Abstract
Interleukin-15 (IL-15) is a proinflammatory cytokine involved in the proliferation, survival, and activation of multiple lymphocyte lineages. However, the prognostic significance of IL-15 for extranodal NK/T cell lymphoma (ENKTL) has not been well established. We retrospectively analyzed 112 patients with newly diagnosed ENKTL. Baseline serum IL-15 levels were determined using sandwich enzyme-linked immunosorbent assays. Patients with high IL-15 (>3.94 mg/L) at diagnosis tended to have more adverse clinical features. Patients with low IL-15 (≤3.94 mg/L) at diagnosis had better progression-free survival (PFS; P < 0.001) and overall survival (OS; P < 0.001) and achieved higher complete remission rates (P = 0.001). Multivariate analysis revealed independent prognostic factors for PFS. Similarly, high IL-15 levels (P = 0.009), no CR after chemotherapy (P = 0.001), Stage III/IV (P = 0.048), and elevated serum EBV-DNA (P = 0.038) were independently predictive of shorter OS. Using the International Prognostic Index or Korean Prognostic Index for nasal NK/T cell lymphoma, the majority of patients were in the low-risk category (with no or one adverse factor). Serum IL-15 was helpful to differentiate the low-risk patients with different survival outcomes (P < 0.001).Our data suggest that serum IL-15 at diagnosis is a novel, powerful predictor of prognosis for ENKTL, which suggests a role for IL-15 in the pathogenesis of this disease and offers new insight into potential therapeutic strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extranodal NK/T cell lymphoma (ENKTL) is relatively more common in Asia than in Western countries [1, 2]. Based on a recent large survey [3], it is the second most prevalent lymphoma subtype and accounts for 5–10 % of all types of lymphomas in China. ENKTL is characterized by angiodestruction, obvious necrosis, and association with Epstein–Barr virus (EBV). Multiple studies have demonstrated that elevated cytokines levels are associated with these pathological changes, for instance, CXCL9, CXCL10 [4, 5], and interleukin-9 (IL-9) [6].
Interleukin-15 (IL-15) is a proinflammatory cytokine referred to the proliferation, survival, and activation of multiple lymphocyte lineages via various kinds of signaling pathways [7, 8]. Recently, many studies have demonstrated that IL-15 can endow neoplastic cells with a selective growth advantage initiating and promoting certain types of malignancies [9, 10]. As regards the clinical significance of IL-15 in hematopoietic malignancies, several studies have suggested that IL-15 may enhance cellular proliferation and was associated with poor prognosis, in particular, relapse-free survival in adult acute lymphoblastic leukemia [11, 12]. Baldassarre et al. [13] also reported that chronic stimulation with IL-15 gives rise to the development of NK lymphoma in a mouse model. In a study with small sample sizes, the serum levels of IL-15 were increased significantly in ENKTL patients than in healthy individuals [14]. The same team of researchers found that the supplementation with exogenous interleukin-15 can promote proliferation and inhibit apoptosis of NK-92, an NK-cell lines (CD3−CD56+TCR−), in vitro [14]. These results indicate that IL-15 can play an important role in the pathogenesis of ENKTL. We hypothesize that IL-15 levels are associated with poor prognosis for ENKTL.
In ENKTL, the prognostic value of Korean Prognostic Index (KPI) was verified by clinical studies. More than 50 % of the patients with ENKTL are in the low KPI risk group, but some of these patients still have a poor clinical outcome [15]. Therefore, the identification of specific risk factors remains an important issue. In this study, we characterized the serum levels of IL-15 and evaluated its impact on the outcome in ENKTL.
Materials and methods
Ethics statement
This study was approved by the Institutional Review Board and ethics committees of Sun Yat-Sen University Cancer Center. Written informed consent for blood samples and medical information were obtained from all patients and healthy volunteers. The study was performed in agreement with the guidelines of the Declaration of Helsinki.
