Abstract
Purpose
The aim of the study was to analyse greater tuberosity’s (GT) micro-vascularization in the context of rotator cuff tear and to identify factors that could affect the rate and distribution of micro-vessels.
Methods
Eighty-seven patients with supraspinatus and/or infraspinatus tendon tears were included in a prospective study. Mean age at surgery was 58 years (41–78) and clinical symptoms were lasting from an average of 20 months before surgery. A bone core of 1-cm depth was obtained from the GT during rotator cuff repair at two localizations, medial and lateral within tuberosity. Micro-vascularization was then analysed with an immunohistochemistry technique based on CD34 antigen tracking endothelial cells at two levels of depth for each sample (more and less than 5 mm). Epidemiologic and pathologic data were correlated with the rate of micro-vascularization measured.
Results
Median rate of GT’s micro-vascularization was 9.8 %, which ranged from 0.13 % to 33.4 %. This rate decreased with preoperative steroid injection (7.4 % vs 11.2) and with localization close to the cartilage of the humeral head (8.7 % vs 11.9 %). However, it remains almost homogenous along the depth’s core. Moreover, no significant correlation was found regarding age at surgery, gender, context of previous trauma, smoking habits, duration of symptoms, and specific data regarding the tendon tear.
Conclusions
This study highlighted the variability of GT’s micro-vascularization in case of rotator cuff tear. A greater rate was observed at the lateral part of the footprint, whereas medical history of steroid injection has a negative influence on micro-vascularization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Healing of rotator cuff tendons after repair remains problematic and improvement of healing rate is of ongoing investigation [1–5]. The strongest mechanical fixations of the tendons to bone have been shown to be correlated to better tendon healing. Indeed, quality of sutures, type of anchorage and surgical repair technique are more and more reliable [6]. However, two weak links remain of concern and are predictable of the anatomical result of the repair: the quality of the musculo-tendinous unit and the quality of the bone at the reinsertion site [7]. Fatty infiltration index, muscle atrophy and tendon retraction are reported to be major prognostic factors [7, 8]. The mechanical value of the bone seems also to be implied, as much as its biological value [9–15]. It has been demonstrated that initiation of the healing process of the tendon onto the bone are related to bone marrow-derived cells coming from the footprint, which differentiate into tendon tissues [9, 11, 12, 14, 16]. Therefore, micro-vascularity of the greater tuberosity (GT) could reflect the biological potential of the bone in cases of rotator cuff repair involving the supraspinatus and/or the infraspinatus tendons. To our knowledge, no study to date has investigated the micro-vascularization at the footprint in case of rotator cuff tear.
The aim of the study was to analyse the micro-vascularization of the GT in the context of rotator cuff tear and to identify factors that could affect its rate and distribution. Our hypothesis was that micro-vascularity at the GT was variable, depending on epidemiological data and the type of rotator cuff tendon tear.
Methods
Study design and patients
A prospective study was conducted in our department from January 2011 to January 2012 after being approved by the institutional review board. Inclusion criteria were: all patients who were operated for suprapsinatus and/or infraspinatus tendons tears after a failed conservative treatment, with an open or arthroscopic surgical technique, and who gave their agreement to enter the study. Exclusion criteria were: lack of preoperative MRI or arthro-CT scans focused on rotator cuff tendon (stage of retraction and muscle fatty infiltration), a subscapularis tear without involvement of supra or infraspinatus tendon, and a bone sample quality that did not allow a valuable immunohistochemical analysis.
One hundred three patients were consecutively enrolled in this study during the period of inclusion. Two of them were excluded because of an isolated subscapularis tendon tear and two others because of incomplete radiologic data; 12 bone samples were inadequate for biological analysis, leaving 87 patients (87 samples), who were available for statistical analysis.
Patients
Among the 87 patients, there were 43 men and 44 women with a mean age of 58 (range, 41–78). Twenty-four (27 %) patients were tobacco smokers and 16 had other arteriosclerosis risk factors such as diabetes, hypertension, obesity and hypercholesterolemia. Steroid injection in sub acromial space had been used preoperatively in 20 patients (23 %).
