Abstract
Although anti-disialoganglioside (GD2) antibodies are successfully used for neuroblastoma therapy, a third of patients with neuroblastoma experience treatment failure or serious toxicity. Various strategies have been employed in the clinic to improve antibody-dependent cell-mediated cytotoxicity (ADCC), such as the addition of interleukin (IL)-2 to enhance natural killer (NK) cell function, adoptive transfer of allogeneic NK cells to exploit immune surveillance, and retinoid-induced differentiation therapy. Nevertheless, these mechanisms are not fully understood. We developed a quantitative assay to test ADCC induced by the anti-GD2 antibody Hu14.18K322A in nine neuroblastoma cell lines and dissociated cells from orthotopic patient-derived xenografts (O-PDXs) in culture. IL-2 improved ADCC against neuroblastoma cells, and differentiation with all-trans retinoic acid stabilized GD2 expression on tumor cells and enhanced ADCC as well. Degranulation was highest in licensed NK cells that expressed CD158b (P < 0.001) and harbored a killer-cell immunoglobulin-like receptor (KIR) mismatch against the tumor-specific human leukocyte antigen (HLA; P = 0.016). In conclusion, IL-2 is an important component of immunotherapy because it can improve the cytolytic function of NK cells against neuroblastoma cells and could lower the antibody dose required for efficacy, thereby reducing toxicity. The effect of IL-2 may vary among individuals and a biomarker would be useful to predict ADCC following IL-2 activation. Sub-populations of NK cells may have different levels of activity dependent on their licensing status, KIR expression, and HLA–KIR interaction. Better understanding of HLA–KIR interactions and the molecular changes following retinoid-induced differentiation is necessary to delineate their role in ADCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Decades of research have improved our understanding of the interactions between the immune system and tumors. Consequently, numerous therapeutic advances for adult cancers have made their way into the clinic in the past 30 years, including interventions to modulate immune system-mediated ablation of tumor cells with antibodies that target tumor-specific antigens for antibody-dependent cell-mediated cytotoxicity (ADCC) and complement-dependent cytotoxicity [1]. Other strategies are geared towards chimeric antigen receptor T cells [2] and immune check-point inhibitors [3] to exploit T cell-mediated tumor cell ablation. In addition, antibodies that abrogate cell receptor signaling (e.g., human epidermal growth factor receptor 2 [4]) or interfere with the tumor microenvironment (e.g., neutralizing antibodies against vascular endothelial growth factor [5]) are routinely used to provide therapeutic benefit.
Although several successful immunotherapy trials have been conducted for pediatric leukemias and lymphomas, far fewer have been conducted for pediatric solid tumors. To date, the most significant immunotherapy study for pediatric solid tumors investigated the efficacy of anti-disialoganglioside (GD2) antibody for neuroblastoma [6]. GD2 is a suitable target for antibody therapy because it is abundantly expressed in most neuroblastoma cells and its expression is restricted in normal cells, including peripheral nerves [7]. Anti-GD2 antibodies induce ADCC via natural killer (NK) cells [8]. NK cell surveillance mechanisms [9, 10] and NK cell stimulation with interleukin (IL)-2 [11] can also contribute to the antitumor effect. This has led to clinical trials incorporating IL-2, anti-GD2 antibodies, and adoptive transfer of haploidentical NK cells for the treatment of neuroblastoma (NCT01576692, NCT02650648, NCT00877110, and NCT01857934). Retinoid-based differentiation therapy has been used for children with neuroblastoma [6, 12]. Because GD2 is a marker of mature neurons, anti-GD2 antibody is currently administered in combination with cis-retinoic acid.
Despite many advances in neuroblastoma immunotherapy, the cellular mechanisms of intervention-augmented ADCC in neuroblastoma are not fully understood, although they may directly affect treatment. For example, insight into the relative contribution of ADCC versus NK cell surveillance could determine whether and when adoptive transfer of NK cells is useful during treatment. This may help define criteria for donor selection. In addition, better understanding of the differential and combined effects of IL-2, retinoic acid, and anti-GD2 antibody therapy may be useful to refine current treatment regimens, thereby reducing therapy-related toxicity.
Because a relatively small number of patients with high-risk neuroblastoma are diagnosed each year and available for clinical trials, it may take many years to improve our understanding in clinical studies of ADCC mechanisms in neuroblastoma. To expedite this process, we developed a quantitative ex vivo assay to test ADCC in several neuroblastoma cell lines and orthotopic patient-derived xenografts (O-PDXs). We quantified the relative contribution of ADCC or direct NK cell-mediated cytotoxicity to neuroblastoma cell death. These studies were performed with proliferating neuroblastoma cells and differentiated neuroblastoma cells that were treated with all-trans retinoic acid (ATRA), which is used with anti-GD2 antibody therapy in the clinic [6]. These studies are the first to use O-PDXs and patient-matched NK cells. Together, our data suggest that IL-2 is an important component of anti-GD2 antibody therapy in neuroblastoma. Moreover, we found that ADCC contributes more to NK cell degranulation ex vivo than does NK cell surveillance. By using our ADCC assay with patient-match O-PDXs and NK cells, we demonstrate the feasibility of studying immunotherapy strategies for individual patients with neuroblastoma.
Materials and methods
Tumor cells
Neuroblastoma cell lines were maintained in Roswell Park Memorial Institute 1640 medium (Lonza, Walkersville, MD; CHLA90, NBLS, SK-N-BE2, SK-N-JCI, SK-N-MM), Dulbecco’s modified eagle medium (Lonza; NB-1691, SK-N-NAS, SK-N-NFI), Eagle’s minimum essential medium (EMEM; American Type Culture Collection [ATCC], Manassas, VA; IMR32, SK-N-SH), and EMEM/Kaighn’s modification of Ham’s F12 media (ATCC; SH-SY5Y) supplemented with 10% heat-inactivated fetal bovine serum (Biowest, Kansas City, MO), 100 IU/mL penicillin, 100 µg/mL streptomycin, and 2 mM L-glutamine if base medium did not contain l-glutamine (all Gibco media, Grand Island, NY). The O-PDX lines SJNBL108_X and SJNBL013761_X1 were grown orthotopically in CD-1 immunodeficient mice and approved by the IACUC of St. Jude Children’s Research Hospital. Palpable tumors were harvested and further processed into single-cell suspensions for plating, as previously described [13].
