Abstract
Objective
To retrospectively compare inter- and intra-reader agreement of abbreviated MRCP (aMRCP) with comprehensive MRI (cMRCP) protocol for detection of worrisome features, high-risk stigmata, and concomitant pancreatic cancer in pancreatic cyst surveillance.
Methods
151 patients (104 women, mean age: 69[10] years) with baseline and follow-up contrast-enhanced MRIs were included. This comprised 138 patients under cyst surveillance with 5-year follow-up showing no pancreatic ductal adenocarcinoma (PDAC), 6 with pancreatic cystic lesion-derived malignancy, and 7 with concomitant PDAC. The aMRCP protocol used four sequences (axial and coronal Half-Fourier Single-shot Turbo-spin-Echo, axial T1 fat-saturated pre-contrast, and 3D-MRCP), while cMRCP included all standard sequences, including post-contrast. Three blinded abdominal radiologists assessed baseline cyst characteristics, worrisome features, high-risk stigmata, and PDAC signs using both aMRCP and cMRCP, with a 2-week washout period. Intra- and inter-reader agreement were calculated using Fleiss’ multi-rater kappa and Intra-class Correlation Coefficient (ICC). 95% confidence intervals (CI) were calculated.
Results
Cyst size, growth, and abrupt main pancreatic duct transition had strong intra- and inter-reader agreement. Intra-reader agreement was ICC = 0.93–0.99 for cyst size, ICC = 0.71–1.00 for cyst growth, and kappa = 0.83–1.00 for abrupt duct transition. Inter-reader agreement for cyst size was ICC = 0.86 (aMRCP) and ICC = 0.83 (cMRCP), and for abrupt duct transition was kappa = 0.84 (aMRCP) and kappa = 0.69 (cMRCP). Thickened cyst wall, mural nodule and cyst-duct communication demonstrated varying intra-reader agreements and poor inter-reader agreements.
Conclusion
aMRCP showed high intra- and inter-reader agreement for most pancreatic cyst parameters that highly rely on T2-weighted sequences.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pancreatic cystic lesions (PCLs), often interchangeably called Branch–Duct Intraductal Papillary Mucinous Neoplasms (BD-IPMNs), are increasingly detected on imaging studies, with a prevalence approaching 50% on MRI [1]. Long-term surveillance studies of PCLs report an estimated incidence of malignancy arising from these PCLs (PCL derived malignancy) from 1.8 to 4.3% at 5 years [2,3,4,5,6] and up to 15% in 15 years [4]. In addition, concomitant cancer can arise away from PCLs, elsewhere in the pancreas, due to a “field defect” associated with PCLs [7].
Pancreatic cancer has a dismal 5-year survival rate as most patients present with locally advanced or metastatic disease [8]. However, patients presenting with stage 1A pancreatic cancer have a 5-year survival of up to 83.7% [9]. Therefore, major societal guidelines, including the American Gastroenterology Association (AGA), the American College of Gastroenterology (ACG), the American College of Radiology (ACR), the European Evidence-Based, and the International Association of Pancreatology (IAP)/Fukuoka guidelines [10,11,12,13,14] recommend long-term surveillance of pancreatic cysts, often with magnetic resonance imaging/magnetic resonance cholangiopancreatography (MRI/MRCP), hereafter referred to as MRI, with the goal of early detection of PCL derived pancreatic cancer.
MRI, typically with and without intravenous contrast, is often the imaging modality of choice for cyst surveillance given its excellent tissue characterization, avoidance of ionizing radiation, and the ability to perform the heavily T2-weighted MRI sequences. However, patient discomfort, time, and cost associated with intravenous contrast administration, as well as concern about gadolinium deposition in the brain [15] have sparked interest in an abbreviated MRI protocol without utilizing intravenous contrast.
Therefore, the purpose of our study was to retrospectively assess intra- and inter-reader agreement of an abbreviated MRI (aMRCP) and a comprehensive MRI (cMRCP) protocol for PCL surveillance, assessment for worrisome features or high-risk stigmata, and detection of concomitant pancreatic cancer.