Eligibility criteria
We conducted a retrospective study of 112 patients newly diagnosed with nasal ENKTL, who received chemotherapy, radiotherapy or both at the Sun Yat-sen University Cancer Center from January 2003 to 2014. The inclusion criteria in this study were as follows: (1) pathologically confirmed diagnosis of NK/T cell lymphoma according to the WHO classification, (2) NK/T cell are positive in the detection of CD3, CD56, and cytotoxic molecules by immunohistochemical, Epstein–Barr virus (EBV) by in situ hybridization, (3) no previous or concomitant malignant tumor and no previous anti-cancer treatments, (4) available serum samples obtained prior to the initial treatment and stored at −80 °C, and (5) adequate clinical information and follow-up data. Patients were excluded if found any clinical evidence to support chronic active inflammatory, such as rheumatoid arthritis and pancreatitis. Patients with other subtypes of NHL, including unspecified peripheral T cell lymphoma or blastic NK-cell lymphoma/leukemia, were not included.
All patients were staged by using the standard Ann Arbor staging system. The International Prognostic Index (IPI; age, PS, stage, LDH level, extranodal sites) and NK/T cell lymphoma Prognostic Index (KPI; stage, LDH level, B symptoms, regional lymph nodes) [2] were calculated on the basis of patient demographics, physical examination, Eastern Cooperative Oncology Group performance status (ECOG PS), B symptoms, the value of lactate dehydrogenase (LDH) from serum biochemistry, magnetic resonance imaging (MRI) of the head and neck and computed tomography (CT) scan of the chest, abdomen and pelvis, positron emission tomography–computed tomography (PET-CT) of the whole body, bone marrow aspiration, and trephine biopsy. Complete blood counts and serum Epstein–Barr virus-DNA (EBV-DNA) copy number were routinely examined.
Treatment
Patients received treatment strategies as follows: (1) patients with early-stage ENKTL received chemotherapy followed by involved-field radiotherapy (IFRT) and (2) patients with advanced stage ENKTL received chemotherapy alone. The chemotherapy regimens were as follows: (1) EPOCH (etoposide, doxorubicin, vincristine, cyclophosphamide, prednisone); (2) GELOX (gemcitabine, oxaliplatin, l-asparaginase) [16]; and (3) CHOP-L (CHOP plus l-asparaginase). Patients were given at least two cycles. A maximum of six initial chemotherapy cycles were utilized. Involved-field radiotherapy median total dose was 56 Gy with a range of 45–60 Gy, which was given as daily 2 Gy with 5 fractions each week. The treatment response was assessed in accordance with standard response criteria for non-Hodgkin lymphoma [17]. After the whole treatment was completed, patients were followed-up and evaluated by their oncologist in the outpatient department.
ELISA
Sandwich enzyme-linked immunosorbent assay (ELISA) kits (R&D Systems, CA, USA) were used to measure serum IL-15 levels. All venous blood samples were obtained from patients at diagnosis and twelve healthy subjects. The blood samples were centrifuged, and serum was collected and stored at −80 °C until further assay. Serum samples were routinely analyzed by ELISA according to the manufacturer’s protocol. Briefly, standards and samples were added to a microplate, which have been precoated with a mouse monoclonal antibody specific to IL-15. After removal of any unbound antibody or enzyme reagent by washing, a substrate solution was added to the wells; color development was terminated by Stop Solution; and the resulting absorbance was read at 450 nm using a spectrophotometer (Tecan, Mannedorf, Switzerland). IL-15 concentrations were interpolated from a standard curve, which was generated using the recombinant IL-15 protein. All samples were analyzed in triplicate, and the results were averaged.
Statistical analysis
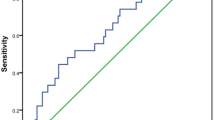
Serum IL-15 concentration was presented as median (min, max), while categorical data are expressed as n (%). Differences between the two groups were tested using Mann–Whitney U test or Chi-square test. The receiver operating characteristics (ROC) curve analysis was used to determine the cutoff concentration for serum IL-15 in the prediction of survival. The Kaplan–Meier method and log-rank test were applied for univariate analyses of the impacts of several pretreatment characteristics on survival, including IL-15. Variables which were significant at P < 0.05 in univariate analysis were entered into multivariate analysis. Multivariate analysis was used to assess the prognostic impact of selected variables, according to the Cox regression model.
