Abstract
Purpose
To determine the frequency, imaging, and clinical manifestations of immune checkpoint inhibitor (ICI)-related colitis in cancer patients on monotherapy or combination therapy.
Methods
The electronic medical records of 1044 cancer patients who received ICIs were retrospectively reviewed to identify 48 patients who had a clinical diagnosis of immune-related colitis. Imaging studies were reviewed to identify patients with imaging manifestations of colitis. Demographic data, type of ICIs, symptoms, presence of other immune-related adverse events (irAEs), and management were recorded.
Results
There was imaging evidence of immune-related colitis in 34 patients (24 men; median age: 63.5 years). The median time to onset of colitis was 75 days (IQR 25–75, 49.5–216 days) in patients receiving monotherapy (group 1) and 78 days (IQR 25–75, 44.3–99.5 days) in patients undergoing combination therapy (group 2) following start of ICI. Symptoms included diarrhea (91.1% [31 of 34]), nausea/vomiting (52.9% [18 of 34]), and abdominal pain (52.9% [18 of 34]). The most common imaging findings were bowel wall thickening (97% [33 of 34]) and fluid-filled colon (82.3% [28 of 34]). Colitis was diffuse in 21 of 34 (61.8%) patients. Imaging manifestations did not differ between the two groups (p > 0.05). Steroids and antibiotics were used to treat colitis in 29 of 34 (85.2%) and 13 of 34 (38.2%) patients, respectively. No patients in group 1 experienced concurrent irAEs, but 5 of 18 (27.8%) of patients in group 2 had other irAEs (p = 0.046).
Conclusion
Immune-related colitis occurred in 3.3% of patients receiving ICIs with bowel wall thickening, fluid-filled colon and pancolitis being the most common imaging manifestations. Imaging manifestations did not differ between patients receiving monotherapy or combination therapy. However, concurrent irAEs were significantly observed in patients undergoing combination therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Immune checkpoint inhibitors (ICIs) are used to treat cancer by effectively stimulating the immune system to attack cancer cells. Ipilimumab is a recombinant human monoclonal antibody that binds to the cytotoxic T-lymphocyte associated antigen 4 (CTLA-4), which is a down-regulator of T-cell activation pathways. It was approved by the United States Federal Drug Administration (FDA) in 2011 for treatment of late-stage metastatic melanoma [1]. In the following years, other immunotherapy agents, such as nivolumab and pembrolizumab, have been developed. Nivolumab is a fully human monoclonal antibody that binds to the programmed cell death-1 (PD-1) receptor and selectively inhibits PD-1 activity. The binding of PD-1 ligand 1 or ligand 2 (PD-L1 or PD-L2) renders the T-cell inactive. Nivolumab blocks ligand binding to PD-1 and allows for T-cell activation and proliferation. It is used as first line for metastatic melanoma in combination with ipilimumab. Ipilimumab and nivolumab in combination have a significantly higher response rate, progression-free survival, and overall survival than ipilimumab therapy alone for metastatic melanoma [2]. Pembrolizumab, similarly, is a selective anti-PD-1 humanized monoclonal antibody, used in the treatment of metastatic melanoma, metastatic non-small cell lung cancer (NSCLC), and head and neck squamous cell carcinoma (HNSCC).
These agents are associated with a wide range of side effects, referred to as immune-related adverse events (irAE), which include uveitis, rash, hypophysitis, pneumonitis, hepatitis, pancreatitis, and colitis, among others. Colitis is one of the most common irAEs, with some cases being fatal. Therefore, early identification and prompt treatment of immune-related colitis is extremely important. Currently, colonoscopy and biopsy of colonic mucosa is the gold standard for diagnosis of immune-related colitis. However, less invasive measures, notably computed tomography (CT), can be used to detect and monitor colitis and other irAEs.
The purpose of this study is to determine the frequency, clinical and imaging manifestations of immune-related colitis in cancer patients on monotherapy or combination ICI therapy.
Materials and methods
Patients and clinical findings
A retrospective database search between January 2010 and November 2018 was performed in 1044 patients treated with ICIs to identify cases who subsequently developed immune-related colitis. Inclusion criteria were as follows: 1-adult patients (age > 18 years) who were treated with ICIs for various cancers as part of the standard clinical care and developed clinical signs and symptoms of colitis, based on the common terminology criteria for adverse events (CTCAE), 2-patients who had at least one cross-sectional imaging study performed at the time of presentation and had radiologic evidence of colitis.