NK cell preparation and isolation
For each experiment, NK cells from residual peripheral whole blood were collected from heparinized apheresis rings obtained from healthy de-identified blood donors. Each experiment was performed with a new donor. Peripheral blood mononuclear cells were isolated via density-gradient centrifugation (GE Healthcare Ficoll-Paque PLUS, Marlborough, MA), and red blood cells were removed with lysis buffer (Qiagen, Hamburg, Germany). NK cells were isolated with RosetteSep Human NK Cell Enrichment Cocktail (Stem Cell Technologies, Cambridge, MA) and human MACSxpress NK Cell Isolation Kit (Miltenyi Biotec, Bergisch Gladbach, Germany). IL-2 was provided by the Biological Resource Branch at the National Cancer Institute for preactivation of NK cells.
Therapeutic antibodies
The anti-GD2 antibody Hu14.18K322A was provided to St. Jude Children’s Research Hospital and Children’s GMP, LLC (Memphis, TN) by Merck Serono (Darmstadt, Germany) and was manufactured by Children’s GMP, LLC. The anti-HLA antibody W6/32 (Biolegend, San Diego, CA) recognizes a monomorphic epitope on the 45 kDa polypeptide products of HLA-A, -B, and -C and was used at a concentration of 1.5 µg/mL to block HLA.
ADCC and NK cytotoxicity assays and confluence analysis
For the ADCC and NK cytotoxicity assays, neuroblastoma cells were cultured on 96-well flat-bottom plates (Corning Inc., Corning, NY) at 37° in 5% CO2 incubators. The effector cell-to-target cell (E:T) ratio was determined by performing a semiautomated nuclear cell count after 4′,6-diamidino-2-phenylindole stain with Fiji (Curtis Rueden and Image J, Madison, WI) and manual count of neuroblastoma cells. To induce ADCC, different dilutions of Hu14.18K322A ranging from 10 pg/mL to 10 µg/mL were added to the culture wells 1 h prior to co-incubating effector cells with tumor cells. NK cytotoxicity assays were performed with effector cells to target tumor cells using the conditions and quantification described above for the ADCC assay; however, no hu14.18K322A was added. Calcein-AM (Thermo Fisher, Waltham, MA) was used at a concentration of 2 nM to perform live-cell staining. Images of calcein-AM-stained cells were acquired with a C2 Nikon confocal microscope (Nikon, Melville, NY). Images were further processed with the Fiji plugin Trainable Weka Segmentation that combines machine-learning algorithms with selected image features to conduct pixel-based segmentations. Segmented areas were quantified and represented confluence. Specific lysis was calculated with the following formula: \({\text{specific lysis }}(\% ){\text{ }}=\left( {1 - \left. {\frac{{{\text{confluence}}\;{\text{untreated}} - {\text{confluence}}\;{\text{treated}}}}{{{\text{confluence}}\;{\text{untreated}}}}~} \right)~} \right. \times 100.\) For ADCC assays with O-PDXs, the CellTiter-Glo luminescent cell viability assay (Promega, Madison, WI) was used to quantify specific lysis.
CD107a degranulation assay
NK cells were incubated with neuroblastoma cells at an E:T ratio of 5–1, in addition to anti-CD107a antibody (clone H4A3, Biolegend). After 1 h, GolgiStop solution (BD Biosciences, San Jose, CA) was added, and cells were incubated for another 3 h before staining for flow cytometry analysis.
Differentiation assay
To induce neuronal differentiation, neuroblastoma cells were incubated with 10 µM ATRA (Sigma Aldrich, St. Louis, MO) for 72 h.
RNA sequencing
Trizol (Invitrogen, Carlsbad, CA) RNA extraction was used to isolate total RNA, which was prepared by TruSeq and sequenced with an Illumina HiSeq 2500 (San Diego, CA). Resultant stranded paired-end 100-bp sequences were mapped to the hg19 reference genome with the STRONGARM pipeline [14] and counted with HTSeq (Simon Anders and EMBL Heidelberg, Germany) [15]. Fragments per kilobase of transcript per million mapped reads were calculated and then log2-transformed after the addition of a small variance stabilizing bias of 2 and logFC calculated for the ATRA treatment within each cell line. Differential gene expression was defined as fold change of > 2 or < 0.5.
HLA genotyping
Neuroblastoma cell lines were HLA-genotyped. We defined CD158a (2DL1) to be specific for HLA-C allotypes with lysine at position 80 (HLA-CLys80), CD158b1/b2 (2DL2/2DL3) to be specific for B*4601 and HLA-C allotypes with asparagine at position 80 (HLA-CAsn80), and CD158e1 (3DL1) to be specific for HLA-B allotypes expressing the Bw4 epitope (HLA-Bw4) [16].
Flow cytometry
Expression of killer-cell immunoglobulin-like receptors (KIRs) was determined by flow cytometry. The following antibodies were used: CD158a (clone 143211; R&D systems, Minneapolis, MN), CD158b1/2 (DX27; Biolegend), CD158e1 (DX9; Biolegend), and CD159a (REA110; Miltenyi Biotec). For analysis, CD3− (UCHT1) and CD56+ cells (NCAM16.2; BD Biosciences, San Jose, CA) were gated. KIR phenotype analysis was conducted with WinList, v9.0 (Verity Software House, Topsham, ME). For analysis of expression of natural cytotoxicity receptors and NK cell G2D, the following antibodies were used: NKp30 (p30-15), NKp44 (P44-8), NKp46 (9E2), and NK cell G2D (1D11; all Biolegend). HLA status was recognized by W6/32 (Biolegend).