Methods
This retrospective study was approved by our Institutional Review Board and performed in compliance with the Health Insurance Portability and Accountability Act. The requirement for informed consent was waived. The study cohort included three groups of patients with PCLs: (a) patients undergoing routine PCL surveillance, (b) pathologically proven cases of PCL derived malignancy (high-grade dysplasia and/or invasive carcinoma), and c) PCL with concomitant PDAC elsewhere in the pancreas. The last group is included because of the reported increased incidence of concomitant PDAC associated with PCL owing to the “field defect” theory [7, 16, 17], and therefore the need to assess how well aMRCP and cMRCP are at detecting secondary signs of concomitant PDAC.
Patients
A retrospective departmental database search was performed to identify adults (≥ 18 years) who underwent an MRI for pancreatic cyst follow-up from January 2017 through December 2017 and a prior baseline contrast-enhanced MRI at least 1 year earlier. The search terms for the “Indication” in the radiology reports included: “pancreatic cyst-”, “pancreatic IPMN-”, or “intraductal pancreatic mucinous neoplasm follow up”. Specific inclusion criteria for this study were (1) baseline cMRCP for comparison; (2) follow up contrast-enhanced cMRCP for cyst surveillance; (3) at least 5 years of clinical or imaging follow-up confirming no subsequent pancreatic cancer diagnosis for these patients undergoing PCL surveillance. Patients that had prior pancreatic surgery were excluded.
Pathology database query
In order to enrich the study population with cases of malignancy (high-grade dysplasia and invasive carcinoma) arising from BD-IPMNs, the pathology database was searched by an abdominal radiologist (CH) from 2014 to 2020 for patients that have undergone pancreatic resections for the indications of “pancreatic cyst” or “intraductal mucinous cystic neoplasm”. These patients must have also had 2 MRIs that are at least 1 year apart.
Pancreatic tumor board conference database query
Two authors (CH and BD) reviewed cases from weekly pancreatic tumor board conferences from 2017 to identify pathologically proven primary PDAC that had at least 1 coexisting cyst elsewhere in the pancreas. The images showed no biliary stents, pancreatic stents, or metastases. These patients must have had 2 MRIs that are at least 1 year apart.
Comprehensive MRI protocol (Table 1)
All patients underwent a cMRCP on either 1.5T and 3.0T MRI systems. Patients fasted for 4 h prior to the MRI examination and drank 1 cup of water mixed with 1 mL of gadolinium-based contrast immediately before the examination in order to suppress fluid signal from stomach and proximal small bowel (Gadobutrol, Bayer HealthCare, Whippany, NJ). A phased array flex coil covered the patient’s abdomen. The sequences included in the cMRCP are as follows: coronal half-Fourier acquisition single-shot turbo spin echo (HASTE), axial HASTE, axial in and out of phase, diffusion-weighted imaging with 3 b-values (b-50, b-400 and b-800), axial T1 fat-suppressed pre- and post-contrast (3 post contrast acquisitions at 5, 60 and 180 s using bolus tracking) and delayed coronal volumetric interpolated breath-hold examination (VIBE) after the initiation of intravenous contrast (Gadobutrol, 0.1 mmol/kg). Coronal oblique (covering pancreatic duct and biliary tree) 3D MRI and MIP were obtained, and if failed, thick slab coronal oblique T2 weighted sequences were obtained.
Abbreviated MRI technique (Table 1)
A simulated aMRCP including 4 selected sequences from the cMRCP for radiologist review: HASTE (coronal and axial), axial T1 fat suppressed pre-contrast VIBE, and 3D MRI sequences.
Imaging review
Three fellowship trained abdominal radiologists with 4, 2, and 2 years of post-fellowship experience, blinded to initial imaging report and clinical information, performed independent imaging review. All radiologists routinely interpret MRI for pancreatic cyst surveillance during daily clinical practice. Radiologists were aware that this study cohort consisted of patients undergoing pancreatic cyst surveillance, but were not aware that the study included a subset of “enriched” malignant cases. To simulate real world experience in the reading room, radiologists had access to the prior cMRCP images and report for comparison, but were blinded to the surveillance MRI radiology reports and clinical information, endoscopic ultrasound, or pathology results for any of these cases.