The demographics and clinical manifestations of the patients were obtained by review of medical records. Primary cancer types of the patients, administration of single or multiple ICIs, the start and end dates of immunotherapies were recorded. Imaging studies were retrospectively evaluated.
Cases with radiographically evident colitis were subsequently correlated with clinical, laboratory, histopathologic data, colonoscopy reports and stool analysis to exclude conditions that might mimic immune-related colitis including infectious and neutropenic colitis.
This study was approved by the institutional review board with waiver for informed consent and was in compliance with the Health Insurance Portability and Accountability Act.
Cross-sectional imaging analysis and imaging features
Due to the retrospective nature of the study, the imaging parameters and protocols varied among patients. CT scans of the abdomen and pelvis were obtained on multidetector scanners with 120 kVp and a tube current maximum of 500 mA with intravenous contrast agent unless patients had a renal impairment or iodine allergy. No oral contrast agent was given to the patients. Multiplanar reformatted images were reviewed on Picture Archiving Communication System (PACS; Sectra, Sweden).
Imaging features that were evaluated for immune-related colitis included bowel wall thickening (bowel wall thickening was categorized as mild [3–5 mm], moderate [5–7 mm], severe [> 7 mm]); enhancement pattern (homogeneous, mucosal, layered); lumen contents (fluid, feces, blood, and fat); mesenteric change (stranding, edema, fluid); mesenteric vessel engorgement; free air, and pneumatosis coli [3,4,5]. Involvement of length was assessed according to the involved colonic segments. Colon was divided into four segments and based on that called focal (< 1 segment), segmental (1–3 segments), and diffuse (entire colon). Segmental colitis associated with diverticulosis (SCAD) restricted to a segment of colon with diverticulosis was also searched [3, 5, 6].
The images were reviewed by two board-certified radiologists in consensus (S.H.T and N.H.R, with 12 and 21 years of experience). The radiologists were aware that the patients were treated with ICIs for various cancers but did not have access to other clinical details. For each imaging study, a score of 1–5 was assigned based on radiographic features corresponding to colitis: 1, definitely not colitis; 2, probably not colitis; 3, equivocal; 4, probable colitis; and 5, definite colitis. Patients who had imaging that scored ≥ 3 were considered positive. For each positive case, specific imaging criteria were described. The date of the scan was recorded to represent the onset of radiographically evident immune-related colitis.
The response of the underlying malignancy to the ICI therapy at the time of the detection of immune-related colitis was recorded as per the immune Response Evaluation Criteria in Solid Tumors (iRECIST).
Statistical analysis
Descriptive statistics were obtained for the demographic and clinical characteristics of cases. Differences in demographics, imaging findings, and clinical characteristics were compared between patients with radiographically evident immune-related colitis who received single agent and multiple agent, using the Fisher’s exact test for categorical variables. All p values were based on a two-sided hypothesis. A p value of < 0.05 was considered to be statistically significant. All statistical analyses were conducted using JMP® Software (JMP®, Version 13.0.0 SAS Institute Inc., Cary, NC, 1989–2007).
Results
Among the 1044 patients who were treated with ICIs, 48 (4.6%) were identified to have clinical symptoms of colitis. 4 patients who did not have available cross-sectional imaging at the episode of colitis were excluded. Of the remaining 44 patients, 34 (3.3%) (24 men, 10 women; mean age: 63.5 years) who had imaging scores of ≥ 3 and confirmation of clinical findings were considered to have radiologic immune-related colitis.
Clinical findings
The breakdown of the specific agents used in single agent and combination therapy as well as the types of cancer treated is provided in Table 1. There were 16 (47%) patients who received single agent therapy (group 1) and 18 (52.9%) who received combination therapy (group 2).
Clinical manifestations of patients treated with monotherapy and combination therapy are described in Table 2. The median number of days from start of the ICI to presentation of colitis symptoms were 75 days (IQR 25–75, 49.5–216 days) in group 1 and 78 days (IQR 25–75, 44.3–99.5 days) in group 2. Clinical symptoms included diarrhea (91.1% [31 of 34]), nausea/vomiting (52.9% [18 of 34]) and abdominal pain (52.9% [18 of 34]). None of the patients had fever but white blood cell count (WBC) was elevated in 7 of 34 (20.6%) patients. The median WBC count of patients with elevated levels was 15.3 × 109/L (range 11.4 × 109/L–38.3 × 109/L). Stool analysis was performed in 27 of 34 (79.4%) patients with negative result in all patients. 14.7% [5 of 34] of patients had a corresponding colonoscopy that confirmed colitis.