Statistical analysis
Student’s paired t test, one-way ANOVA, and multiple regression analysis were used to calculate statistical significance between groups (defined as P ≤ 0.05). All analyses were conducted with JMP Pro 12 (SAS Institute Inc., Cary, NC).
Results
Development and validation of an assay for NK cell-mediated cytotoxicity against neuroblastoma cells
Most assays of NK cell-mediated killing of tumor cells use purified peripheral blood NK cells and target tumor cells in suspension [17, 18]. The advantage of this approach is that flow cytometry-based quantification of target-cell viability and studies of NK cell properties can be conducted at the same time. However, these methods are suboptimal for neuroblastoma cells because they are adherent, and their dissociation from culture plates can lead to cell death (Supplementary Fig. 1). Therefore, we developed an assay in which purified NK cells (Fig. 1a) were added to neuroblastoma cells in a 96-well plate, and NK cell-mediated cytotoxicity was analyzed in situ (Fig. 1b). Following co-incubation of effector and target cells, viable neuroblastoma cells were stained with calcein-AM and quantified by semiautomated confluence analysis (Fig. 1c). Residual NK cells were excluded from the analysis by their smaller size.
Development and validation of an assay to quantify NK cell-mediated cytotoxicity and ADCC in neuroblastoma cells. a Isolation of NK cells from peripheral whole blood yielded a highly purified CD56+/CD3− population (98%) compared with that of the buffy coat (13%). b Images produced in differential interference contrast (DIC) microscopy are shown. For the ADCC assay, neuroblastoma cells were plated into a 96-well plate and incubated with NK cells (solid arrow) ± Hu14.18K322A (t = 0 h). The number of neuroblastoma cells per well was counted to calculate the E:T ratio. After 12 h (t = 12 h), most NK cells were washed off with a small amount aggregated on neuroblastoma cells (dashed arrow). Viable cells were stained with calcein-AM and imaged by semiautomated microscopy. c Binary segmentation of the original image was performed with Fiji to determine cell confluence. d The effect of NK cell-mediated ablation (dark gray bars) and ADCC with Hu14.18K322A (light gray bars) was compared in resting and IL-2-activated NK cells (50 IU/mL) across nine neuroblastoma cell lines. The E:T ratio was 5:1 with a 12 h incubation time. e Two neuroblastoma cell lines were studied in co-culture by live-cell imaging. The E:T ratio was 5:1. The number of dead cells with ADCC and NK cell-mediated cytotoxicity was determined over time for NB-1691 (red line) and SK-N-SH (black line). Most significant differences between cell lines were seen with a 12-h incubation time.DIC differential interference contrast
We selected nine neuroblastoma cell lines spanning the spectrum of GD2 and HLA expression (Supplementary Table 1). HLA expression of neuroblastoma cells was studied by flow cytometry and compared to the HLA-negative cell line K562 and peripheral blood to classify HLA expression as low, intermediate, or normal. Purified peripheral blood NK cells from healthy donors were used as effector cells, and the expression of CD158a, CD158b, CD158e1, NKp30, NKp44, NKp46, and NKG2D was determined by flow cytometry (Supplementary Figures 2 and 3). IL-2 at a concentration of 50 IU/mL was used for NK cell activation. ADCC was induced by Hu14.18K322A, which is 98% humanized and contains an alanine substitution at lysine 322 to decrease allodynia and complement-dependent cytotoxicity [19]. We used concentrations of 10 µg/mL of Hu14.18K322 as described in previous studies [20]. We optimized the incubation times and E:T ratios across all neuroblastoma cell lines for ADCC, which were 12 h and 5–1, respectively, because it was the shortest time to achieve statistically significant differences in normalized relative cell killing across multiple neuroblastoma cell lines (Fig. 1d).
Live-cell imaging was used as an independent method for assay validation. In a co-culture experiment, we quantitated specific lysis by allogeneic NK cells against two neuroblastoma cell lines with low (SK-N-SH) and high GD2 expression (NB-1691). Specific lysis induced by Hu14.18K322A was significantly higher in NB-1691 than in SK-N-SH at 12 h (both P < 0.001; Fig. 1e). In absence of Hu14.18K322A, this difference was statistically greater at 12 h (P < 0.001) than at 4 h (P = 0.042). We used these conditions for all subsequent experiments.
Because dissociated cells from O-PDXs tend to grow in aggregates, confluence analysis by quantitative microscopy was not ideal to assess cell viability. Instead, we used the CellTiter-Glo luminescent cell viability assay (Fig. 2a) to determine viability relative to the confluence of cells growing in two dimensions (Fig. 2b).
Development of an assay to quantify NK cell-mediated cytotoxicity and ADCC in O-PDXs a Dissociated tumor cells from O-PDXs were plated for the ADCC assay. IL-2 activated or resting NK cells were added ± Hu14.18K322A (t = 0 h) and incubated for 12 h. The CellTiter-Glo luminescent cell viability assay was used to quantify ADCC. b ADCC results are plotted as relative light units (RLU) correlate with confluence in cells that are growing in two dimensions. RLU relative light units
IL-2 improves ADCC and NK cell-mediated cytotoxicity
Previous studies used peripheral blood mononuclear cells to demonstrate the enhancing effect of IL-2 on ADCC induced by anti-GD2 antibody against neuroblastoma [21]. Although it is known that IL-2 specifically augments NK cell function [11, 22], the reported ADCC effect in these studies cannot unambiguously be attributed to NK cells. We prestimulated purified human NK cells with physiologic and supraphysiologic doses of recombinant IL-2 (rIL-2) for 24 h before conducting ADCC assays. Stimulated NK cells expressed higher levels of NKp30 (P = 0.037), NKp44 (P < 0.001), and NKG2D (P < 0.001), relative to that of resting NK cells (Supplementary Figure 3). The cell line SK-N-MM has normal expression of HLA and inhibitory KIR ligands of KIR2DL1, KIR2DL2/3, and KIR3DL1, and has high levels of GD2. This cell line should be least susceptible to HLA–KIR mismatch and therefore most suitable to assess specific lysis due to ADCC by resting and IL-2-activated NK cells at different time points. IL-2 increased ADCC in a dose-dependent manner, and the cytotoxic effect of Hu14.18K322A was most apparent when NK cells were preactivated with 50 IU/mL IL-2 (Fig. 3a). To quantify ADCC with Hu14.18K322A under these conditions, NK cells from three donors were tested with the nine neuroblastoma cell lines by three serial 1000-fold dilutions of Hu14.18K322A. In resting NK cells, the highest antibody concentration of Hu14.18K322A (10 µg/mL) improved ADCC, compared with that of lower concentrations (Fig. 3b). The specific lysis was highest with IL-2 preactivated NK cells and antibody doses of Hu14.18K322A of > 10 ng/mL (Fig. 3b, c). As expected, specific lysis in the GD2-deficient cell line SH-SY5Y did not improve with the addition of Hu14.18K322A (Fig. 3c).