Clinical symptoms were of 20 months (range, one to 126) duration before surgery. Thirty-three patients (38 %) described a traumatic event as the beginning of their shoulder symptoms.
Tissue collection and preparation
Two senior surgeons performed surgery according to a standardized technique: subacromial decompression, biceps tenotomy or tenodesis and rotator cuff repair in anatomic position. The tendon was fixed with transosseous Mason-Allen non-absorbable sutures or lateral tension band anchorage during, respectively, open and arthroscopic surgery [17].
One bone sample (a core) was obtained from each patient during the surgical procedure using 8-gauge diameter trocars (Jamshidi®, Carefusion, USA) inserted perpendicular to the exposed footprint of the GT at the rotator cuff site and before abrasion of the bone with a burr. Two localisations in the middle zone were investigated in a randomized design selection: close to the cartilage of the humeral head (medial footprint-group M) or at the top of the GT (lateral footprint- group L). A bone core of 1-cm depth obtained from each patient was immediately sent to the Pathology Department in a hydrated compress for specific fresh analysis.
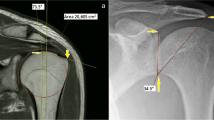
Bone sections were obtained from paraffin-embedded blocks. Immunohistochemistry analysis was performed with an anti-CD34 antibody (clone QBEnd10, 1:100 dilution; Beckman Coulter, Marseille, France), which is a specific tracker of endothelial cells and micro-vessels, widely used in tumour vascularity characterization [18, 19]. Slides were processed automatically (Autostainer link 48; Dako, Courtaboeuf, France) according to the protocols supplied by the antibody manufacturers (Fig. 1).
After slides scanning (NanoZoomer; Hamamatsu, Massy, France), vascular structures labelled with anti-CD34 antibody were quantified using the imaging software NDP.view 2.3.1 (Hamamatsu) and NIS elements Basic Research 2.30 (Nikon, Champigny sur Marne, France) at the same scale (Fig. 2). The micro-vascularization resulted from the ratio automatically calculated between vascular structures’ area and miscellaneous structures’ area (trabecular bone, fat interstitial tissue, stromal cells, etc.). This relation was studied at two levels of depth for each sample: less than 5 mm (level 1) and more than 5 mm from the top of the core (level 2).
Statistical analysis
Univariate comparisons were performed to study the relationship between micro-vascularization and others variables such as demographic factors (age, sex), clinical history (smoker, arteriosclerosis risk factors, history of traumatic event or steroid injections) and pathological data (number of tendons involved, stage of tendon retraction and fatty degeneration index of the muscle, shape of acromion according to Bigliani classification). Median and interquartile-range (IQR) were given for GT’s microvacularization. For categorical variables, we used Wilcoxon or Kruskal-Wallis nonparametric comparison tests and, for continuous variables, we calculated the Pearson’s correlation coefficient. We considered statistical significance reached when p-value <0.05. Analyses were conducted using Stata software v11.1.
Results
Data distribution was not normal and ranged from 0.13 % to 33.4 %. Median rate of GT’s micro-vascularization was 9.8 % (mean, 11.5; SD, 7.8; IQR, 5.5-16.2) (Fig. 3).
There was no significant difference in the micro-vascularization rate at different depths of the bone cores: level 1 was 9.49 % (IQR 0.18–36.5) and level 2 was 9.91 % (IQR 0.09–50.63) (p = 0.56). The micro-vascularization rate tended to be higher at the lateral footprint than at the medial footprint, respectively, 11.9 % (IQR 6.2–18.0) and 8.7 % (IQR 4.3–14.5) (p = 0.16).
No statistically significant correlation was identified according to demographic characteristics, i.e. age at surgery or duration of symptoms did not seem to affect micro-vascularization. However, patient population with previous steroid injection trended to have a lower rate of micro-vascularization (7.4 % vs 11.2 %; p = 0.13) (Table 1).
