Abstract
Purpose
A variety of bone substitutes have been successfully used to fill PEEK cages in cervical interbody fusion in order to avoid the complications related to bone harvesting from the donor site. However, no controlled study has previously been conducted to compare the effectiveness of PEEK interbody cages containing calcium sulphate/ demineralized bone matrix (CS/DBM) with autogenous cancellous bone for the treatment of cervical spondylosis. The objective of this prospective, randomized clinical study was to evaluate the effectiveness of implanting PEEK cages containing CS/DBM for the treatment of cervical radiculopathy and/or myelopathy.
Methods
Sixty-eight patients with cervical radiculopathy and/or myelopathy were randomly assigned to receive one- or two-level discectomy and fusion with PEEK interbody cages containing CS/DBM or autogenous iliac cancellous bone (AIB). The patients were followed up for two years postoperatively. The radiological and clinical outcomes were assessed during a two-year follow-up.
Results
The mean blood loss was 75 ± 18.5 ml in the CS/DBM group and 100 ± 19.6 ml (P < 0.01) in the AIB group. The fusion rate was 94.3 % in the CS/DBM group and 100 % in the AIB group at 12-month follow-up. The fusion rate was 100 % at final follow-up in both groups. No significant difference (P > 0.05) was found regarding improvement of JOA score and segmental lordosis as well as neck and arm pain at all time intervals between the two groups. The total complication rate was significantly higher (P < 0.05) in the AIB group than in the CS/DBM group, but there was no significant difference between the two groups (P > 0.05) when comparing the complications in the neck.
Conclusions
In conclusion, the PEEK interbody fusion cage containing CS/DBM or AIB following one- or two-level discectomy had a similar outcome for cervical spondylotic radiculopathy and/or myelopathy. The rate of fusion and the recovery rate of JOA score between the two groups were the same. The filling of CS/DBM in the PEEK cage instead of AIB has the advantage of less operative blood loss and fewer complications at the donor site.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the classic techniques for anterior cervical interbody fusion were introduced by Cloward [1] and Smith and Robinson [2] in the 1950s, anterior cervical discectomy and fusion (ACDF) has been developed and become a standard operative procedure for cervical degenerative disc disease associated with radiculopathy or myelopathy. The goal of interbody fusion is to restore the physiological height of intervertebral space and the lordosis of cervical spine after removal of the offending disc and osteophytes. Tri-cortical autologous iliac crest bone grafts are the gold standard grafts used for creating bony fusion between the two vertebrae. However, the incidence of painful complications, including wound infection, haematoma, chronic pain, increased blood loss and operation time, cutaneous nerve neuroma, and pelvic fracture, could reach as high as 24 % [3].
Therefore, the development of alternative grafts and instrumentation techniques are widely studied [4]. Polyetheretherketone (PEEK) interbody cages filled with cancellous bone provide initial stability and require less structural bone graft. The cages prevent graft collapse and restore disc space height and cervical lordosis [5]. The union rate is similar to a tricortical iliac crest bone graft [6]. In order to avoid the complications related to bone harvesting from the donor site, bone substitute such as cancellous allograft [7], tricalcium phosphate [8], biphasic calcium phosphate [9], demineralized bone matrix [10], mineralized collagen [11], and demineralised bone matrix combined with bone morphogenic protein [12] have been successfully used to fill in the cages in the cervical interbody fusion.
Calcium sulphate (CS) is one bone substitute occupying a unique position in the universe of biomaterials. It has been used in clinical practice for a long time and is widely recognized as a biocompatible material with applications in bone regeneration. CS pellets have been successfully used as an implantable filler in the treatment of periodontal bone defects [13] and long bone defects [14]. However, CS is significantly inferior to autologous iliac crest bone despite the addition of bone marrow aspirate when they are used in one-level lumbar posterolateral fusion [15]. Demineralized bone matrix (DBM) has been shown to have an osteoconductive and osteoinductive potential [16–20] because of the proteins and various growth factors present in the extracellular matrix. The CS/DBM composite graft has been successfully used as graft extender in the treatment of large osteonecrotic lesions of the femoral head [14]. To our knowledge, there has been little study on its biological effect in cervical interbody fusion. Therefore, the present study was carried out to compare the effectiveness of PEEK interbody cages containing CS/DBM with autogenous cancellous bone for the treatment of cervical spondylosis with radiculopathy and/or myelopathy.