IL-2 enhances NK cell-mediated ADCC in neuroblastoma cells. a NK cells were prestimulated with IL-2 concentrations ranging from 0 to 5000 IU/mL for 24 h and subsequently tested with the SK-N-MM neuroblastoma cell line at different E:T ratios. The assays were conducted with (gray bar) and without Hu14.18K322A (black bar). The cytotoxic effect of Hu14.18K322A was statistically significant across multiple E:T ratios when NK cells were preactivated with 50 IU/mL IL-2. NK cells from three allogeneic donors were tested in nine neuroblastoma cell lines (b) Three serial dilutions of Hu14.18K322A were used [High (H): 10 µg/mL, Med (M): 10 ng/mL, and Low (L): 10 pg/mL] to induce ADCC. The highest antibody concentration yielded better median specific lysis (black bar) in resting NK cells, but a reduced concentration (10 ng/mL) was equally efficacious when concomitantly administered with IL-2. c Results for individual neuroblastoma cell lines are shown in which IL-2 preactivated NK cells showed equivalent cytotoxicity with lower antibody doses. The highest antibody concentration yielded better median specific lysis in NB-1691 with resting and IL-2 preactivated NK cells. ADCC was comparable to NK cell-mediated cytotoxicity in the GD2-deficient cell line SH-SY5Y
ADCC is more effective than “missing-self” recognition for NK cell degranulation
During NK cell education, NK cells balance their activating and inhibitory receptors to not only ensure self-tolerance, but also recognize pathologic states associated with loss of HLA class I expression (i.e., “missing-self”; Fig. 4a), a process referred to as rheostat model [23, 24]. Consequentially, NK cell education will give rise to a population of NK cells that express a balanced repertoire of activating and inhibitory cell surface receptors and are responsive to stimulation and to subsets of NK cells that lack receptors for self-HLA class I molecules but are hyporesponsive to stimulation to prevent autoimmunity [23, 24]. We examined the role of HLA–KIR interactions ex vivo by using two neuroblastoma cell lines that were matched by HLA genotype and GD2 expression but had normal (SK-N-JCI) and low/absent levels of HLA expression (SK-N-SH) compared to white blood cells from buffy coat (normal) and K562 (absent); Fig. 4b. We conducted the ADCC assay with two concentrations of Hu14.18K322A (10 µg/mL and 10 ng/mL) and NK cells from 15 allogeneic donors that were prestimulated with 50 IU/mL of IL-2. As expected, specific lysis by IL-2-activated NK cells was higher in both cell lines, compared with the specific lysis mediated by resting NK cells (Fig. 4c, P < 0.001 for both cell lines). When the effect of ADCC was directly compared between the neuroblastoma cell lines, IL-2-stimulated NK cells induced lysis in more of the HLA-expressing neuroblastoma cells (SK-N-JCI) than in the HLA low-expressing cells (SK-N-SH) (Fig. 4c). The mechanisms leading to higher specific lysis in the presence of IL-2 are unclear. It is possible that other receptor–ligand interactions not measured in this study accounted for these differences. To control for these variables, future experiments could use one cell line with conditional HLA knock-out to assess the effect of HLA–KIR interactions on ADCC.
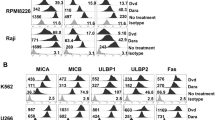
Comparison of ADCC and missing-self recognition for neuroblastoma cell ablation. a Schematic depicting HLA–KIR interactions and the principles of NK cell-mediated cytotoxicity. b The SK-N-SH neuroblastoma cell line demonstrated downregulation of HLA (red) surface expression, whereas the SK-N-JCI cell line expressed characteristic HLA levels. Isotype is shown in gray. K562 served as negative control and white blood cells from buffy coat as positive control. c Head-to-head comparison of susceptibility to NK cell-mediated cytotoxicity and ADCC. Activated NK cells induced more tumor cell death in SK-N-JCI than in SK-N-SH cells. Resting NK cells did not affect tumor cell death levels. d HLA expression was induced by interferon-γ treatment for 72 h and comparable to buffy coat. e–h Degranulation of NK cells from three donors was assessed by quantifying CD107a expression in single KIR-positive NK cell sub-populations after co-incubation with neuroblastoma cells that genotypically lacked the HLA class I molecules corresponding to CD158a (SK-N-AS), CD158b (NBLS), or CD158e1 (NB-1691). When stratified by KIR sub-population (e), presence of HLA–KIR mismatch between NK cells and tumor cells (f), use of antibody Hu14.18K322A (g), or licensing status and HLA–KIR mismatch (h), the greatest level of NK cell degranulation was noted in CD158b-expressing NK cells (e), in NK cells harboring KIRs that were mismatched against HLA expressed by the respective neuroblastoma cells (f), in the presence of antibody (g), and in licensed NK cells (h). KIR expression and HLA–KIR mismatch status remain statistically significant in a multiple regression analysis
Because the ADCC assay only quantitates tumor cell death, we also measured CD107a expression in NK cells from three donors to study the impact of HLA–KIR interaction on NK cell degranulation. Using the KIR and HLA genotype information from each donor, we determined the NK cell populations that are licensed (expressing KIR that corresponds to donor HLA) and unlicensed (expressing KIR which the donor did not express HLA for; Supplementary Table 2). Subsequently, we co-incubated IL-2-activated NK cells with neuroblastoma cells that genotypically lacked the HLA class I molecules corresponding to CD158a (SK-N-AS), CD158b (NBLS), or CD158e1 (NB-1691) and recreated HLA–KIR ligand mismatch this way. HLA expression was induced by interferon-γ treatment for 72 h (Fig. 4d). A blocking anti-HLA antibody was used to recreate the state of missing self (lack of HLA–KIR interaction), and Hu14.18K322A was used to induce ADCC. The highest levels of CD107a expression were present in NK cells expressing CD158b (P < 0.001; Fig. 4e), harboring KIRs that were mismatched against HLA expressed by the respective neuroblastoma cells (P = 0.016; Fig. 4f), in the presence of antibody (P < 0.001; Fig. 4g), and in licensed NK cells (P < 0.05; Fig. 4h). KIR expression and HLA–KIR mismatch status remain statistically significant in a multiple regression analysis. Collectively, these data suggest that higher NK cell-mediated activity may be achieved via recruitment of the licensed NK cell population and in the setting of anti-GD2 antibody and HLA–KIR mismatch aside from other signals.