Results
Patient characteristics
In total, 112 patients (73 male, 39 female; median age 44 years) met the inclusion criteria. The clinical characteristics of the 112 patients are listed in Table 1. Most patients (101 cases, 90.2 %) displayed a favorable performance status (ECOG PS 0–1). Forty-six patients (41.1 %) presented with B symptoms. Elevated LDH levels were observed for 34 cases (30.4 %). Fifty-eight patients (51.8 %) displayed regional lymph node involvement. Most patients (88 cases, 78.6 %) had localized disease (Stage I/II). According to the IPI, a majority of the patients (87 cases, 77.7 %) were classified as low/low–intermediate risk (IPI = 0–1), and 25 patients (22.3 %) were categorized as intermediate–high/high risk (IPI = 2–5). The number of patients with KPI = 0–1 (62 cases, 55.4 %) was significantly higher than those with KPI = 2–4 (50 cases, 44.6 %).
Baseline serum IL-15 levels
The mean concentration of serum IL-15 for all patients was 4.1 pg/mL with a median of 3.76 pg/mL (range 1.19–13.45 pg/mL). Serum IL-15 was detected in ten healthy volunteers, and the median concentration was 0.67 pg/mL (range 0–1.12 pg/mL), which was significantly lower than that of ENKTL patients (P < 0.001). To identify an optimal cutoff point for survival outcomes, the ROC curve analysis was selected. The most discriminative cutoff concentration of serum IL-15 was 3.94 pg/mL with an area under the curve (AUC) value of 0.776 [95 % confidence interval (CI) 0.679–0.872, P < 0.001] (Fig. 1). Based on the ROC analysis result, we used the IL-15 level >3.94 mg/L as the cutoff value in the present study. Based on this cutoff value, 67 patients (57.1 %) were categorized into the low-CRP group (≤3.94 mg/L), and 48 patients (42.9 %) were categorized into the high-CRP group (>3.94 mg/L). The baseline clinical features of the patients in the low-CRP group were compared with those in the high-CRP group (Table 1). The high-CRP group was characterized by a higher proportion of patients with more frequent B symptoms, elevated serum EBV-DNA levels, more common Regional LN involvement and elevated KPI scores. As shown in Table 1, the serum IL-15 level was significantly higher in patients with elevated LDH levels, poor PS, no complete response (CR) after chemotherapy, etc. However, there was no significant correlation between serum IL-15 level and gender, age, Ann Arbor stage.
Treatment modalities and response
The primary treatment modalities were as follows: (a) 88 cases (78.6 %) received chemotherapy followed by radiotherapy (RT); and (b) 24 cases (21.4 %) received chemotherapy alone; the treatment details and responses are listed in Table 2. No significant difference was found in the treatment modalities as well as chemotherapy regimens between the patients with IL-15 levels ≤3.94 mg/L and patients displaying IL-15 levels >3.94 mg/L (P = 0.248). After the initial treatment, 73 of the 112 treated patients (65.2 %) achieved a CR. The rate of CR to initial treatment was significantly higher in the low IL-15 group than in the high IL-15 group (78.1 vs. 47.9 %, respectively, P = 0.001).
Survival and prognostic factors
Within a median follow-up time of 31 months (5–152), the 5-year PFS and OS rates for all 112 patients were 51.7 (95 % CI 40.9–62.5 %) and 60.6 % (95 % CI 50.4–70.8 %), respectively. Patients in low IL-15 group had significantly better PFS (5-year PFS 77.5 vs. 14.1 %, P < 0.001; Fig. 2a) and OS (5-year OS 80.6 vs. 36.6 %, P < 0.001; Fig. 2b). In the patients received chemotherapy alone (n = 2,421.4 %), elevated serum IL-15 levels were associated with shorter PFS and OS (P = 0.035 and P = 0.028, respectively) and also related to inferior PFS and OS (P < 0.001 and P < 0.001, respectively) in the patients received chemotherapy followed by radiotherapy (n = 8,878.6 %). Significant survival differences were found between the patients who gained CR after chemotherapy and those without CR (P < 0.001 and P < 0.001, respectively, Fig. 3a, b).