No significant correlation was found between bone micro-vascularization and type of rotator cuff tendon tears, fatty degeneration index and acromion shape (Table 2).
Discussion
To our knowledge, this is the first study which has investigated the bone biological patterns at the GT with a reproducible technique of measurement of micro-vascularization based on anti-CD34 antibodies, which is commonly used to assess angiogenesis in human solid tumours [17, 18]. The rate of the micro-vascularization at the footprint has been shown to be highly variable from less than 1 % to more than 33 % of tissue, with a median rate of 9.8 %, in the context of rotator cuff tendon tears. This rate was almost homogenous at any level of depth into the GT (in the limits of 10 mm in depth). However, micro-vascularization tended to decrease with steroid injection performed before surgery. Bone close to the humeral head cartilage (medial footprint) had a lower rate of vascularization than at the top of the GT (lateral footprint). No significant statistical correlation has shown relationship between micro-vascularization and age at surgery, gender, context of previous trauma, smoking habits or others arteriosclerosis risk factors, number of torn tendons, stage of retraction or fatty degeneration index and duration of symptoms.
Many authors have investigated prognosis factors that could influence the healing process in case of rotator cuff tendon repair, including epidemiologic and histo-morphometric features [7, 19–24]. Therefore, the success of tendon healing seems to depend on patient’s age, comorbidities, the tendon itself (quality, tear size, degree of retraction) and the muscle (fatty degeneration index and atrophy). Bone quality at the site of tendon insertion remains likely a major component as well, but few studies have investigated this link of the healing process. Biologically, cells coming from the footprint initiate the healing process [12, 14]. However, no significant difference could be shown in our study regarding the micro-vascularization at any depth of the GT. It seems from these results that bone spongialization could not be required for the footprint preparation before tendon anchorage. On the other hand, radiofrequency burning of the footprint commonly performed before tendon anchorage could result in damaging micro-vessels and should be avoided if possible [25]. Mechanically, it has been previously reported that an optimal fixation of the tendon is related to a higher healing rate, and that double row techniques using heavy sutures and anchors seem to improve tendon healing [4–6, 26]. However, fixations of the tendon seem to be better at the border of the articular surface, where the medial row is commonly placed [27–29]. Several authors have pointed out that bone density decreases in case of rotator cuff disease, which could affect bone stock distribution at the GT [10, 15, 30, 31]. According to this study, the tendency of greater micro-vascularization at the top of the GT is an argument for application of the tendon as lateral as possible onto the footprint. Doing so, the double row technique should offer some guarantees with respectively strong medial anchorage and lateral application for a better healing combining theoretical mechanical and biological advantages [5]. However, implications of double row techniques on clinical outcomes at follow-up remain controversial to date [26].
Our study supported that subacromial corticosteroid injections may play a role in lowering micro-vascularization’s rate at the GT. These injections were known to induce adverse effects on the tendon structure [32–34]. In case of rotator cuff tear, corticosteroids directly impregnate the GT and could induce apoptosis of endothelial cells, as it has been shown in cases of femoral head osteonecrosis [35].
Limitations
This study has several weaknesses. There was no control group, with intact rotator cuff tendons, to validate normal bone micro-vascularization at the GT. Indeed, a control-group was ethically difficult to obtain in order to get bone samples in a healthy patient population. On the other hand, the number of patients included was low and did not allow us to perform multivariate analysis. Because of the lack of data in the literature, we could not perform evaluation of the number of subjects required based on a specific difference we wished to stress; this could explain in part the lack of statistical significance detection according to the confidence interval in some variables analyses. Furthermore, only two sites were explored at the supraspinatus footprint: the lateral footprint at the top of the GT and the medial footprint, close to the humeral head cartilage. An intermediary site could have been sampled but it would have decreased the contact bone/tendon area during the repair with an adverse affect on tendon healing onto the GT.