Neuronal differentiation enhances ADCC
Because neuroblastoma tumors comprise neuroblastic cells (N-type), GD2-negative Schwann cell-like stroma cells (S-type), or both cell types (I-type), the expression of the neuronal marker GD2 can vary between and within tumors [7]. To determine what effect neuronal differentiation may have on susceptibility to ADCC, neuroblastoma cells were cultured in ATRA for 72 h before being subjected to the ADCC assay. GD2 expression was determined by flow cytometry, and gene expression of differentiated neuroblastoma cells were compared with that of untreated cells. All cells were assigned a cell type designation (N-, S-, or I-type) according to their morphology.
N-type and I-type cells increased neurite outgrowth, which did not occur in S-type cells (Fig. 5a). This morphologic change was associated with an up-regulation of genes involved in ATRA metabolism (CYP26A1/B1, DHRS3; Fig. 5b) and binding (CRABP1/2, RARB, RBP1; Fig. 5c). Other genes that were found to be differentially expressed in ATRA-treated cells encode for proteins involved in cell structure, the MAPK and NOTCH1 signaling pathway, neuronal differentiation, and angiogenesis (Supplementary Table 3).
Effect of neuroblastoma differentiation on NK cell-mediated ADCC and ADCC. a After exposure to ATRA for 72 h, neurite outgrowth was present in N-type and I-type cells (solid arrows). No changes in morphology were noted in some I-type cells and most S-type cells (dashed arrows). b, c Differential gene expression of ATRA-binding proteins (b) and enzymes involved in ATRA metabolism (c) after differentiation of neuroblastoma cells. d Flow cytometry analysis of GD2. For all but two cell lines (SK-N-SH and SH-SY5Y), the percentage of GD2-expressing cells after ATRA-induced differentiation was unchanged, compared with that in untreated cells. e ADCC assays using 2 allogeneic donors against 10 neuroblastoma cell lines (listed in Supplementary Table 1) were conducted. Each dot refers to the average specific lysis per cell line for the respective experimental condition. Statistically significantly (***) higher median specific lysis (black bar) by resting NK cells and Hu14.18K322A was noted after differentiation with ATRA
A high percentage of GD2-positive cells were present among the neuroblastoma cell lines (median 83.9%; range 44.0–98.9%) with exception of SH-SY5Y cells (mean 2.9 ± 0.7%; Fig. 5d). The percentage of GD2-positive cells did not change after ATRA treatment (median 78.5%; range 1.3–98.5%; Fig. 5d). The mean fluorescence intensity for GD2 ranged broadly (median 1001; range 189–32,461), but did not significantly change after neuronal differentiation (median 1332; range 203–16,402; P > 0.05). ADCC was higher in differentiated neuroblastoma cells when induced by resting NK cells (P = 0.004). For all other conditions, specific lysis of ATRA-treated cells was not different than that in untreated cells (Fig. 5e).
Individualized testing of ADCC is possible with O-PDXs and matched NK cells from individual patients with neuroblastoma
To test ADCC of individual patients in the laboratory, we conducted ADCC assays with O-PDXs and NK cells matched from the same donor. The O-PDX SJNBL108_X expressed high levels of GD2, as detected by flow cytometry, and a second O-PDX SJNBL013761_X1 was deficient in GD2 (Fig. 6a). CD158b-expressing NK cells were the predominant KIR-expressing NK cell population in the peripheral blood of the SJNBL108_X donor, and CD158a-expressing NK cells were predominant for the SJNBL013761_X1 donor (Fig. 6b). Both O-PDXs were susceptible to ADCC when induced with Hu14.18K322A, which was unexpected for SJNBL013761_X1 because it did not express any appreciable levels of GD2 (Fig. 6c). This could be due to expression of other compensatory surface molecules, such as HLA class I, although we did not test this. The SJNBL013761_X1 O-PDX was resistant to NK cell-mediated cytotoxicity without antibody, even when the NK cells were stimulated with IL-2. Live-cell imaging supported this observation.
ADCC assays with matched O-PDXs and patient NK cells. a, b Flow cytometry plots are shown depicting GD2 expression (a) and KIR phenotype (b) in the SJNBL108_X and SJNBL013761_X1 O-PDXs. c ADCC assay results for SJNBL108_X and SJNBL013761_X1 are plotted as relative light units (RLU). RLU relative light units
Discussion
High-risk neuroblastoma is one of the most common solid tumors of childhood [25]. Despite the use of immunotherapy and differentiation therapy in the multimodal treatment regimen for these patients, a third of affected children experience treatment failure within the first 2 years of therapy, and more than 50% suffer from dose-limiting toxicities [6, 26]. We studied the contribution of IL-2, anti-GD2 antibody therapy, ATRA, and HLA–KIR mismatch in NK cell-mediated cytotoxicity of neuroblastoma cells with the aim to better understand the cellular mechanisms of NK cell-mediated ADCC. The results of our study point to several potential strategies that warrant further validation in vivo to improve immunotherapy for patients with neuroblastoma.