Table 3 displays the results of the univariate and multivariate analysis of the potential predictors of PFS and OS. Multivariate analysis using the forward conditional Cox region model identified IL-15 levels >3.94 mg/L (RR = 4.138, 95 % CI 2.043–8.383, P < 0.001), B symptoms (RR = 1.965, 95 % CI 1.079–3.580, P = 0.027), and no CR after chemotherapy (RR = 3.101, 95 % CI 1.939–4.957, P < 0.001) as three adverse factors for PFS. In the multivariate analysis for OS, IL-15 levels >3.94 mg/L (RR = 2.943, 95 % CI 1.305–6.639, P = 0.009), stage III/IV (RR = 2.608, 95 % CI 1.009–6.742, P = 0.048), no CR after chemotherapy (RR = 2.515, 95 % CI 1.454–4.348, P = 0.001), and serum EBV-DNA (RR = 2.141, 95 % CI 1.043–4.395, P = 0.038) were found to be significant independent predictors of OS.
The distribution of patients inside risk groups based on IPI score and KPI score is presented in Table 4. In the IPI score, more than 70 % of all cases were in the low-risk category (with no or one adverse factor), but this prognostic model failed to differentiate patients with different outcomes in the low-risk group. The KPI model balanced distribution of patients into different risk groups better than IPI model (score 0–1: 62 cases, 55.4 %; score 2–4: 50 cases, 44.6 %). However, the KPI model also had no discriminating power in patients with no or one adverse factors (5-year OS 70.6 vs. 63.3 %, P = 0.425).
For patients in the low-risk category according to IPI, serum IL-15 level at diagnosis could distinguish those with good outcomes from those with poor outcomes. Serum IL-15 level can divide the patients in IPI score of 0–1 group (n = 87, 77.7 %) into two subgroups with significant differences in PFS and OS (P < 0.001 and P < 0.001, respectively, Fig. 4a, b). Similarly, in patients with KPI score of 0–1 (n = 62, 55.4 %), serum IL-15 level at diagnosis also helped to differentiate patients with different prognoses (P < 0.001 and P < 0.001, respectively, Fig. 4c, d).
Progression-free survival (PFS) and Overall survival (OS) according to serum IL-15 level (≤3.94 vs. >3.94 mg/L) at diagnosis in patients with extranodal natural killer T cell lymphoma, nasal type (ENKTL). Kaplan–Meier plots of PFS (a) and OS (b) for subgroups with low International Prognostic Index (IPI) score of 0–1; Kaplan–Meier plots of PFS (c) and OS (d) for subgroups with low Korean Prognostic Index (KPI) score of 0–1
Discussion
Previous studies have confirmed the role of IL-15 in various hematological malignancies, including adult T cell leukemia, acute lymphoblastic leukemia, and NK/T cell lymphoma [14, 18, 19]. A clinical study in adult ALL indicated that higher IL-15 expression was significant associated with shorter survival. However, the prognostic role of IL-15 in ENKTL remains unclear. In this study, we found that the serum concentration of IL-15 in ENKTL patients was much higher than in normal healthy people. In ENKTL patients, the levels of serum IL-15 significantly correlated with clinicopathological features, such as elevated LDH levels, poor PS, and no complete response (CR) after chemotherapy. Furthermore, elevated serum concentration of IL-15 was related to poor responses to chemotherapy or chemoradiotherapy. According to the Cox regression model that included the serum levels of IL-15, responses after chemotherapy, stage III/IV, serum EBV-DNA, B symptoms, and so on, it was concluded that serum IL-15 and responses after chemotherapy were independent prognostic factors for both PFS and OS.