Materials and methods
Patient population
This study was carried out with the approval of the Committee of Medical Ethics and the Institutional Review Board of our hospital. The informed consent of each patient and his or her family was signed. Between January 2006 and December 2008, a consecutive series of 68 patients were included in the study. There were 36 men and 32 women with mean age of 55.4 years (range 35–68 years). All the patients suffered from cervical degenerative disc disease and complained of progressive upper extremity radicular symptoms and/or myelopathy. The symptoms had lasted for at least six months (range six to 25 months) before the operation. The conservative therapy lasted at least for three months and failed. One- to two-level discectomy and interbody fusion with PEEK cage at contiguous levels from C3–4 to C6–7 were performed for soft disc herniation or spondylosis. The exclusion criteria were as follows: more than two levels of developmental cervical stenosis; significant comorbidities associated with poor general health such as active infection, metabolic disease, severe osteoporosis, gross obesity; smokers which might interfere with the fusion process; continuous or combined ossification of the posterior longitudinal ligament; prior cervical spine surgery; any major psychological problem; claim of Worker Compensation. When a patient was included, the patient was given a registration number and was allocated randomly to one of the groups by computer, either the CS/DBM group or the autogenous iliac cancellous bone (AIB) group. The patients’ demographic characteristics are listed in Table 1.
Surgical techniques
General inhalation anaesthesia was used in all patients. The operations were performed by a senior spine surgeon. Standard right side anterior Smith–Robinson approach was chosen as the surgical procedure. After the exposure the segment was identified by the C-arm fluoroscope. The disc space was opened and distraction was applied using a Caspar distractor. The disc, posterior longitudinal ligament, and osteophytes, including the posterior part of the uncinate process were removed. The upper and lower endplates were well prepared by removing the overlying cartilage and preserving the hardest subchondral bone. The interbody fusion was performed with PEEK cage (MC+®, LDR, France) containing calcium sulphate/demineralized bone matrix (54 levels in 35 patients) in the CS/DBM group or containing autogenous iliac cancellous bone (53 levels in 33 patients) cages in the AIB group. The cage size was determined by both pre-operative templating and intra-operative evaluation using a trial cage to confirm initial stability. In the CS/DBM group, the inner space of the PEEK cage was impacted with the CS/DBM pellets (OsteoSet®2 DBM, Wright Medical Technologies, Arlington, TN) (Fig. 1). In the AIB group, the cage was filled with autologous iliac cancellous bone harvested from the left anterior iliac crest through a mini-incision. The cages were then gently introduced into the disc space and carefully pushed into a good position with an impactor. After the cage was implanted, anterior fixation was performed with an anterior titanium locked plate (ABC plate, Aesculap, Tuttlingen, Germany). The correct position was checked by anteroposterior and lateral views of plain radiography before wound closure. All patients used a Philadelphia collar for four weeks postoperatively. Neck exercises were initiated four weeks after surgery and a normal activity level was progressively resumed.
Assessment of results
The operation time, blood loss, and duration of hospital stay were recorded. The clinical assessment included the neurological outcomes and the neck and arm pain preoperatively and at discharge, three, six, 12, and 24 months after surgery. The data were collected by an independent observer. The Japanese Orthopedic Association (JOA) scoring system (score range, 0–17) was used to assess the neurological outcomes and the visual analogue index (VAS, 0–10) was used to assess the pain. The recovery rate of JOA score was calculated according to the formula: the recovery rate = [(postoperative score–pre-operative score)/(17–pre-operative score)] × 100 %. The complications at the surgical site including the neck and anterior iliac crest were recorded after the surgery.
The fusion status of the PEEK cage was evaluated radiographically at discharge, six weeks and three, six, 12, and 24 months after surgery. The fine cut computerized tomography scans were performed one year after the surgery. Fusion was defined as the presence of continuous trabecular bone bridges in at least one of the following locations: anterior, within, or posterior to the PEEK cage. Absence of such bridges or the presence of an anterior-posterior discontinuation was classified as non-fusion. Segmental lordosis at the surgical level was measured by Cobb’s angle in order to assess the sagittal alignment. The radiographic analysis was performed by two independent spine surgeons who were blinded to the study and the information of the patients.
Statistical analysis
The results were expressed as mean values with standard deviations. The unpaired Student’s t test or Chi-square test was used for comparison of the results between the two groups, and paired t test or repeated measures ANOVA followed by Newman–Keuls–Student test for comparison of the results between time points. The results were considered significant at a level of P < 0.05.