Many studies have described the enhancing effect of IL-2 on NK cell growth and survival and suggested a supporting role in ADCC [11, 27, 28]. However, therapeutic administration of IL-2 has been limited in the clinic by the considerable toxicity associated with high doses [29]. For example, in the latest high-risk neuroblastoma study by the European International Society of Pediatric Oncology Neuroblastoma Group, 44% of patients who received high-dose rIL-2 at 6 × 106 IU/m2 by subcutaneous injection were unable to tolerate the regimen and had to terminate their treatment prematurely [30]. The investigators of this study questioned the therapeutic role of rIL-2 in their trial, given that they did not find a survival benefit with the use of rIL-2. However, the findings may have been confounded by the high dropout rate of patients in the IL-2 treatment arm [30]. Our data show that IL-2 improves ADCC in culture and support the continued use of this cytokine in neuroblastoma immunotherapy. The IL-2 concentration that we used is tolerable and physiologically achievable, falling within the range of serum levels from adult and pediatric pharmacokinetic studies [29, 31]. Therefore, we argue that low doses of IL-2 may be an efficacious yet better tolerated option for children with neuroblastoma. ADCC is enhanced by greater IL-2 activation and anti-GD2 antibody concentration (of > 10 ng/mL) until this effect reaches a plateau in vitro. In the future, we suggest comparing several doses of Hu14.18K322A in combination with IL-2 in preclinical studies to determine which dose combination may yield the best anti-tumor effect. Clinically, dose de-escalation of anti-GD2 antibody therapy could result in better tolerability because it may decrease antibody-related pain, which is dose-dependent and currently managed in the clinic with preemptive administration of morphine and decreased anti-GD2 antibody infusion rates, extending up to 10 days (NCT01857934) [32].
NK cell-based therapy found applicability in the clinic after evidence emerged that individuals with acute myeloid leukemia who receive bone marrow transplants with HLA–KIR mismatch have improved long-term survival [10]. For neuroblastoma, NK cell therapy could be exploited as either part of anti-GD2 antibody therapy or cancer-directed immunosurveillance [33, 34], but the cellular mechanisms are less clearly understood in neuroblastoma than in acute myeloid leukemia. We found that ADCC was a strong signal for NK cell degranulation. Therefore, adoptive transfer of allogeneic NK cells may be more effective when given with antibody. We also observed that NK cells of all of our donors express CD158b and were licensed and predominantly active, whereas other NK cell populations exhibited less degranulation. CD158b (KIR2DL2/3) and HLA-C1 ligands are the most common KIR allele and HLA among the Caucasian population [35]. The cumulative number of Caucasians with HLA-C allotypes with asparagine at position 80 corresponding to CD158b approximates a third in this ethnic group [35]. Therefore, it is likely to have a donor with licensed and potentially active NK cell that express CD158b and could explain our findings. However, it is unclear how NK cell education preferentially expands the CD158b-expressing sub-population. Our findings also raise the question if selection of suitable NK cell donors which is based primarily on donor KIR genotype and recipient HLA genotype should be expanded to determine the fraction of active and hypoactive NK cell populations according to the HLA and KIR genotype of the donor. We will further validate these data with cells isolated from additional donors in ex vivo and animal model studies.
Previous studies of neuroblastoma cell death in culture compensated for un-induced levels of cell death by removing neuroblastoma cells from culture plates by normalizing assay results. Although this is an effective approach, the nine neuroblastoma cell lines we tested had very different intrinsic sensitivities to flow cytometry-based cytotoxicity assays. Therefore, we developed a new assay that minimized basal levels of cell death. We conducted a large series of ADCC assays with this method, demonstrating its feasibility. Unlike flow cytometry-based assays that have a very high sensitivity in detecting membrane disintegrity with viability staining, our ADCC assay required the tumor cells to have undergone cell death to quantify specific lysis. Therefore, our assay measures ADCC more conservatively than do flow cytometry-overing from an NK cell assault.
Importantly, we isolated NK cells from the peripheral blood of healthy de-identified allogeneic blood donors to assess ADCC by resting and IL-2 activated NK cells. Because of donor de-identification, each experiment was conducted with fresh cells from a different donor. Because the level of NK cell-mediated cytotoxicity may vary among individuals, comparing ADCC within an experiment with NK cells from one donor rather than between experiments with NK cells from different donors may lead to more biologically meaningful conclusions.
GD2 expression remained stable after ATRA-induced differentiation, which was expected because GD2 is a marker found in mature neurons [36]. Susceptibility to ADCC was improved after ATRA treatment. This is clinically relevant because patients receive anti-GD2 antibody therapy combined with ATRA [6]. Although not studied here, ATRA can induce higher expression of NKG2D ligands [37]. NKG2D serves as global co-stimulatory signal for various ITAM-associated pathways in NK cells, including CD16 signaling [38]. Although this could have been a plausible explanation as to why ATRA-treated tumors are highly susceptible to ADCC by anti-GD2 antibody alone without the need of IL-2 activation of NK cells, RNA sequencing did not reveal differential expression of the respective genes. Therefore, at this point, the mechanisms behind this are unclear, and future molecular studies are needed to explain the observed differences. In concordance with prior reports [39], the morphology of ATRA-differentiated neuroblastoma cells varied greatly and could be due to differential expression of ATRA effector genes. For example, RARB and CRABP2 are upregulated in good differentiator cells and function as regulatory binding proteins that induce the transcription of ATRA target genes [40]. The transcriptional effects of ATRA also depend on its cellular concentration. Enzymes belonging to the CYP26 family are mainly responsible for ATRA homeostasis and were upregulated as well. Whether or not these genes can be used to predict differentiation efficiency warrants further studies.