In the present study, we measured serum IL-15 levels in healthy volunteers and patients with ENKTL. We found that IL-15 was fairly low in the healthy controls (median concentration 0.67 pg/mL), but it showed a relative higher level in patients with ENKTL, with a median value of 3.76 pg/mL. The results of the current study are consistent with the recent study of Chow et al. [14] in which serum IL-15 levels were first reported as a specific tumor biomarker for ENKTL patients. IL-15 is a pleiotropic cytokine that influences proliferation, differentiation, resistance to apoptosis [20], and cellular localization of T [21] and B lymphocytes [7], neutrophils [22], and natural killer (NK) cells [23]. Thus, it is easy to explain the correlation between IL-15 and B symptoms, elevated serum LDH and response to treatment. However, it remains unclear why IL-15 levels were also associated with EBV-DNA.
According to the ROC curve analyses, 3.94 pg/mL was an optimal cutoff value for distinguishing between poor outcomes and good outcomes. Patients with low IL-15 levels (≤3.49 pg/mL) tended to have higher CR rates (78.1 %) than those with high IL-15 levels (>3.49 pg/mL) (47.9 %) (P = 0.001). Specifically, 5-year PFS and OS rate in the low IL-15 level group were clearly longer than those in the high IL-15 level group (PFS 77.5 vs. 14.1 %, P < 0.001; OS 80.6 vs. 36.6 %, P < 0.001). Multivariate analysis also indicated that IL-15 was an independent prognostic factor for PFS and OS. All these data confirmed that serum IL-15 was closely correlated with treatment response and prognosis in ENKTL, implying a significant role for IL-15 in the pathogenesis and development of this disease. Nevertheless, IL-15 can lead to either a favorable or unfavorable clinical prognosis depending on the tumor. Yajima et al. [24] examined the effects of in vivo overexpression of IL-15 on protection against two types of murine B16 melanoma lines, B16.44, and B16F10 cells in IL-15 transgenic (Tg) mice and found that tumor growth was severely retarded in IL-15 Tg mice after subcutaneous (s.c.) inoculation with B16.44 or B16F10 cells. The inconsistent roles of IL-15 in tumors may be partly attributed to different immune effects or single nucleotide polymorphisms.
Although ENKTL is a distinctive entity with poor prognosis, approximately 70 % of the patients in our study were categorized as low risk based on IPI score. Accordingly, patients with adverse and good clinical outcomes were found in the group with IPI score <2. The prognostic value of IPI and KPI model was evaluated in the present study. These two models were highly prognostic in the univariate analysis. The KPI model balanced distribution of patients into different risk groups. However, patients were allocated disproportionately within the IPI prognostic model. Moreover, all these three models failed to identify patients with poor prognosis in the low-risk category (with no or one adverse factor). When adding serum IL-15 at diagnosis to the two models, the low-risk patients were separated on the basis of different survival outcomes with sufficient statistical power.
A possible role for IL-15 in malignant disorders of the immune system was first suggested by its identification in an adult T cell leukemia-lymphoma cell line and the fact that IL-15 transgenic mice develop an NK/T large granular lymphocyte leukemia—like disease [25]. The mechanisms underlying the relationship between elevated serum IL-15 levels and poor prognosis are not clear; however, several potential explanations have been proposed. Functionally, IL-15 supports cell expansion and maintenance by (1) inducing strong proliferative signals via JAK/STAT and Ras/MAPK signaling pathways and (2) preventing cell death by increasing antiapoptotic proteins Bcl-2 and Bcl-Xl, as well as decreasing proapoptotic proteins Bim and Puma through activation of the PI3 K pathway [26–31]. Indeed, Chow et al. [14] found that IL-15 can also maintain the survival of NK-92 cells by preserving AKT phosphorylation. Recent studies show that IL-15 enhances cellular proliferation and upregulates CNS homing molecules in pre-B acute lymphoblastic leukemia by inducing STAT5, ERK 1/2, and to a lesser extent PI3K and NF-kB phosphorylation [25]. Further studies, however, are needed to elucidate the cellular mechanisms of IL-15-mediated signaling in NK/T cell lymphoma.
