0.171.
Discussion
Existing guidelines [7, 8] indicate that surgical delay has a negative impact on in-hospital death. However, the effect of this delay on patient mortality is controversial and variations across studies may depend on failure to adjust for confounding variables or on the adjustment for different variables [16].
Our study contributes additional evidence to this ongoing debate. The gender ratio of three females to one male in our sample is consistent with that reported by Bjorgul and Reikerås [23] for prospectively registered Norwegian cases. We found a significant association between delayed surgery and 30-day mortality. The unadjusted odds ratio was 2.07, 95% CI 1.14–3.79, and the odds ratio adjusted for age, gender and significant comorbidities was slightly decreased (OR = 1.992, 95% CI 1.065–3.725). In a second multivariate logistic regression model taking the ASA score into account, the odds ratio still denoted an excess mortality that approached statistical significance (OR = 1.839, 95% CI 0.971–3.486). Our results differ from previous studies carried out in Italy [11, 12] and from a study based on the German nationwide quality registry [24], where the outcome was in-hospital mortality. However, our results are consistent with the conclusion of the meta-analysis of Shiga et al. [13].
Our study was carried out in a teaching hospital where 95% of the patients underwent surgery for hip fracture and more than 50% were operated upon within two days after admission. This denotes a good performance compared to a recent report from the United Kingdom [25]. Our 30-day mortality was 3.5%, which again indicates a good performance compared to other studies [11, 12] and is consistent with results from US hospitals [3].
One strength of our study is the use of potential confounding variables derived both from administrative databases and clinical records. Of the variables derived from clinical records only ASA score was associated with 30-day mortality, and INR and Hb were not. While the ASA scoring system has been criticised as a measure of clinical severity for its subjective nature, in some studies it proved to be a powerful predictor of mortality after hip fracture [14]. Our results confirm that the ASA score is associated with an excess mortality and is therefore a potential confounder to be taken into account in risk adjustment models.
Our results should be interpreted whilst keeping in mind that the model including the ASA score was based on the subset of 1,261 patients for whom the information was available from clinical records. Therefore, the power to detect a significant difference in mortality in patients undergoing surgery after two days was decreased. An additional reason for a decrease in power is that the difference of 2.5% in mortality rate in patients operated upon before or after two days was lower than expected. The post-hoc power of our study was 61%.
A second limitation is that the data came from a single hospital, which may limit the general application of findings. However, this weakness allows elimination of a source of variability related to hospital organisation and procedures. Moreover, although we included a number of demographic and clinical covariates in the models to account for patient differences, some unmeasured characteristics may affect the risk of mortality. For instance, Barone et al. [22] reported that low socioeconomic level was associated with increased mortality and with a lower risk of early intervention after controlling for other demographic and clinical confounders. This suggests that disadvantaged people may have a differential access to care, despite the universal healthcare coverage in Italy.
In conclusion, we argue that clinical and organisational efforts should be directed to decreasing the time to surgery keeping in mind that undue delay may compromise the surgical benefit.
As the most recent guidelines underscore [7, 8], patient flow logistical and appropriate management of medical conditions may be crucial to make hospitals more patient-centred and to improve patient outcomes.