All MRI examinations were reviewed on Picture Archiving and Communication System (Intellispace® PACS, Philips Medical Systems Einthoven, Netherlands) in 2 independent reading sessions. The aMRCP were reviewed first and then following a 2-week washout period the cMRCP were reviewed. Radiologists assessed the largest or most suspicious cyst, deemed as the dominant cyst on the MRI study for the following key features according to the ACR 2017 pancreatic cyst white paper [11] (Table 2): cyst multiplicity, size, growth, location, morphology (unilocular versus multilocular), thickened cyst wall (enhancing thickened cyst wall if on cMRCP), mural nodule (both enhancing and non-enhancing mural nodule if on cMRCP), pancreatic duct caliber where widest. Readers also assessed for signs of concomitant PDAC including abrupt pancreatic duct stricture or caliber change, solid pancreatic mass, or peripancreatic vessel (celiac artery, superior mesenteric artery, common hepatic artery, main portal vein and superior mesenteric vein) involvement by soft tissue.
Statistical analysis
Inter-reader agreement between all 3 radiologists was calculated for each item using Fleiss’ multi-rater kappa statistic (κ) and continuous variables were assessed based on the Intra-class Correlation Coefficient (ICC). Ninety-five percent confidence intervals (CI) also were calculated. Diagnostic performance of aMRCP and cMRCP was also assessed using pathology proven PCL derived malignancy and concomitant pancreatic cancers. Kappa value of ≤ 0 is considered no agreement; 0.01- 0.20, none to slight; 0.21–0.40, fair; 0.41–0.60, moderate; 0.61–0.80, substantial; and ≥ 0.81 is considered almost perfect agreement [18]. Statistical comparison of diagnostic performance of aMRCP and cMRCP for PCL derived malignancy and concomitant pancreatic cancer was not performed due to the small sample size (6 and 7 patients, respectively). All statistical analyses were performed by an open source statistical software program R (R Core Team, version 4.3.2; Vienna, Austria). A 2-tailed P value of less than 0.05 was considered to indicate a statistically significant difference.
Results
Patients
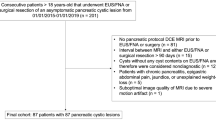
Figure 1 shows the patient inclusion flowchart. 1781 consecutive patients were initially identified by retrospective departmental database search. 150 consecutive patients were identified. 12 patients were excluded due to lack of prior cMRCP or prior pancreatic surgery, leaving 138 patients in the low risk PCL follow-up group. This group of patients had at least 5 years clinical or imaging follow-up to ensure cyst benignity: 106 patients had clinical notes supporting no pancreatic cancer diagnosis and the remaining 32 patients had cross sectional imaging available 5 years later in 2023 without evidence of pancreatic cancer or metastases. Additional 13 patients were added for cohort enrichment as follows (7 concomitant PDAC identified by multidisciplinary tumor board review and 6 with malignant IPMN). Manual review of pathology reports yielded 16 cases of malignancy arising from an IPMN, 10 were excluded due to lack of 2 MRIs, leaving 6 cases of malignancy arising from an IPMN (4 out of 6 were high -grade dysplasia, 2 out of 6 were invasive carcinoma). The final cohort consisted of 151 patients (104 women and 47 men, mean [SD] age: 69[10] years. Table 3 summarizes patient and dominant PCL characteristics.
Intra-reader agreement between aMRCP and cMRCP
Tables 4 shows intra-reader agreement for PCL evaluation. Intra-reader agreement was almost perfect (ICC = 0.93–0.99) for cyst size, strong to almost perfect for cyst growth (ICC = 0.71–1.00) and cyst location (kappa = 0.79–0.99). While 2 readers had almost perfect intra-reader agreement for cyst communication with the main pancreatic duct (kappa = 0.86, 1.00), one reader had fair agreement (kappa = 0.37).