In conclusion, this is the first study that confirms the close relationship of IL-15 with several clinical features of ENKTL, including B symptoms, Regional LN involvement, etc. Serum IL-15, which can be easily measured in clinical practice, may be a significant independent prognostic factor for this disease. These results suggest a role for IL-15 in the pathogenesis of ENKTL and offer new insight into potential therapeutic strategies. Future prospective studies are warranted to confirm our findings.
References
Au WY, Weisenburger DD, Intragumtornchai T, et al. Clinical differences between nasal and extranasal natural killer/T-cell lymphoma: a study of 136 cases from the international peripheral T-cell lymphoma project. Blood. 2009;113:3931–7.
Lee J, Suh C, Park YH, et al. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J Clin Oncol. 2006;24:612–8.
Sun J, Yang Q, Lu Z, et al. Distribution of lymphoid neoplasms in China: analysis of 4,638 cases according to the World Health Organization classification. Am J Clin Pathol. 2012;138:429–34.
Moriai S, Takahara M, Ogino T, et al. Production of interferon-{gamma}-inducible protein-10 and its role as an autocrine invasion factor in nasal natural killer/T-cell lymphoma cells. Clin Cancer Res. 2009;15:6771–9.
Teruya-Feldstein J, Jaffe ES, Burd PR, et al. The role of Mig, the monokine induced by interferon-gamma, and IP-10, the interferon-gamma-inducible protein-10, in tissue necrosis and vascular damage associated with Epstein–Barr virus-positive lymphoproliferative disease. Blood. 1997;90:4099–105.
Nagato T, Kobayashi H, Kishibe K, et al. Expression of interleukin-9 in nasal natural killer/T-cell lymphoma cell lines and patients. Clin Cancer Res. 2005;11:8250–7.
Armitage RJ, Macduff BM, Eisenman J, et al. IL-15 has stimulatory activity for the induction of B cell proliferation and differentiation. J Immunol. 1995;154:483–90.
Cooper MA, Bush JE, Fehniger TA, et al. In vivo evidence for a dependence on interleukin 15 for survival of natural killer cells. Blood. 2002;100:3633–8.
Giron-Michel J, Giuliani M, Fogli M, et al. Membrane-bound and soluble IL-15/IL-15 Ralpha complexes display differential signaling and functions on human hematopoietic progenitors. Blood. 2005;106:2302–10.
Tinhofer I, Marschitz I, Henn T, et al. Expression of functional interleukin-15 receptor and autocrine production of interleukin-15 as mechanisms of tumor propagation in multiple myeloma. Blood. 2000;95:610–8.
Cario G, Izraeli S, Teichert A, et al. High interleukin-15 expression characterizes childhood acute lymphoblastic leukemia with involvement of the CNS. J Clin Oncol. 2007;25:4813–20.
Wu S, Fischer L, Gokbuget N, et al. Expression of interleukin 15 in primary adult acute lymphoblastic leukemia. Cancer. 2010;116:387–92.
Baldassarre G, Fedele M, Battista S, et al. Onset of natural killer cell lymphomas in transgenic mice carrying a truncated HMGI-C gene by the chronic stimulation of the IL-2 and IL-15 pathway. Proc Natl Acad Sci USA. 2001;98:7970–5.
Chow C, Liu AY, Chan WS, et al. AKT plays a role in the survival of the tumor cells of extranodal NK/T-cell lymphoma, nasal type. Haematologica. 2005;90:274–5.
Huang JJ, Jiang WQ, Lin TY, et al. Absolute lymphocyte count is a novel prognostic indicator in extranodal natural killer/T-cell lymphoma, nasal type. Ann Oncol. 2011;22:149–55.
Wang H, Wuxiao ZJ, Zhu J, et al. Comparison of gemcitabine, oxaliplatin and l-asparaginase and etoposide, vincristine, doxorubicin, cyclophosphamide and prednisone as first-line chemotherapy in patients with stage IE to IIE extranodal natural killer/T-cell lymphoma: a multicenter retrospective study. Leuk Lymphoma. 2014. doi:10.3109/10428194.2014.939964.