Results
All patients included in this study were treated as originally randomized. The average operative time was 55 ± 10.5 minutes for one-level and 80 ± 13.8 min for two-level procedures in the CS/DBM group. The average operative time was 70 ± 12.8 minutes for one-level and 100 ± 11.6 minutes for two-level procedures in the AIB group. The operation time was significantly longer in the AIB group than in the CS/DBM group (P < 0.01). The mean blood loss was significantly lower in the CS/DBM group than in the AIB group (75 ± 18.5 vs. 100 ± 19.6 ml, P < 0.01). There was no statistical significance with respect to hospital stay between the two groups (6.5 ± 1.5 vs. 7 ± 1.8 days, P > 0.05). No patient in both groups had undergone a second operation for any reason.
The patients were followed up for two years. One patient for one-level fusion in the CS/DBM group was lost in the six-month follow-up and one patient for two-level fusion in the AIB group was lost in the 12-month follow-up. The average VAS scores of neck pain and arm pain improved significantly (P < 0.01) after the operation both in the CS/DBM group and in the AIB group (Table 2). At the final follow-up, the average improvement rate was 69 % for neck pain and 70 % for arm pain in the CS/DBM group, and 68 % for neck pain and 68 % for arm pain in the AIB group. No significant differences were found between the CS/DBM group and the AIB group at any follow-up time point.
JOA score improved in each case. The pre-operative average JOA score was 12.68 ± 3.05 points in the CS/DBM group and 13.12 ± 2.88 in the AIB group. At final follow-up, the average JOA score improved significantly (P < 0.01) to 16.30 ± 0.78 points in the CS/DBM group and 16.34 ± 0.68 in the AIB group (Table 3). There were no significant differences (P > 0.05) when comparing the JOA scores between the two groups at all time intervals. The recovery rate was 83.8 % in the CS group and 83.0 % in the AIB group.
The mean pre-operative segmental lordotic angle was 2.0 ± 3.7° in the CS/DBM group and 2.3 ± 3.5° in the AIB group. At the final follow-up, the segmental lordotic angle was significantly (P < 0.05) improved to 3.6 ± 2.5° in the CS/DBM group and 3.8 ± 2.4° in the AIB group (Table 4). There was no significant difference (P > 0.05) when comparing the mean segmental lordosis between the two groups at each follow-up point.
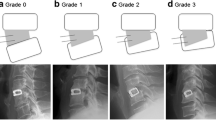
The lateral X-rays showed the regular incorporation of the CS/DBM into new bone with time in the CS/DBM group (Fig. 2a–f). At discharge, the CS/DBM was opaque in the transparent PEEK cage. At six-week follow-up, the density of CS/DBM had decreased and the centre of cage had become nearly transparent. At three-month follow-up, the centre part of the cage was still transparent and no new bone was observed. At six-month follow-up, the density of the centre part had increased, especially in the area close to the upper and lower endplate. At 12-month follow-up, the centre part of the cage was opaque again and new bone had formed in the cage. Sagittal reconstructive images of the CT scan showed that new bone mass bridged the disc space within the cage (Fig. 3a–b). The density had become stable till final follow-up. In the AIB group, the autogeneous bone was opaque on the radiograph and there was no obvious change with time. The fusion rate was 94.3 % (50/53 levels) in the CS/DBM group and 100 % (51/51 levels) in the AIB group at 12-month follow-up. The fusion rate was 100 % at final follow-up in both groups.
The radiological change of cervical spine in a male patient with cervical myelopathy from the calcium sulphate/demineralized bone matrix (CS/DBM) group. a The CS/DBM was opaque in the transparent PEEK cage on the lateral X-ray film one week after the operation. b The density of CS/DBM decreased and the centre of cage became nearly transparent six weeks after the operation. c The centre part of the cage was still transparent and no new bone was observed three months after the operation. d The density of the centre part increased, especially in the area close to the upper and lower endplate six months after the operation. e The centre part of the cage was opaque again and new bone formed in the cage 12 months after the operation. f Two years later, new bone in the centre part of the cage was clearly identified
There was no device-related complication such as hardware loosening and breakage, screw pullout, or displacement of the cage in both groups. There were three minor complications in the CS/DBM group and six in the AIB group. However, no additional surgery was required for any cause in both groups. The complication rate was 8.6 % in the CS group and 18.2 % in the AIB group. The complications in the CS/DBM group included one case of superficial wound infection and two hoarseness, while the complications in the AIB group included two cases of hoarseness, one superficial wound infection in donor site and three chronic pains or regional numbness in donor site. Although the total complication rate was significantly higher (P < 0.05) in the AIB group than in the CS/DBM group, there was no significant difference between the two groups (P > 0.05) when comparing the complication rate in the neck.