We have demonstrated the feasibility of conducting tissue-matched ADCC experiments with patient NK cells and O-PDXs. Characterizing effector and tumor cells and conducting ADCC assays for individual patients in the laboratory may provide a valuable opportunity to identify and validate predictive biomarkers for therapy success and to study the potential vulnerabilities of tumor cells. Together, our findings highlight several potential ways to improve immunotherapy for patients with neuroblastoma and warrant further validation in vivo.
Abbreviations
- ADCC:
-
Antibody-dependent cell-mediated cytotoxicity
- ATRA:
-
All-trans retinoic acid
- E:T:
-
Effector cell to target cell
- EMEM:
-
Eagle’s minimum essential medium
- GD2:
-
Disialoganglioside
- HLA:
-
Human leukocyte antigen
- IL-2:
-
Interleukin-2
- KIR:
-
Killer-cell immunoglobulin-like receptor
- NK:
-
Natural killer
- O-PDX:
-
Orthotopic patient-derived xenograft
- rIL-2:
-
Recombinant interleukin-2
References
Zent CS, Chen JB, Kurten RC et al (2004) Alemtuzumab (CAMPATH 1H) does not kill chronic lymphocytic leukemia cells in serum free medium. Leuk Res 28:495–507. https://doi.org/10.1016/j.leukres.2003.09.011
Brentjens RJ, Davila ML, Riviere I et al (2013) CD19-targeted T cells rapidly induce molecular remissions in adults with chemotherapy-refractory acute lymphoblastic leukemia. Sci Transl Med 5:177ra38. https://doi.org/10.1126/scitranslmed.3005930
Larkin J, Chiarion-Sileni V, Gonzalez R et al (2015) Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med 373:23–34. https://doi.org/10.1056/NEJMoa1504030
Slamon DJ, Leyland-Jones B, Shak S et al (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344:783–792. https://doi.org/10.1056/NEJM200103153441101
Hurwitz H, Fehrenbacher L, Novotny W et al (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350:2335–2342. https://doi.org/10.1056/NEJMoa032691
Yu AL, Gilman AL, Ozkaynak MF et al (2010) Anti-GD2 Antibody with GM-CSF, Interleukin-2, and Isotretinoin for Neuroblastoma. N Engl J Med 363:1324–1334. https://doi.org/10.1056/NEJMoa0911123
Schulz G, Cheresh DA, Varki NM et al (1984) Detection of ganglioside GD2 in tumor tissues and sera of neuroblastoma patients. Cancer Res 44:5914–5920
Janeway CA Jr, Travers P, Walport M et al (2001) Immunobiology: The Immune System in Health and Disease. 5th edn. New York: Garland Science. The destruction of antibody-coated pathogens via Fc receptors. http://www.ncbi.nlm.nih.gov/books/NBK27171/. Accessed 6 May 2017
Kärre K, Ljunggren HG, Piontek G, Kiessling R (1986) Selective rejection of H-2-deficient lymphoma variants suggests alternative immune defence strategy. Nature 319:675–678. https://doi.org/10.1038/319675a0
Ruggeri L, Mancusi A, Capanni M et al (2007) Donor natural killer cell allorecognition of missing self in haploidentical hematopoietic transplantation for acute myeloid leukemia: challenging its predictive value. Blood 110:433–440. https://doi.org/10.1182/blood-2006-07-038687
Henney CS, Kuribayashi K, Kern DE, Gillis S (1981) Interleukin-2 augments natural killer cell activity. Nature 291:335–338. https://doi.org/10.1038/291335a0
Villablanca JG, Khan AA, Avramis VI et al (1995) Phase I trial of 13-cis-retinoic acid in children with neuroblastoma following bone marrow transplantation. J Clin Oncol 13:894–901. https://doi.org/10.1200/JCO.1995.13.4.894
Stewart E, Shelat A, Bradley C et al (2015) Development and characterization of a human orthotopic neuroblastoma xenograft. Dev Biol 407:344–355. https://doi.org/10.1016/j.ydbio.2015.02.002
Downing JR, Wilson RK, Zhang J et al (2012) The pediatric cancer genome project. Nat Genet 44:619–622. https://doi.org/10.1038/ng.2287
Anders S, Pyl PT, Huber W (2015) HTSeq–a Python framework to work with high-throughput sequencing data. Bioinformatics 31:166–169. https://doi.org/10.1093/bioinformatics/btu638
André P, Biassoni R, Colonna M et al (2001) New nomenclature for MHC receptors. Nat Immunol 2:661. https://doi.org/10.1038/90589
Brunner KT, Mauel J, Cerottini JC, Chapuis B (1968) Quantitative assay of the lytic action of immune lymphoid cells on 51-Cr-labelled allogeneic target cells in vitro; inhibition by isoantibody and by drugs. Immunology 14:181–196
Cederbrant K (2005) Natural killer cell assay. In: Vohr H-W (ed) Encyclopedic reference of immunotoxicology. Springer, Berlin, pp 469–472
Sorkin LS, Otto M, Baldwin WM et al (2010) Anti-GD2 with an FC point mutation reduces complement fixation and decreases antibody-induced allodynia. Pain 149:135–142. https://doi.org/10.1016/j.pain.2010.01.024
Alderson KL, Luangrath M, Elsenheimer MM et al (2013) Enhancement of the anti-melanoma response of Hu14.18K322A by αCD40 + CpG. Cancer Immunol Immunother 62:665–675. https://doi.org/10.1007/s00262-012-1372-8
Hank JA, Surfus J, Gan J et al (1994) Treatment of neuroblastoma patients with antiganglioside GD2 antibody plus interleukin-2 induces antibody-dependent cellular cytotoxicity against neuroblastoma detected in vitro. J Immunother Emphas Tumor Immunol 15:29–37
Rossi AR, Pericle F, Rashleigh S et al (1994) Lysis of neuroblastoma cell lines by human natural killer cells activated by interleukin-2 and interleukin-12. Blood 83:1323–1328
Brodin P, Lakshmikanth T, Johansson S et al (2009) The strength of inhibitory input during education quantitatively tunes the functional responsiveness of individual natural killer cells. Blood 113:2434–2441. https://doi.org/10.1182/blood-2008-05-156836