Within the group 1, 13 of 16 (81%) patients received steroid treatment for their colitis, and 6 of 16 (37%) received antibiotics. In the group 2, 16 of 18 (89%) patients received steroids and 7 of 18 (39%) received antibiotics. All patients except for one had reported improvement in their colitis symptoms after receiving either or both forms of treatment.
Imaging findings
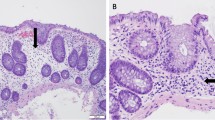
Table 3 details imaging features of patients. With regards to imaging features, bowel wall thickening (97% [33 of 34]), and fluid-filled colon (82.3% [28 of 34]) were the most common findings in both sets of patients (Figs. 1, 2). 10 of 16 (62.5%) patients who received single agent and 11 of 18 (61.1%) patients who had a combination therapy showed diffuse colitis. 2 of 18 (11%) patients on combination therapy had SCAD. 7 of 16 patients (43.7%) and 9 of 18 patients (50%) demonstrated mucosal enhancement pattern. Average colitis scores based on the imaging were 4.4 and 4.8 for group 1 and group 2, respectively. Imaging findings did not differ between group 1 and group 2 (p > 0.05). Only 37.5% and 50% of radiology reports in the monotherapy and combination therapy groups, respectively, specifically called out “colitis” in the read.
47-year-old man with melanoma presenting with diarrhea. Axial contrast-enhanced CT images performed 35 days after initiation of ipilimumab shows bowel wall thickening in transverse colon (a) and ascending colon (b) with layered enhancement pattern and fat stranding. Coronal-reformatted contrast-enhanced CT image (c) demonstrates bowel wall thickening and layered enhancement of cecum and descending colon with mesenteric vessel engorgement. Coronal-reformatted contrast-enhanced CT image (d) shows fluid-filled rectum with bowel wall thickening. Findings are consistent with diffuse colitis
40-year-old woman with melanoma presenting with diarrhea and high WBC count (18.8 × 109/L). Coronal-reformatted contrast-enhanced CT image performed 45 days after initiation of ipilimumab and nivolumab shows fluid-filled bowel segments with thickened walls and mucosal hyperenhancement. The findings are consistent with diffuse colitis. The patient received steroid therapy and the symptoms resolved
There was a statistically significant difference between the two groups in terms of development of additional irAEs (p = 0.046). No patients in the single agent group experienced concurrent irAEs, but 5 of 18 (27.8%) patients undergoing combination therapy had documented irAEs. These irAEs included perineal abscess (nivolumab and ipilimumab), hepatitis (ipilimumab and pembrolizumab), pancreatitis and hepatitis (same patient both developed pancreatitis and hepatitis while treated with ipilimumab and pembrolizumab), thyroiditis (nivolumab and ipilumumab), and dermatitis (nivolumab and ipilumumab).
At the time of the diagnosis of immune-related colitis, 15 of 34 (44%) patients had stable disease and 8 of 34 (23%) patients had partial response, while 8 of 34 (23%) patients had progressive disease according to the iRECIST (Fig. 3). Complete response was observed in 1 of 34 (3%) patients. Response of the underlying disease to ICI therapy was not evaluable in 2 of 34 (6%) patients.
60-year-old man with melanoma presenting with diarrhea. Axial contrast-enhanced CT image a shows a metastasis adjacent to the splenic flexure (arrow). Coronal-reformatted contrast-enhanced CT image b obtained at the same time demonstrates no signs of colitis. Axial contrast-enhanced CT performed 32 days after initiation of ipilimumab and nivolumab c shows regression of the metastasis (arrow). Coronal-reformatted contrast-enhanced CT image d demonstrates fluid-filled ascending and descending colon. Findings are consistent with immune-related colitis
Discussion
Immune-related colitis is an established complication in patients treated with ICIs, with potentially life-threatening outcomes [7, 8]. It has been described as the most common ICI-related gastrointestinal toxicity [4, 9, 10]. In patients treated with anti-CTLA-4 and PD-1 pathway inhibitors for various cancers such as melanoma, efficient and accurate diagnosis of colitis is necessary in order for patients to receive treatment [11]. Although colonoscopy and biopsy is often regarded as the gold standard for diagnosis, use of noninvasive measures can maximize patient safety and benefit. Beyond identification of clinical features, radiological features must also be taken into consideration when assessing for the presence and severity of colitis [12]. Garcia-Neuer et al. investigated CT and demonstrated it to be a reliable and noninvasive mode of diagnosing colitis in ipilimumab-treated advanced melanoma patients. They also found that CT is highly predictive of colitis on colonoscopy and biopsy, and therefore colonoscopy and biopsy may not be necessary to establish colitis [13].