There was also almost perfect intra-reader agreement for abrupt duct transition (kappa = 0.83–1.00). Two readers had almost perfect intra-reader agreement for identification of a solid mass separate from the dominant PCL (kappa = 0.85 and 0.92), however 1 reader had moderate intra-reader agreement (kappa = 0.49). Mural nodule had moderate to almost perfect intra-reader agreement (kappa = 0.41, 0.66, 1.00). Thickened cyst wall had no to fair intra-reader agreement (kappa = 0.09–0.33).
Inter-reader agreement for aMRCP and cMRCP
Tables 5 shows inter-reader agreement for PCL evaluation. There was strong inter-reader agreement for cyst size (ICC = 0.86 and 0.83 for aMRCP and cMRCP, respectively) and pancreatic duct caliber (ICC = 0.80 for aMRCP and 0.82 for cMRCP). There was moderate inter-reader agreement for cyst growth (kappa = 0.59 for aMRCP and 0.52 for cMRCP). There was no to slight inter-reader agreement for cyst communication with the main pancreatic duct (kappa = 0.17 for aMRCP and kappa = 0.13 for cMRCP).
There was no to slight inter-reader agreement for thickened cyst wall (kappa = 0.17 for aMRCP and 0.03 for cMRCP) and mural nodule (kappa = 0.14 for aMRCP and 0.19 for cMRCP). There was substantial and moderate inter-reader agreement for solid mass separate from the PCL (kappa = 0.74 for aMRCP and 0.59 for cMRCP). There was almost perfect and substantial inter-reader agreement for abrupt duct transition (kappa = 0.84 for aMRCP and kappa = 0.69 for cMRCP). Table 5 summarizes inter-reader agreement for aMRCP and cMRCP.
aMRCP and cMRCP detection of PCL derived malignancy and concomitant pancreatic cancer
For PCL derived malignancy, the sensitivity on aMRCP ranged from 0/6 (0%) to 3/6 (50%), with an overall sensitivity of 4/18 (22%). The sensitivity on cMRCP ranged from 1/6 (17%) to 2/6 (33%), with an overall sensitivity of 4/18 (22%) for all 3 readers. Specificity was 94% for cMRCP and 95% for aMRCP. Figure 2 illustrates an example of PCL derived malignancy that was missed by all 3 readers.
A 74-year-old woman presented for PCL surveillance. a Axial Half-Fourier-Acquired Single-shot Turbo Spin Echo (HASTE), b Axial contrast-enhanced T1 fat-suppressed and c MRI thick slab images demonstrate a 1.9 cm dominant pancreatic head cyst (arrow) without worrisome features or high-risk stigmata by 3 readers, stable from prior MRI. Original radiology report measured two adjacent cysts as a 3.2 cm conglomerate cyst, with the cyst size a worrisome feature. This led to endoscopic ultrasound and fine-needle aspiration which showed atypical cells. Patient underwent Whipple resection. Pathology yielded high-grade dysplasia without invasive component
For concomitant pancreatic cancer, sensitivity on aMRCP ranged from 5/7 (71%) to 7/7 (100%), with an overall sensitivity of 18/21 (86%) amongst all 3 readers. The sensitivity on cMRCP was 100% for all 3 readers. Specificity was 98% at both cMRCP and aMRCP (98%). Figure 3 demonstrates a concomitant pancreatic cancer that was detected by all 3 readers based on abrupt main pancreatic duct caliber change.