Joncker NT, Fernandez NC, Treiner E et al (2009) NK cell responsiveness is tuned commensurate with the number of inhibitory receptors for self-MHC class I: the rheostat model. J Immunol 182:4572–4580. https://doi.org/10.4049/jimmunol.0803900
Howlander N, Noone A, Krapcho M et al (2011) SEER Cancer Statistics Review, 1975–2009. National Cancer Institute, Bethesda
Navid F, Sondel PM, Barfield R et al (2014) Phase I trial of a novel anti-GD2 monoclonal antibody, Hu14.18K322A, designed to decrease toxicity in children with refractory or recurrent neuroblastoma. J Clin Oncol 32:1445–1452. https://doi.org/10.1200/JCO.2013.50.4423
Grimm EA, Mazumder A, Zhang HZ, Rosenberg SA (1982) Lymphokine-activated killer cell phenomenon. Lysis of natural killer-resistant fresh solid tumor cells by interleukin 2-activated autologous human peripheral blood lymphocytes. J Exp Med 155:1823–1841
Hank JA, Robinson RR, Surfus J et al (1990) Augmentation of antibody dependent cell mediated cytotoxicity following in vivo therapy with recombinant interleukin 2. Cancer Res 50:5234–5239
Ribeiro RC, Rill D, Roberson PK et al (1993) Continuous infusion of interleukin-2 in children with refractory malignancies. Cancer 72:623–628
Ladenstein R, Poetschger U, Gray J et al (2016) Toxicity and outcome of anti-GD2 antibody ch14.18/CHO in front-line, high-risk patients with neuroblastoma: final results of the phase III immunotherapy randomisation (HR-NBL1/SIOPEN trial). J Clin Oncol 34(15_suppl):Abstract 10500
Atkins MB, Gould JA, Allegretta M et al (1986) Phase I evaluation of recombinant interleukin-2 in patients with advanced malignant disease. J Clin Oncol 4:1380–1391. https://doi.org/10.1200/JCO.1986.4.9.1380
Lode H, Siebert N, Kietz S et al (2013) Long-term continuous infusion of anti-GD2 antibody CH14.18/CHO in relapsed/refractory neuroblastoma patients. J Immunother Cancer 1(1_suppl):Abstract P244
Delgado DC, Hank JA, Kolesar J et al (2010) Genotypes of NK Cell KIR Receptors, Their Ligands, and Fc Receptors in the Response of Neuroblastoma Patients to Hu14.18-IL2 Immunotherapy. Cancer Res 70:9554–9561. https://doi.org/10.1158/0008-5472.CAN-10-2211
Venstrom JM, Zheng J, Noor N et al (2009) KIR and HLA genotypes are associated with disease progression and survival following autologous hematopoietic stem cell transplantation for high-risk neuroblastoma. Clin Cancer Res 15:7330–7334. https://doi.org/10.1158/1078-0432.CCR-09-1720
Marsh SGE, Parham P, Barber LD (2000) The HLA factsbook. Academic Press, San Diego
Jin HJ, Nam HY, Bae YK et al (2010) GD2 expression is closely associated with neuronal differentiation of human umbilical cord blood-derived mesenchymal stem cells. Cell Mol Life Sci 67:1845–1858. https://doi.org/10.1007/s00018-010-0292-z
Zou Z, Nomura M, Takihara Y et al (1996) Isolation and characterization of retinoic acid-inducible cDNA clones in F9 cells: a novel cDNA family encodes cell surface proteins sharing partial homology with MHC class I molecules. J Biochem 119:319–328
Ho EL, Carayannopoulos LN, Poursine-Laurent J et al (2002) Costimulation of multiple NK cell activation receptors by NKG2D. J Immunol 169:3667–3675. https://doi.org/10.4049/jimmunol.169.7.3667
Reynolds CP, Kane DJ, Einhorn PA et al (1991) Response of neuroblastoma to retinoic acid in vitro and in vivo. Prog Clin Biol Res 366:203–211
Schug TT, Berry DC, Shaw NS et al (2007) Opposing effects of retinoic acid on cell growth result from alternate activation of two different nuclear receptors. Cell 129:723–733. https://doi.org/10.1016/j.cell.2007.02.050
Acknowledgements
We thank Merck Serono and the Children’s GMP, LLC for providing the Hu14.18K322A anti-GD2 antibody to conduct our studies. We also thank the Biological Resource Branch at the National Cancer Institute for providing rIL-2 used in the present study. We thank Drs. Jennifer Peters and Abbas Shirinifard for optimizing the automated microscopy protocol and optimizing the classifier for segmentation purposes in Fiji, respectively. We thank Dr. Dan Kaufman for reviewing the manuscript. We thank Nisha Badders for scientific editing.
Funding
This work was supported, in part, by Cancer Center Support (CA21765) from the NCI, grants to M.A.D. from the NIH (EY014867 and EY018599 and CA168875). This research was supported by HHMI.
Author information
Authors and Affiliations
Contributions
RN: experimental design, conduction of experiments, analysis and interpretation of data, draft of the manuscript. JH: experimental design, conduction of flow cytometry experiments, review of the manuscript. WKC: experimental design, interpretation of data, review of the manuscript. DF: analysis of RNA sequencing data, review of the manuscript. MAD: experimental design, analysis and interpretation of data, review of manuscript, funding.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and ethical standards
Patient consented to donate biological material (blood and tumor) as part of an ongoing institutional protocol XPD09-234 MAST—MOLECULAR ANALYSIS OF SOLID TUMORS. This protocol was approved by the St. Jude Children’s Research Hospital IRB.
Animal source
All animals were handled according to IACUC approved policies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nguyen, R., Houston, J., Chan, W.K. et al. The role of interleukin-2, all-trans retinoic acid, and natural killer cells: surveillance mechanisms in anti-GD2 antibody therapy in neuroblastoma. Cancer Immunol Immunother 67, 615–626 (2018). https://doi.org/10.1007/s00262-017-2108-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-017-2108-6