References
Nather A, Seow CS, Iau P, Chan A (1995) Morbidity and mortality for elderly patients with fractured neck of femur treated by hemiarthroplasty. Injury 26(3):187–190
Formiga F, Lopez-Soto A, Sacanella E, Coscojuela A, Suso S, Pujol R (2003) Mortality and morbidity in nonagenarian patients following hip fracture surgery. Gerontology 49(1):41–45
Hannan EL, Magaziner J, Wang JJ, Eastwood EA, Silberzweig SB, Gilbert M, Morrison RS, McLaughlin MA, Orosz GM, Siu AL (2001) Mortality and locomotion 6 months after hospitalization for hip fracture: risk factors and risk-adjusted hospital outcomes. JAMA 285(21):2736–2742
Zuckerman JD (1996) Hip fracture. N Engl J Med 334(23):1519–1525
Hamlet WP, Lieberman JR, Freedman EL, Dorey FJ, Fletcher A, Johnson EE (1997) Influence of health status and the timing of surgery on mortality in hip fracture patients. Am J Orthop 26(9):621–627
Jamal Sepah Y, Umer M, Khan A, Ullah Khan Niazi A (2010) Functional outcome, mortality and in-hospital complications of operative treatment in elderly patients with hip fractures in the developing world. Int Orthop 34(3):431–435
New Zealand Guidelines Group (2003) Acute management and immediate rehabilitation after hip fracture amongst people aged 65 years and over. Wellington, NZ. http://www.nzgg.org.nz/guidelines/0007/Hip_Fracture_Management_Fulltext.pdf. Accessed 11 Mar 2010
Scottish Intercollegiate Guideline Network (2009) Management of hip fracture in older people. A national clinical guideline. http://www.sign.ac.uk/guidelines/fulltext/111/index.html. Accessed 21 Jul 2009
Grimes JP, Gregory PM, Noveck H, Butler MS, Carson JL (2002) The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med 15;112(9):702–709
Siegmeth AW, Gurusamy K, Parker MJ (2005) Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br 87(8):1123–1126
Franzo A, Francescutti C, Simon G (2005) Risk factors correlated with post-operative mortality for hip fracture surgery in the elderly: a population-based approach. Eur J Epidemiol 20(12):985–991
Gini R, Capon A, Roti L, Mastromattei A, Buiatti E (2007) Femur fractures among elderly in Lazio and Tuscany regions from 1999 to 2003. Epidemiol Prev 31(4):197–203
Shiga T, Wajima Z, Ohe Y (2008) Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth 55(3):146–154
Holt G, Smith R, Duncan K, Finlayson DF, Gregori A (2008) Early mortality after surgical fixation of hip fractures in the elderly: an analysis of data from the Scottish hip fracture audit. J Bone Joint Surg Br 90(10):1357–1363
Holt G, Smith R, Duncan K, Hutchison JD, Gregori A (2008) Outcome after surgery for the treatment of hip fracture in the extremely elderly. J Bone Joint Surg Am 90(9):1899–1905
Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ (2009) Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury 40(7):692–697
Vidal EI, Moreira-Filho DC, Coeli CM, Camargo KR Jr, Fukushima FB, Blais R (2009) Hip fracture in the elderly: does counting time from fracture to surgery or from hospital admission to surgery matter when studying in-hospital mortality? Osteoporos Int 20(5):723–729
Bryson GL (2008) Waiting for hip fracture repair—do outcomes and patients suffer? Can J Anaesth 55(3):135–139
Charalambous CP, Yarwood S, Paschalides C, Siddique I, Hirst P, Paul A (2003) Factors delaying surgical treatment of hip fractures in elderly patients. Ann R Coll Surg Engl 85(2):117–119
White RH, McKrittick T, Hutchinson R et al (1995) Temporary discontinuation of therapy; changes in the international normalized ratio. Ann Intern Med 122:40–42
Owens WD, Felts JA, Spitznagel EL Jr (1978) ASA physical status classifications: a study of consistency of ratings. Anesthesiology 49:239–243
Barone AP, Fusco D, Colais P, D’Ovidio M, Belleudi V, Agabiti N, Sorge C, Davoli M, Perucci CA (2009) Effects of socioeconomic position on 30-day mortality and wait for surgery after hip fracture. Int J Qual Health Care 21(6):379–386
Bjørgul K, Reikerås O (2007) Incidence of hip fracture in southeastern Norway: a study of 1,730 cervical and trochanteric fractures. Int Orthop 31(5):665–669
Smektala R, Hahn S, Schräder P, Bonnaire F, Schulze Raestrup U, Siebert H, Fischer B, Boy O (2009) [Medial hip neck fracture: influence of pre-operative delay on the quality of outcome: results of data from the external in-hospital quality assurance within the framework of secondary.] Unfallchirurg Sep 12. [Epub ahead of print]
Marsland D, Chadwick C (2009) Prospective study of surgical delay for hip fractures: impact of an orthogeriatrician and increased trauma capacity. Int Orthop Oct 17. [Epub ahead of print] doi:10.1007/s00264-009-0868-0
Acknowledgement
This study was funded with a grant from the Research Program ‘Regione-Universita’ 2007–2009 of the Region Emilia-Romagna.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carretta, E., Bochicchio, V., Rucci, P. et al. Hip fracture: effectiveness of early surgery to prevent 30-day mortality. International Orthopaedics (SICOT) 35, 419–424 (2011). https://doi.org/10.1007/s00264-010-1004-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1004-x