64-year-old woman with known concomitant pancreatic cancer. a Axial HASTE and b MRI thick slab images show minimal main pancreatic duct dilation to 4 mm (solid arrow) with abrupt caliber transition at the pancreatic neck, where there was a subsequently biopsy proven 2.5 cm pancreatic ductal adenocarcinoma. Note several small pancreatic cysts (dashed arrows), away from the cancer. All 3 readers found secondary signs of concomitant pancreatic cancer which are main pancreatic duct dilation (ranging from 0.6 to 0.7 cm) and abrupt main pancreatic duct caliber transition on aMRCP and cMRCP. For the dominant concurrent pancreatic cystic lesion away from the mass, 1 reader described a 1 cm dominant cyst in the head, 1 reader described a 1.3 cm cyst in the body, and 1 reader described a 1.4 cm cyst in the tail
Discussion
Our study evaluated intra- and inter-reader agreement between a simulated abbreviated and a comprehensive MRI in risk categorization of PCLs on surveillance MRI and detection of concomitant pancreatic cancer. There was overall strong to almost perfect intra- and inter-reader agreement for cyst size and pancreatic duct caliber amongst all readers and on both cMRCP and aMRCP in our study. This was expected as pancreatic cysts and the main pancreatic duct are most conspicuous on T2-weighted sequences, which are the workhorse sequences radiologists rely upon for measurements, as also recommended by the Society of Abdominal Radiology guidelines [19]. PCLs are typically measured on either axial or coronal T2-weighted sequences (HASTE and MRI), which are available on both cMRCP and aMRCP. This finding is also consistent with prior literature [20, 21].
However, in our study there was no to slight intra- and inter-reader agreement for assessing thickened cyst wall by both aMRCP and cMRCP, which is an important qualitative “worrisome feature” for categorizing a PCL as high-risk. For mural nodule (due to lack of contrast enhanced sequences, mural nodule on aMRCP corresponds with both enhancing and non-enhancing mural nodule for cMRCP), another important high-risk imaging feature, there was no to slight inter-reader agreement at both aMRCP and cMRCP. Interestingly, intra-reader agreement ranged from moderate to almost perfect for mural nodule. The identification of these high-risk imaging features is important, as these PCLs should undergo subsequent endoscopic ultrasound and fine-needle aspiration, or surgery. The lack of intra- and inter-reader agreement for these findings is not unexpected, as these features are highly subjective. The absence of intra- and inter-reader agreement in our study for “thickened cyst wall” is in accordance with a prior study published by Kang et al., who reported this feature having the lowest inter-reader agreement on both aMRCP and cMRCP, with a kappa values of 0.13 and 0.10, respectively [22]. This is probably because there is no standard definition for cyst wall thickening. The Society of Abdominal Radiology IPMN disease focused panel now recommends ≥ 3 mm or anything more than “thin and imperceptible” wall as a threshold for thickened cyst wall [19]. Our study had lower mural nodule detection compared with prior studies, which may stem from the following: First, we had a small cohort of pathologically proven PCL derived malignancy (6 patients), however this more closely reflects the real world experience of PCL surveillance where the incidence of malignancy arising from a PCL is 1.8 to 4.3% at 5 years [3,4,5,6] and therefore very low. Secondly, the majority of our PCL derived malignancy (4/6) harbored only high-grade dysplasia without invasive component. A recent study evaluating diagnostic performance of Fukuoka guideline also found sub-optimal sensitivity for detection of high-grade dysplasia and invasive carcinoma arising from PCL with a sensitivity of 40% in a group of high-risk individuals [23].
Signs of concomitant pancreatic cancer detection include: finding a mass separate from a cyst, abrupt main pancreatic duct caliber transition, and perivascular soft tissue. The finding of duct abrupt transition had the highest intra- and inter-reader agreement (Kappa = 0.83–1, and 0.69–0.8, respectively). This is expected as MRI has superb conspicuity for pancreatic duct visualization, and abrupt pancreatic duct transition/cut-off has been shown to be the most reproducible and specific secondary sign of PDAC [24,25,26]. Sensitivity for concomitant pancreatic cancer detection was slightly higher on cMRCP compared with aMRCP for 2 out of 3 readers, although our sample size was too small to statistically compare these.
Another important feature that lacked inter-reader agreement was duct communication. This is also not surprising as thin MRI sequences are susceptible to motion artifact and duct communication can be difficult to accurately assess on T1- and T2-weighted sequences due to thick slice thickness. It is surprising that cyst morphology (unilocular versus multilocular) also had somewhat low intra- and inter-reader agreement, possibly due to difficulty ascertaining if adjacent small cysts should be considered a conglomerate multi-loculated cyst or separately as several unilocular cysts. This can potentially play a role in diagnosing PCL subtypes and may impact cyst risk stratification based on size (cyst size ≥ 3 cm is a worrisome feature) as illustrated on Fig. 2.