Discussion
To our knowledge this is the first randomized prospective study to compare CS/DBM with autogeneous bone in the treatment of cervical degenerative disc disease. The fusion rate and the clinical outcome of the CS/DBM group were similar to the AIB group. The CS/DBM could be substituted by new bone to promote cervical interbody fusion and could be an alternative to autogenous graft.
ACDF is a well-established operative procedure used to treat cervical degenerative disc disease associated with radiculopathy or myelopathy. Sufficient decompression and ultimate solid bony fusion are the prerequisite to a successful procedure [5, 21]. The ideal bone graft should possess three main characteristics: osteoconductivity, osteoinductivity and osteogenicity. Autogenous tricortical bone graft from iliac fulfills the above features. However, donor site problems including chronic pain, infection, and nerve injury had been highlighted at a rate as high as 24 % [3]. Allograft is one of the excellent options. However, the fusion rate is not as high as autograft, and graft collapse has been reported. Moreover, there is the potential transmission of infectious disease [22–24].
In order to solve these problems, interbody fusion cages with different kinds of biomaterials have been developed. Polyetheretherketone (PEEK) is a non-absorbable semicrystalline biopolymer that has been used in a variety of medical devices. It is biocompatible and the modulus of elasticity is similar to the bone [7, 25, 26]. The PEEK cage is radiolucent and new bone within the cage can be observed on the plain X-ray. The titanium marker in the cage makes it easy to be localized by the investigator. The standard X-ray films could be used to assess the fusion process. Pechlivanis et al. [27] reported that the empty PEEK cage without additional filling could be implanted after anterior cervical discectomy. Although fusion status did not influence the clinical outcome, the nonfusion rate was high according to radiologic criteria. The PEEK packed with autogaft or bone substitutes was usually used in cervical interbody fusion. Autogeneous bone is the gold standard fill in the PEEK cage to promote fusion. Cho et al. [28] compared the autograft-filled PEEK cage with tricortical autograft in the cervical interbody fusion. The results showed that the radiological fusion rate was higher in the PEEK group (100 %) than in the autograft group (93 %) and the complication rate was much higher in the autograft group. Although there is no need for a structural graft, cancellous bone harvest via a small incision still results in donor site morbidity. Different kinds of biomaterials including calcium phosphate ceramic [8, 9] and demineralized bone matrix [10] were developed to fill the cage instead of autograft in order to avoid the donor site complication.
In this study, the CS/DBM was used to fill in the PEEK cage instead of autogenous bone. DBM is a derivative of allograft bone and possesses putative biological or osteoinductive activity. It contains type-1 collagen, noncollagenous proteins, and a small amount of osteoinductive growth factors such as BMPs, transforming growth factor beta 1 (TGF-β1), and insulin-like growth factor (IGF) [29]. It is prepared by pulverisation of allogenic bone to a consistent size, followed by mild acid extraction of the mineralised phase of bone [30, 31]. As a dry powder, DBM is often mixed with other carriers to turn it into a putty or paste. The preparation of DBM and the type of component with which it is combined have the influence on its osteoconductivity [32, 33]. Calcium sulphate is one of these carriers. The use of CS as a regenerative material was firstly reported in 1892 [34]. It has resorbable osteoconductive properties due to the three-dimensional structural framework which is useful for angiogenesis and osteogenesis [35]. Thus the CS/DBM composite graft possesses both osteoconductive and osteoinductive properties and has been used to treat bone defects. Kim et al. [36] compared CS/DBM composite graft with CS or DBM alone in a controlled, split-mouth study using a dog model. They found that surgical implantation of DBM and CS, alone or in combination, may result in significantly improved regeneration of alveolar bone in three-wall intrabony periodontal defects. Kim et al. [37] also investigated a composite graft composed of CS and DBM in a randomized, controlled clinical study. They found that a CS/ DBM composite graft covered by a CS barrier in intrabony periodontal defects had the same significant improvements as the control group, which received gingival flap surgery alone. Feng et al. [14] found that CS/ DBM could be used as a safe and effective graft extender in free vascularised fibular grafting for large osteonecrotic lesions of the femoral head. Although the CS/DBM composite graft has been successfully used in the bone defect to promote healing, there is a lack of literature regarding the use of CS/DBM in the cervical interbody fusion. This study addressed this point and showed that the CS/DBM could be packed in the PEEK cage to promote interbody fusion in the cervical spine.