Cheson BD, Horning SJ, Coiffier B, et al. Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J Clin Oncol. 1999;17:1244.
Burton JD, Bamford RN, Peters C, et al. A lymphokine, provisionally designated interleukin T and produced by a human adult T-cell leukemia line, stimulates T-cell proliferation and the induction of lymphokine-activated killer cells. Proc Natl Acad Sci USA. 1994;91:4935–9.
Barata JT, Keenan TD, Silva A, et al. Common gamma chain-signaling cytokines promote proliferation of T-cell acute lymphoblastic leukemia. Haematologica. 2004;89:1459–67.
Bulfone-Paus S, Ungureanu D, Pohl T, et al. Interleukin-15 protects from lethal apoptosis in vivo. Nat Med. 1997;3:1124–8.
Grabstein KH, Eisenman J, Shanebeck K, et al. Cloning of a T cell growth factor that interacts with the beta chain of the interleukin-2 receptor. Science. 1994;264:965–8.
Girard D, Paquet ME, Paquin R, Beaulieu AD. Differential effects of interleukin-15 (IL-15) and IL-2 on human neutrophils: modulation of phagocytosis, cytoskeleton rearrangement, gene expression, and apoptosis by IL-15. Blood. 1996;88:3176–84.
Carson WE, Fehniger TA, Haldar S, et al. A potential role for interleukin-15 in the regulation of human natural killer cell survival. J Clin Invest. 1997;99:937–43.
Yajima T, Nishimura H, Wajjwalku W, et al. Overexpression of interleukin-15 in vivo enhances antitumor activity against MHC class I-negative and -positive malignant melanoma through augmented NK activity and cytotoxic T-cell response. Int J Cancer. 2002;99:573–8.
Williams MT, Yousafzai Y, Cox C, et al. Interleukin-15 enhances cellular proliferation and upregulates CNS homing molecules in pre-B acute lymphoblastic leukemia. Blood. 2014;123:3116–27.
Huntington ND, Puthalakath H, Gunn P, et al. Interleukin 15-mediated survival of natural killer cells is determined by interactions among Bim, Noxa and Mcl-1. Nat Immunol. 2007;8:856–63.
Johnston JA, Bacon CM, Finbloom DS, et al. Tyrosine phosphorylation and activation of STAT5, STAT3, and Janus kinases by interleukins 2 and 15. Proc Natl Acad Sci USA. 1995;92:8705–9.
Miyazaki T, Kawahara A, Fujii H, et al. Functional activation of Jak1 and Jak3 by selective association with IL-2 receptor subunits. Science. 1994;266:1045–7.
Adunyah SE, Wheeler BJ, Cooper RS. Evidence for the involvement of LCK and MAP kinase (ERK-1) in the signal transduction mechanism of interleukin-15. Biochem Biophys Res Commun. 1997;232:754–8.
Steelman LS, Pohnert SC, Shelton JG, et al. JAK/STAT, Raf/MEK/ERK, PI3 K/Akt and BCR-ABL in cell cycle progression and leukemogenesis. Leukemia. 2004;18:189–218.
Miyazaki T, Liu ZJ, Kawahara A, et al. Three distinct IL-2 signaling pathways mediated by bcl-2, c-myc, and lck cooperate in hematopoietic cell proliferation. Cell. 1995;81:223–31.
Acknowledgments
We thank the patients and their families and all the investigators, including the physicians, nurses, and laboratory technicians in this study. Our work was supported by the following funds: National Natural Science Foundation of China, and the contract/Grant No. 81272620.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Article note
Hua Wang, Jia-yu Zhu, and Cheng-cheng Liu have contributed equally to this article.
Rights and permissions
About this article
Cite this article
Wang, H., Zhu, Jy., Liu, Cc. et al. Increased serum levels of interleukin-15 correlate with negative prognostic factors in extranodal NK/T cell lymphoma. Med Oncol 32, 370 (2015). https://doi.org/10.1007/s12032-014-0370-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0370-4