Prior abbreviated MRI research studies are also retrospective in design and extracted a few sequences from the comprehensive MRI [20, 22, 27, 28], with Pozzi-Mucelli et al. using an ultrashort protocol consisting of only axial and coronal HASTE as well as pre-contrast T1 weighted sequences [20]. Macari et al. was the first to investigate this concept, and found that the administration of intravenous contrast would essentially make no difference in 56 patients with cyst follow up recommendation between 2 readers [27]. No pathology was incorporated in this study. Nougaret et al. found similarly low 4.6% disagreement between abbreviated and comprehensive MRI, with the abbreviated protocol overcalling 8 cases that had potential mural nodules that were noted to be not concerning on post contrast sequences. Of their cohort of 301 patients, 32 had cysts that enlarged, 4 developed mural nodules and one developed a mural nodule without cyst size change. These 5 cases with mural nodules were the only ones found to harbor malignancy, and the remainder were presumed to be benign. Both the Macari and Nougaret studies focused on pancreatic cysts but did not assess pancreatic ducts, as both studies were performed before the ACR 2017 White Paper and revised 2017 IAP/Fukuoka guideline [11, 13]. Pozzi-Mucelli et al. was the only study that did not include the MRI sequence. This study focused on comparing cyst size and duct diameter between the standard comprehensive and a simulated ultrashort protocol. Their 154-patient cohort included pre-operative MRI, surveillance MRI and post-operative MRI, with 1 case of BD-IPMN with synchronous PDAC and 1 case of mixed type IPMN with synchronous PDAC. The remaining IPMNs were mostly mixed-type, although there was no mention of associated malignancy [20].
In contrary, Kang et al. followed 123 patients with 156 PCLs and included a large number of pathologically proven malignant lesions (n = 33). This study reported substantial inter-reader agreement on abbreviated MRI for mural nodules, cyst size, and main pancreatic duct dilation. In addition, there was 100% per-lesion and per-patient sensitivity for detecting malignant IPMNs on abbreviated MRI, and specificity of 49.6 and 36.7% [22]. Similar to Nougaret, no malignant cystic lesions were missed by aMRCP, although there were false positive cases. Additionally, Kang et al. included main duct and mixed type IPMNs (n = 52). This group assumed that a cyst with 2-year stability was benign. Similarly, of the 235 patients that Yoo et al. included in their study, 195 were BD-IPMN (83%), and with 40 being (17%) main duct or mixed type IPMN and they used 2-year stability to classify that 85% of their cases were benign [21]. However, it is known that cysts often require much longer than 2 years for malignant transformation, which explains why life-long cyst surveillance is endorsed by the majority of societal consensus guidelines.
Our study differs from these prior studies in that it is predominately comprised of small pancreatic cysts and only 1 mixed type IPMN. The median cyst and duct caliber are 1.4 and 0.3 cm, respectively. Studies have shown that there is a small but real risk of malignancy development from these PCLs, however several new publications have noted that the overall risk is very small for PCLs smaller than 1.5 cm and that long-term surveillance may be excessive and unnecessary [5, 29]. Our study illustrates no to slight intra and inter-reader agreement for an important high-risk feature: thickened cyst wall, with both cMRCP and aMRCP. Similarly, there was no to slight inter-reader agreement for mural nodule with cMRCP and aMRCP, another high-risk imaging feature. However, this finding must be carefully considered in the context of the small number of PCL derived malignancy. In addition, although there was a small sample size of malignant lesions, fewer malignant lesions were identified with abbreviated than comprehensive MRI in our study.