The CS/DBM composite graft is radiopaque and the complete filling in the PEEK cage can be monitored in the radiographic film. The CS provides a biological osteoconductive framework which new bone can grow into and is resorbed at a rate consistent with natural bone formation. Over a period of six to12 weeks the calcium sulphate is reabsorbed by a process of dissolution in ovine tibial and femoral metaphyseal defects [38]. Lillo and Peltier [39] have reported that calcium sulphate without being covered with periosteum is not absorbed but, when covered, is completely absorbed within 45 to 72 days, and that calcium sulphate facilitates new bone formation in contact with periosteum or bones. Its rapid reabsorption provides an osteoconductive scaffold for the ingrowth of blood vessels and associated fibrogenic and osteogenic cells. Therefore, in this study the CS/DBM was opaque in the transparent PEEK cage at the discharge. At six-week follow-up, the CS had gradually dissolved and the graft in the cage had become nearly transparent. At three-month follow-up, the graft in the cage was transparent in the X-film because of the complete absorption of CS without new mineralization bone formation. DBM has been shown to have an osteoconductive and osteoinductive potential [16–18]. It is encapsulated in the CS and does not provide structural strength. The proteins and various growth factors including BMPs in the extracellular matrix will be released continually to promote fusion when the CS scaffold dissolves gradually. Hence, six months after the implantation, new bone had formed in the cage, especially in the area close to the upper and lower endplate where the graft contacted the host bone directly. One year later, new bone had formed in the cage, which made the centre part of the cage opaque again.
The incidence of adverse reaction was reported to be 13.8 % and symptoms developed an average of 38.9 days after the operation when the CS was used as a bone defect filler [40]. The most common sign of adverse reaction was edematous or erythematous appearance in the post-operative incision site without other signs of infection. Active drainage or expression of serous fluid was also considered an adverse reaction. Wound drainage has been reported in 4 % of 109 patients treated with calcium sulphate pellets in a prospective multicentre study [41]. Although there were complications in this study, none was related to this adverse reaction. It has been theorized that this serous drainage is the result of the osmotic effect of the calcium sulphate and that it subsides with calcium sulphate resorption.
The clinical benefits of CS/DBM instead of autogenous bone in the PEEK cage are evident in this study because of the similar fusion rates and clinical outcomes in two cervical interbody groups. The surgical time and blood loss were shortened in the CS/DBM group and the additional surgical site and its complications were avoided. However, there are some limitations in this study. First, the sample size for patients included in this study is relatively small. Further clinical studies with more patients will be necessary. Second, assessment of interbody fusion was determined by plain radiography particularly and fine CT scan. The new bone incorporation process was estimated by the density change on the plain radiography. The real process of CS/DBM degradation and new bone ingrowth could not be elucidated because it was impossible to perform biopsy in the clinical practice. An animal study should be carried out to give a more vivid description on this process in the future.
Conclusions
In summary, the PEEK interbody fusion cage containing CS/DBM following one- or two-level discectomy proved to have a similar outcome as the PEEK cage containing AIG for cervical spondylotic radiculopathy and/or myelopathy. The rate of fusion and the recovery rate of JOA score between the two groups were the same. The PEEK cage containing CS/DBM provides an effective and reliable alternative to PEEK cage containing AIG. The CS/DBM method has less operative blood loss and fewer complications at the donor site.