Conclusions
This study has shown that the rate of micro-vessels is variable and ranged from 1 % to about 33 % at GT, with a median rate of 9.8 %. Previous corticosteroid injections seem to lower this rate. Greater vascularisation was found close to the top of the GT, at the lateral footprint. Further investigations are necessary to understand how quality and quantity of micro-vessels could influence tendon healing after rotator cuff repair.
References
Kovacevic D, Rodeo SA (2008) Biological augmentation of rotator cuff tendon repair. Clin Orthop Relat Res 466:622–633
Oh JH, Chung SW, Kim SH, Chung JY, Kim JY (2014) 2013 Neer award: effect of the adipose-derived stem cell for the improvement of fatty degeneration and rotator cuff healing in rabbit model. J Shoulder Elbow Surg 23:445–455
Schaer M, Schober M, Berger S, Boileau P, Zumstein MA (2012) Biologically based strategies to augment rotator cuff tears. Int J Shoulder Surg 6:51–60
Xu C, Zhao J, Li D (2014) Meta-analysis comparing single-row and double-row repair techniques in the arthroscopic treatment of rotator cuff tears. J Shoulder Elbow Surg 23:182–188
Chen M, Xu W, Dong Q, Huang Q, Xie Z, Mao Y (2013) Outcomes of single-row versus double-row arthroscopic rotator cuff repair: a systematic review and meta-analysis of current evidence. Arthroscopy 29:1437–1449
Denard PJ, Burkhart SS (2013) The evolution of suture anchors in arthroscopic rotator cuff repair. Arthroscopy 29:1589–1595
Chung SW, Oh JH, Gong HS, Kim JY, Kim SH (2011) Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med 39:2099–2107
Chung SW, Kim JY, Kim MH, Kim SH, Oh JH (2013) Arthroscopic repair of massive rotator cuff tears: outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med 41:1674–1683
Caplan AI (2009) Why are MSCs therapeutic? New data: new insight. J Pathol 217:318–324
Cadet ER, Hsu JW, Levine WN, Bigliani LU, Ahmad CS (2008) The relationship between greater tuberosity osteopenia and the chronicity of rotator cuff tears. J Shoulder Elbow Surg 17:73–77
Hirose K, Kondo S, Choi HR, Mishima S, Iwata H, Ishiguro N (2004) Spontaneous healing process of a supraspinatus tendon tear in rabbits. Arch Orthop Trauma Surg 124:374–377
Kida Y, Morihara T, Matsuda K et al (2013) Bone marrow-derived cells from the footprint infiltrate into the repaired rotator cuff. J Shoulder Elbow Surg 22:197–205
Kirchhoff C, Braunstein V, Milz S et al (2010) Assessment of bone quality within the tuberosities of the osteoporotic humeral head: relevance for anchor positioning in rotator cuff repair. Am J Sports Med 38:564–569
Uhthoff HK, Seki M, Backman DS, Trudel G, Himori K, Sano H (2002) Tensile strength of the supraspinatus after reimplantation into a bony trough: an experimental study in rabbits. J Shoulder Elbow Surg 11:504–509
Waldorff EI, Lindner J, Kijek TG et al (2011) Bone density of the greater tuberosity is decreased in rotator cuff disease with and without full-thickness tears. J Shoulder Elbow Surg 20:904–908
Gamradt SC, Gallo RA, Adler RS et al (2010) Vascularity of the supraspinatus tendon three months after repair: characterization using contrast-enhanced ultrasound. J Shoulder Elbow Surg 19:73–80
Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG (2005) Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am 87:1229–1240
Frank RE, Saclarides TJ, Leurgans, Speziale NJ, Drab EA, Rubin DB (1995) Tumor angiogenesis as a predictor of recurrence and survival in patients with node-negative colon cancer. Ann Surg 222:695–699
Maschio LB, Madallozo BB, Capellasso BA et al (2014) Immunohistochemical investigation of the angiogenic proteins VEGF, HIF-1α and CD34 in invasive ductal carcinoma of the breast. Acta Histochem 116:148–157