Limitations include that this is a retrospective, single-center study. Additionally, there are a small number of surgically resected malignant IPMNs and concomitant PDACs. However, this reflects the typical daily clinical workflow where most PCLs are of low risk based on radiology assessment. Finally, there is not pathologic proof of benignity for all pancreatic cysts, as this would not occur in clinical practice. To overcome this possibility, we ensured at least 5 years clinical or imaging follow-up for patients included in our study.
In conclusion, there was strong intra- and inter-reader agreement for pancreatic cyst features at aMRCP that relied on T2 weighted sequences such as cyst size, growth, main pancreatic duct caliber and abrupt duct transition. However, both aMRCP and cMRCP had no to slight agreement for important imaging features of cyst wall thickening and mural nodule, with comparable sensitivity for detecting PCL-derived malignancy. cMRCP showed trends towards increased concomitant PDAC detection compared with aMRCP. However, it is important to note the limitations of the study, particularly the small number of PCL-derived malignancy, most of which consisted of high-grade dysplasia without invasive carcinoma, and the small number of PCL concomitant PDAC. Future large-scale and ideally prospective studies are needed to assess whether an abbreviated protocol can be potentially more appropriate for select patients before formal societal recommendations are revised.
References
Kromrey ML, Bülow R, Hübner J, et al. Prospective study on the incidence, prevalence and 5-year pancreatic-related mortality of pancreatic cysts in a population-based study. Gut 2018; 67:138-145
Pergolini I, Sahora K, Ferrone CR, et al. Long-term Risk of Pancreatic Malignancy in Patients With Branch Duct Intraductal Papillary Mucinous Neoplasm in a Referral Center. Gastroenterology 2017; 153:1284-1294.e1281
Moris M, Raimondo M, Woodward TA, et al. International Intraductal Papillary Mucinous Neoplasms Registry: Long-Term Results Based on the New Guidelines. Pancreas 2017; 46:306-310
Oyama H, Tada M, Takagi K, et al. Long-term Risk of Malignancy in Branch-Duct Intraductal Papillary Mucinous Neoplasms. Gastroenterology 2020; 158:226-237.e225
Pergolini I, Sahora K, Ferrone CR, et al. Long-term risk of pancreatic malignancy in patients with branch duct intraductal papillary mucinous neoplasm in a referral center. Gastroenterology 2017; 153:1284-1294. e1281
Yoen H, Kim JH, Lee DH, Ahn SJ, Yoon JH, Han JK. Fate of small pancreatic cysts (<3 cm) after long-term follow-up: analysis of significant radiologic characteristics and proposal of follow-up strategies. Eur Radiol 2017; 27:2591-2599
Ingkakul T, Sadakari Y, Ienaga J, Satoh N, Takahata S, Tanaka M. Predictors of the presence of concomitant invasive ductal carcinoma in intraductal papillary mucinous neoplasm of the pancreas. Ann Surg 2010; 251:70-75
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin 2023; 73:17-48
Corrigendum: recent trends in the incidence and survival of stage 1A pancreatic cancer: a surveillance, epidemiology, and end results analysis. J Natl Cancer Inst 2021; 113:216
Elta GH, Enestvedt BK, Sauer BG, Lennon AM. ACG Clin Guideline: Diagn Manag Pancreat Cysts. 2018; 113:464–479
Megibow AJ, Baker ME, Morgan DE, et al. Management of Incidental Pancreatic Cysts: A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol 2017; 14:911-923
Paiella S, Salvia R, De Pastena M, et al. Screening/surveillance programs for pancreatic cancer in familial high-risk individuals: A systematic review and proportion meta-analysis of screening results. Pancreatology 2018; 18:420-428
Tanaka M, Fernández-del Castillo C, Kamisawa T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology 2017; 17:738-753