References
Cloward RB (1958) The anterior approach for removal of ruptured cervical disks. J Neurosurg 15:602–617
Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40-A:607–624
Banwart JC, Asher MA, Hassanein RS (1995) Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine (Phila Pa 1976) 20:1055–1060
Vaccaro AR, Singh K, Haid R, Kitchel S, Wuisman P, Taylor W, Branch C, Garfin S (2003) The use of bioabsorbable implants in the spine. Spine J 3:227–237
Vavruch L, Hedlund R, Javid D, Leszniewski W, Shalabi A (2002) A prospective randomized comparison between the Cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiologic study. Spine (Phila Pa 1976) 27:1694–1701
Song KJ, Lee KB (2006) A preliminary study of the use of cage and plating for single-segment fusion in degenerative cervical spine disease. J Clin Neurosci 13:181–187
Liao JC, Niu CC, Chen WJ, Chen LH (2008) Polyetheretherketone (PEEK) cage filled with cancellous allograft in anterior cervical discectomy and fusion. Int Orthop 32:643–648
Dai LY, Jiang LS (2008) Anterior cervical fusion with interbody cage containing beta-tricalcium phosphate augmented with plate fixation: a prospective randomized study with 2-year follow-up. Eur Spine J 17:698–705
Cho DY, Lee WY, Sheu PC, Chen CC (2005) Cage containing a biphasic calcium phosphate ceramic (Triosite) for the treatment of cervical spondylosis. Surg Neurol 63:497–503, discussion 503–494
Topuz K, Colak A, Kaya S, Simsek H, Kutlay M, Demircan MN, Velioglu M (2009) Two-level contiguous cervical disc disease treated with peek cages packed with demineralized bone matrix: results of 3-year follow-up. Eur Spine J 18:238–243
Scholz M, Schleicher P, Eindorf T, Friedersdorff F, Gelinsky M, Konig U, Sewing A, Haas NP, Kandziora F (2010) Cages augmented with mineralized collagen and platelet-rich plasma as an osteoconductive/inductive combination for interbody fusion. Spine (Phila Pa 1976) 35:740–746
Dickerman RD, Reynolds AS, Morgan B (2008) Polyetheretherketone (PEEK) cage filled with bone morphogenic protein and demineralised bone matrix in anterior cervical discectomy and fusion. Int Orthop 32:717
Alderman NE (1969) Sterile plaster of Paris as an implant in the infrabony environment: a preliminary study. J Periodontol 40:11–13
Feng Y, Wang S, Jin D, Sheng J, Chen S, Cheng X, Zhang C (2011) Free vascularised fibular grafting with OsteoSet(R)2 demineralised bone matrix versus autograft for large osteonecrotic lesions of the femoral head. Int Orthop 35:475–481
Niu CC, Tsai TT, Fu TS, Lai PL, Chen LH, Chen WJ (2009) A comparison of posterolateral lumbar fusion comparing autograft, autogenous laminectomy bone with bone marrow aspirate, and calcium sulfate with bone marrow aspirate: a prospective randomized study. Spine (Phila Pa 1976) 34:2715–2719
Katz JM, Nataraj C, Jaw R, Deigl E, Bursac P (2009) Demineralized bone matrix as an osteoinductive biomaterial and in vitro predictors of its biological potential. J Biomed Mater Res B Appl Biomater 89:127–134
McKee MD (2006) Management of segmental bony defects: the role of osteoconductive orthobiologics. J Am Acad Orthop Surg 14:S163–S167
Peterson B, Whang PG, Iglesias R, Wang JC, Lieberman JR (2004) Osteoinductivity of commercially available demineralized bone matrix. Preparations in a spine fusion model. J Bone Joint Surg Am 86-A:2243–2250
Pietrzak WS, Perns SV, Keyes J, Woodell-May J, McDonald NM (2005) Demineralized bone matrix graft: a scientific and clinical case study assessment. J Foot Ankle Surg 44:345–353
Wang JC, Alanay A, Mark D, Kanim LE, Campbell PA, Dawson EG, Lieberman JR (2007) A comparison of commercially available demineralized bone matrix for spinal fusion. Eur Spine J 16:1233–1240
Sampath P, Bendebba M, Davis JD, Ducker TB (2000) Outcome of patients treated for cervical myelopathy. A prospective, multicenter study with independent clinical review. Spine (Phila Pa 1976) 25:670–676
Anderson PA, Subach BR, Riew KD (2009) Predictors of outcome after anterior cervical discectomy and fusion: a multivariate analysis. Spine (Phila Pa 1976) 34:161–166
Grossman W, Peppelman WC, Baum JA, Kraus DR (1992) The use of freeze-dried fibular allograft in anterior cervical fusion. Spine (Phila Pa 1976) 17:565–569