Mallon WJ, Misamore G, Snead DS, Denton P (2004) The impact of preoperative smoking habits on the results of rotator cuff repair. J Shoulder Elbow Surg 13:129–132
Robinson PM, Wilson J, Dalal S, Parker RA, Norburn P, Roy BR (2013) Rotator cuff repair in patients over 70 years of age: early outcomes and risk factors associated with re-tear. Bone Joint J 95:199–205
Wu XL, Briggs L, Murrell GA (2012) Intraoperative determinants of rotator cuff repair integrity: an analysis of 500 consecutive repairs. Am J Sports Med 40:2771–2776
Namdari S, Donegan RP, Chamberlain AM, Galatz LM, Yamaguchi K, Keener JD (2014) Factors affecting outcome after structural failure of repaired rotator cuff tears. J Bone Joint Surg Am 96:99–105
Plate JF, Brown PJ, Walters J et al (2014) Advanced age diminishes tendon-to-bone healing in a rat model of rotator cuff repair. Am J Sports Med 42:859–868
Ficklscherer A, Loitsch T, Serr M et al (2014) Does footprint preparation influence tendon-to-bone healing after rotator cuff repair in an animal model? Arthroscopy 30:188–194
Millett PJ, Warth RJ, Dornan GJ, Lee JT, Spiegl UJ (2014) Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg 23:586–597
Kirchhoff C, Braunstein V, Milz S et al (2012) Age and gender as determinants of the bone quality of the greater tuberosity: a HR-pQCT cadaver study. BMC Musculoskelet Disord 13:221
Tingart MJ, Apreleva M, Lehtinen J, Zurakowski D, Warner JJ (2004) Anchor design and bone mineral density affect the pull-out strength of suture anchors in rotator cuff repair: which anchors are best to use in patients with low bone quality? Am J Sports Med 32:1466–1473
Yamada M, Briot J, Pedrono A et al (2007) Age- and gender-related distribution of bone tissue of osteoporotic humeral head using computed tomography. J Shoulder Elbow Surg 16:596–602
Meyer DC, Fucentese SF, Koller B, Gerber C (2004) Association of osteopenia of the humeral head with full-thickness rotator cuff tears. J Shoulder Elbow Surg 13:333–337
Oh JH, Song BW, Lee YS (2014) Measurement of volumetric bone mineral density in proximal humerus using quantitative computed tomography in patients with unilateral rotator cuff tear. J Shoulder Elbow Surg 23:993–1002
Dean BJ, Franklin SL, Murphy RJ, Javaid MK, Carr AJ (2014) Glucocorticoids induce specific ion-channel-mediated toxicity in human rotator cuff tendon: a mechanism underpinning the ultimately deleterious effect of steroid injection in tendinopathy? Br J Sports Med 48(22):1620–1626
Lee HJ, Kim YS, Ok JH, Lee YK, Ha MY (2013) Effect of a single subacromial prednisolone injection in acute rotator cuff tears in a rat model. Knee Surg Sports Traumatol Arthrosc. Jan 31 [Epub ahead of print]
Tillander B, Franzén LE, Karlsson MH, Norlin R (1999) Effect of steroid injections on the rotator cuff: an experimental study in rats. J Shoulder Elbow Surg 8:271–274
Kerachian MA, Séguin C, Harvey EJ (2009) Glucocorticoids in osteonecrosis of the femoral head: a new understanding of the mechanisms of action. J Steroid Biochem Mol Biol 114:121–128
Author information
Authors and Affiliations
Corresponding author
Additional information
IRB approval: approved study on number 17-0313.
Rights and permissions
About this article
Cite this article
Bonnevialle, N., Bayle, X., Projetti, F. et al. Variations of the micro-vascularization of the greater tuberosity in patients with rotator cuff tears. International Orthopaedics (SICOT) 39, 371–376 (2015). https://doi.org/10.1007/s00264-014-2628-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2628-z