Vege SS, Ziring B, Jain R, Moayyedi P, Clinical Guidelines C, American Gastroenterology A. American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology 2015; 148:819-822; quize812-813
Gulani V, Calamante F, Shellock FG, Kanal E, Reeder SB. Gadolinium deposition in the brain: summary of evidence and recommendations. Lancet Neurol 2017; 16:564-570
Tanaka M. Intraductal Papillary Mucinous Neoplasm of the Pancreas as the Main Focus for Early Detection of Pancreatic Adenocarcinoma. Pancreas 2018; 47:544-550
Yamaguchi K, Kanemitsu S, Hatori T, et al. Pancreatic ductal adenocarcinoma derived from IPMN and pancreatic ductal adenocarcinoma concomitant with IPMN. Pancreas 2011; 40:571-580
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 2012; 22:276-282
Hecht EM, Khatri G, Morgan D, et al. Intraductal papillary mucinous neoplasm (IPMN) of the pancreas: recommendations for Standardized Imaging and Reporting from the Society of Abdominal Radiology IPMN disease focused panel. Abdominal radiology (New York) 2020; 46:1586-1606
Pozzi-Mucelli RM, Rinta-Kiikka I, Wünsche K, et al. Pancreatic MRI for the surveillance of cystic neoplasms: comparison of a short with a comprehensive imaging protocol. Eur Radiol 2017; 27:41-50
Yoo J, Min JH, Lee DH, Hur BY, Kim SW, Kim E. Abbreviated Magnetic Resonance Imaging With Breath-Hold Three-Dimensional Magnetic Resonance Cholangiopancreatography: Assessment of Malignant Risk of Pancreatic Intraductal Papillary Mucinous Neoplasm. J Magn Reson Imaging 2021; 54:1177-1186
Kang HJ, Lee DH, Lee JM, et al. Clinical Feasibility of Abbreviated Magnetic Resonance With Breath-Hold 3-Dimensional Magnetic Resonance Cholangiopancreatography for Surveillance of Pancreatic Intraductal Papillary Mucinous Neoplasm. Investigative radiology 2020; 55:262-269
Dbouk M, Brewer Gutierrez OI, Lennon AM, et al. Guidelines on management of pancreatic cysts detected in high-risk individuals: An evaluation of the 2017 Fukuoka guidelines and the 2020 International Cancer of the Pancreas Screening (CAPS) consortium statements. Pancreatology 2021;
Johnston A, Serhal A, Lopes Vendrami C, et al. The abrupt pancreatic duct cutoff sign on MDCT and MRI. Abdominal radiology (New York) 2020; 45:2476-2484
Tanaka S, Nakao M, Ioka T, et al. Slight Dilatation of the Main Pancreatic Duct and Presence of Pancreatic Cysts as Predictive Signs of Pancreatic Cancer: A Prospective Study. 2010; 254:965-972
Toshima F, Watanabe R, Inoue D, et al. CT Abnormalities of the Pancreas Associated With the Subsequent Diagnosis of Clinical Stage I Pancreatic Ductal Adenocarcinoma More Than One Year Later: A Case-Control Study. AJR Am J Roentgenol 2021; 217:1353-1364
Macari M, Lee T, Kim S, et al. Is gadolinium necessary for MRI follow-up evaluation of cystic lesions in the pancreas? Preliminary results. AJR Am J Roentgenol 2009; 192:159-164
Nougaret S, Reinhold C, Chong J, et al. Incidental pancreatic cysts: natural history and diagnostic accuracy of a limited serial pancreatic cyst MRI protocol. Eur Radiol 2014; 24:1020-1029
Marchegiani G, Pollini T, Burelli A, et al. Surveillance for Presumed BD-IPMN of the Pancreas: Stability, Size, and Age Identify Targets for Discontinuation. Gastroenterology 2023; 165:1016-1024.e1015
Funding
None.
Author information
Authors and Affiliations
Contributions
Bari Dane, MD: Speaker Honorarium from Siemens Healthineers for educational content unrelated to this manuscript. Chenchan Huang, Paul Smereka, Abhinav Vij, Vinay Prabhu, Rebecca Anthopolos, Cristina H. Hajdu, None.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, C., Prabhu, V., Smereka, P. et al. Comparison of intra- and inter-reader agreement of abbreviated versus comprehensive MRCP for pancreatic cyst surveillance. Abdom Radiol 49, 3517–3527 (2024). https://doi.org/10.1007/s00261-024-04449-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-024-04449-8