Radiographically evident immune-related colitis was observed in 3.3% of patients treated with ICIs in our study. A meta-analysis that evaluated the incidence of ICI-related colitis in solid tumor patients reported the overall incidence during ipilimumab monotherapy was 9.1% for all-grade colitis whereas it was 1.3% during PD-1/PD-L1 inhibitor monotherapy [14]. The relatively lower incidence in our study might be due to the evaluation of immune-related colitis in the whole group of patients undergoing ICIs. Additionally, the inclusion criterion of patients having both clinical and radiologic findings of immune-related colitis might have led to the lower incidence.
All patients included in our study had evidence of colitis based on imaging. However, when the reports were retrospectively reviewed, less than half of the CT scan reads reported colitis, even though characteristic imaging features existed. This reveals a need for increased awareness among radiologists of abdominal irAEs. Association of common features such as a fluid-filled colon, bowel wall thickening, mesenteric vessel engorgement, fat stranding, free fluid, and less commonly free air and pneumatosis with colitis with a diagnosis of colitis must be recognized. Importantly, knowledge that the patient is undergoing cancer treatment with ICIs and experiencing symptoms such as fever and diarrhea is significant in providing valuable clinical context in guiding radiologists to include the differential of colitis in their reports. Understanding the temporal presentation of colitis in relation to ICI therapy can be useful.
Patients in our study experienced colitis and were diagnosed within a median of 2 to 3 months of the initiation of treatment, consistent with reports from other published data [3, 15, 16]. No difference in this timeframe was appreciated between monotherapy and combination therapy groups (p = 1). Almost all patients in both groups received treatment for colitis in the form of steroids and/or antibiotics, with 4 also receiving infliximab, with symptomatic improvement in their colitis, demonstrating that prompt identification and proper treatment of colitis can help avoid adverse outcomes, as colitis can be fatal.
Studies have demonstrated that patients receiving combination ICI therapy are more likely to have a gastrointestinal event compared with monotherapy patients [17,18,19]. In our study, there were 16 patients with immune-related colitis on single agent ICI and 18 patients on combination therapy. There have been a few studies in the literature describing radiologic findings of ICI-related colitis, but to our knowledge, none that compare the prevalence of imaging findings of colitis in patients that are undergoing single agent with those receiving combination therapy. Our study showed that there are no significant difference in terms of imaging features of colitis between the 2 groups.
Prior research has also found that the risk of all irAEs, not just colitis, is increased with ipilimumab and nivolumab combination therapy [20]. Likewise, in our study, a greater proportion of patients in the combination therapy group experienced other irAEs in addition to colitis, encompassing perineal abscess, hepatitis, thyroiditis, hypophysitis, and dermatitis. No patients in the single agent group had findings of other irAEs. Clinicians should take care to exclude other irAEs in patients presenting with immune-related-colitis, especially those on combination therapy.
Our study has several limitations including its retrospective design and heterogeneous study population of patients treated with various ICIs in a single institution. Although in our study, the diagnosis of immune-related colitis was based on clinical and radiologic findings, it is difficult to define the absolute gold standard for the diagnosis of irAEs. The diagnosis often requires multidisciplinary interactions among oncologists, radiologists, and pathologists. Therefore, sensitivity and specificity of radiological diagnosis of immune-related colitis were not performed.
In conclusion, immune-related colitis occurred in 3.3% of patients receiving ICIs with bowel wall thickening, fluid-filled colon and pancolitis being the most common imaging manifestations. Imaging manifestations did not differ between patients receiving monotherapy or combination therapy. However, concurrent irAEs were significantly observed in patients undergoing combination therapy. Immune-related colitis is often radiographically evident based on established imaging features, but is not always called in the report probably due to lack of awareness among radiologists.
References
Press Announcements > FDA approves new treatment for a type of late-stage skin cancer. https://web.archive.org/web/20110327063147/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm1193237.htm. Published March 27, 2011. Accessed June 2, 2019.
Wolchok JD, Chiarion-Sileni V, Gonzalez R, et al (2017) Overall Survival with Combined Nivolumab and Ipilimumab in Advanced Melanoma. N Engl J Med 377:1345-1356.