Young WF, Rosenwasser RH (1993) An early comparative analysis of the use of fibular allograft versus autologous iliac crest graft for interbody fusion after anterior cervical discectomy. Spine (Phila Pa 1976) 18:1123–1124
Boakye M, Mummaneni PV, Garrett M, Rodts G, Haid R (2005) Anterior cervical discectomy and fusion involving a polyetheretherketone spacer and bone morphogenetic protein. J Neurosurg Spine 2:521–525
Moore R, Beredjiklian P, Rhoad R, Theiss S, Cuckler J, Ducheyne P, Baker DG (1997) A comparison of the inflammatory potential of particulates derived from two composite materials. J Biomed Mater Res 34:137–147
Pechlivanis I, Thuring T, Brenke C, Seiz M, Thome C, Barth M, Harders A, Schmieder K (2011) Non-fusion rates in anterior cervical discectomy and implantation of empty polyetheretherketone cages. Spine (Phila Pa 1976) 36:15–20
Cho DY, Liau WR, Lee WY, Liu JT, Chiu CL, Sheu PC (2002) Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery 51:1343–1349, discussion 1349–1350
Einhorn TA, Lane JM, Burstein AH, Kopman CR, Vigorita VJ (1984) The healing of segmental bone defects induced by demineralized bone matrix. A radiographic and biomechanical study. J Bone Joint Surg Am 66:274–279
Lee KJ, Roper JG, Wang JC (2005) Demineralized bone matrix and spinal arthrodesis. Spine J 5:217S–223S
Miyazaki M, Tsumura H, Wang JC, Alanay A (2009) An update on bone substitutes for spinal fusion. Eur Spine J 18:783–799
Cheung S, Westerheide K, Ziran B (2003) Efficacy of contained metaphyseal and periarticular defects treated with two different demineralized bone matrix allografts. Int Orthop 27:56–59
Russell JL, Block JE (1999) Clinical utility of demineralized bone matrix for osseous defects, arthrodesis, and reconstruction: impact of processing techniques and study methodology. Orthopedics 22:524–531, quiz 532–523
Peltier LF (1959) The use of plaster of Paris to fill large defects in bone. Am J Surg 97:311–315
Tay BK, Patel VV, Bradford DS (1999) Calcium sulfate- and calcium phosphate-based bone substitutes. Mimicry of the mineral phase of bone. Orthop Clin N Am 30:615–623
Kim CK, Kim HY, Chai JK, Cho KS, Moon IS, Choi SH, Sottosanti JS, Wikesjo UM (1998) Effect of a calcium sulfate implant with calcium sulfate barrier on periodontal healing in 3-wall intrabony defects in dogs. J Periodontol 69:982–988
Kim CK, Chai JK, Cho KS, Moon IS, Choi SH, Sottosanti JS, Wikesjo UM (1998) Periodontal repair in intrabony defects treated with a calcium sulfate implant and calcium sulfate barrier. J Periodontol 69:1317–1324
Peters CL, Hines JL, Bachus KN, Craig MA, Bloebaum RD (2006) Biological effects of calcium sulfate as a bone graft substitute in ovine metaphyseal defects. J Biomed Mater Res A 76:456–462
Lillo R, Peltier LF (1956) The substitution of plaster of Paris rods for portions of the diaphysis of the radius in dogs. Surg Forum 6:556–558
Lee GH, Khoury JG, Bell JE, Buckwalter JA (2002) Adverse reactions to OsteoSet bone graft substitute, the incidence in a consecutive series. Iowa Orthop J 22:35–38
Kelly CM, Wilkins RM, Gitelis S, Hartjen C, Watson JT, Kim PT (2001) The use of a surgical grade calcium sulfate as a bone graft substitute: results of a multicenter trial. Clin Orthop Relat Res 382:42–50
Acknowledgments
This work was supported by the National Natural Science Foundation of China (81071453), the project administrated by Shanghai Science and Technology Committee (13DZ1940802 & 14441901700), the Program for Innovative Research Team of Shanghai Municipal Education Commission, and the Fund for Interdisciplinary Research on Medicine and Engineering of Shanghai Jiaotong University (YG2011MS24). No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Youzhuan XIE and Hua LIcontributed equally to this work.
Rights and permissions
About this article
Cite this article
Xie, Y., Li, H., Yuan, J. et al. A prospective randomized comparison of PEEK cage containing calcium sulphate or demineralized bone matrix with autograft in anterior cervical interbody fusion. International Orthopaedics (SICOT) 39, 1129–1136 (2015). https://doi.org/10.1007/s00264-014-2610-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2610-9