Tirumani SH, Ramaiya NH, Keraliya A, Bailey ND, Ott PA, Hodi FS, Nishino M (2015) Radiographic Profiling of Immune-related Adverse Events in Advanced Melanoma Patients Treated With Ipilimumab. Cancer Immunol Res 3:1185-1192.
Puzanov I, Diab A, Abdallah K, et al (2017) Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J Immunother Cancer 5:95.
Kim KW, Ramaiya NH, Krajewski KM, Shinagare AB, Howard SA, Jagannathan JP, Ibrahim N (2013) Ipilimumab-associated colitis: CT findings. AJR Am J Roentgenol 200:W468-474.
Mekki A, Dercle L, Lichtenstein P, et al (2018) Detection of immune-related adverse events by medical imaging in patients treated with anti-programmed cell death 1. Eur J Cancer 96:91-104.
Beck KE, Blansfield JA, Tran KQ, et al (2006) Enterocolitis in patients with cancer after antibody blockade of cytotoxic T-lymphocyte-associated antigen 4. J Clin Oncol 24:2283-2289.
Weber J, Thompson JA, Hamid O, et al (2009) A randomized, double-blind, placebo-controlled, phase II study comparing the tolerability and efficacy of ipilimumab administered with or without prophylactic budesonide in patients with unresectable stage III or IV melanoma. Clin Cancer Res 15:5591-5598.
Haanen JBAG, Carbonnel F, Robert C, Kerr KM, Peters S, Larkin J, Jordan K; ESMO Guidelines Committee (2017) Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow up. Ann Oncol 28(suppl 4):iv119-iv142.
Sosa A, Cadena EL, Olive CS, Karachaliou N, Rosell R (2018) Clinical assessment of immune-related adverse events. Ther Adv Med Oncol 10:1758835918764628.
Friedman CF, Proverbs-Singh TA, Postow MA (2016) Treatment of the Immune-Related Adverse Effects of Immune Checkpoint Inhibitors: A Review. JAMA Oncol 2:1346-1353.
Gupta A, De Felice KM, Loftus EV Jr, Khanna S (2015) Systematic review: colitis associated with anti-CTLA-4 therapy. Aliment Pharmacol Ther 42:406-417.
Garcia-Neuer M, Marmarelis ME, Jangi SR, et al (2017) Diagnostic Comparison of CT Scans and Colonoscopy for Immune-Related Colitis in Ipilimumab-Treated Advanced Melanoma Patients. Cancer Immunol Res 5:286-291.
Wang DY, Ye F, Zhao S, Johnson DB (2017) Incidence of immune checkpoint inhibitor-related colitis in solid tumor patients: A systematic review and meta-analysis. Oncoimmunology 6:e1344805.
Horn L, Spigel DR, Vokes EE, et al (2017) Nivolumab Versus Docetaxel in Previously Treated Patients With Advanced Non-Small- Cell Lung Cancer: Two-Year Outcomes From Two Randomized, Open-Label, Phase III Trials (CheckMate 017 and CheckMate 057). J Clin Oncol 35:3924-3933.
Alessandrino F, Sahu S, Nishino M, et al (2019) Frequency and imaging features of abdominal immune-related adverse events in metastatic lung cancer patients treated with PD-1 inhibitor. Abdom Radiol (NY) 44:1917-1927.
Larkin J, Hodi FS, Wolchok JD (2015) Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N. Engl. J. Med 373:1270-1271.
Irwin DE, Davis B, Bell JA, Galaznik A, Garcia-Ribas I (2018) Gastrointestinal complications in patients treated with ipilimumab and nivolumab combination therapy or monotherapy. J Comp Eff Res 8:81-90.
Reddy HG, Schneider BJ, Tai AW (2018) Immune Checkpoint Inhibitor-Associated Colitis and Hepatitis. Clin Transl Gastroenterol 9:180.
Zhou S, Khanal S, Zhang H (2019) Risk of immune-related adverse events associated with ipilimumab-plus-nivolumab and nivolumab therapy in cancer patients. Ther Clin Risk Manag 15:211-221.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shieh, A.C., Guler, E., Pfau, D. et al. Imaging and clinical manifestations of immune checkpoint inhibitor-related colitis in cancer patients treated with monotherapy or combination therapy. Abdom Radiol 45, 3028–3035 (2020). https://doi.org/10.1007/s00261-019-02334-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02334-3