Abstract
Imaging of the scrotum in the setting of acute symptoms such as pain or swelling is commonly performed emergently to differentiate between patients who require immediate surgery and those that do not. Acute scrotal symptoms are generally caused by infectious, traumatic or vascular etiologies. Rapid diagnosis and initiation of treatment is vital for testicular salvage in cases of acute testicular torsion, testicular rupture, and Fournier gangrene. Epididymitis, epididymo-orchitis, torsed testicular appendage, segmental testicular infarction, scrotal hematomas, testicular neoplasms, and acute idiopathic scrotal edema can have similar clinical presentations, but these conditions do not require immediate surgery. Ultrasound is the well-established first-line imaging modality for the acute scrotum. Contrast-enhanced ultrasound and magnetic resonance imaging can be useful as problem-solving tools when ultrasound studies are inconclusive or equivocal. This review describes normal scrotal anatomy and a wide range acute scrotal disorders, with emphasis on the imaging and clinical features that can minimize the risk of misdiagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Imaging of acute-onset scrotal swelling with or without pain is performed emergently to establish a diagnosis and to differentiate between patients who need immediate surgical exploration and those who do not. Rapid diagnosis and initiation of treatment are vital for testicular salvage in cases of testicular rupture and ischemia, as testicular viability is directly related to the duration of ischemia [1].
Ultrasound is the established first-line imaging modality for acute scrotal disease [2, 3]. When combined with clinical history and physical examination, ultrasound results can be used to diagnose most scrotal disorders. For equivocal cases that do not require immediate surgical intervention, magnetic resonance imaging (MRI) can be used to help further characterize scrotal pathology. Patients who are evaluated for testicular torsion or ischemia and have equivocal ultrasound findings, however, are often taken for surgical exploration. Contrast-enhanced ultrasound (CEUS) better depicts tissue perfusion as compared to conventional ultrasound and can provide a rapid, non-nephrotoxic, nonionizing, bedside imaging adjunct when ultrasound findings are inconclusive. CEUS can be used for the definitive diagnosis of infarction, assessment of viable parenchyma after trauma, and differentiation of tumor neovascularity, potentially reducing the need for further imaging [4].
The causes of acute scrotal disease are generally divided into infectious, vascular, and traumatic categories. The most common causes of acute scrotal disease include spermatic cord torsion, torsion of the testicular appendages, and acute epididymitis or epididymo-orchitis. Other diagnoses that present acutely are segmental testicular infarction, Fournier gangrene, and acute idiopathic scrotal edema. In cases where testicular trauma has occurred, assessment for testicular hematoma, fracture, and rupture should be performed. Testicular neoplasms do not typically present acutely but can be incidentally discovered in up to 10% to 15% of patients with scrotal trauma [5]. Intratesticular hematoma, focal infection, and segmental testicular infarction can mimic tumors on imaging.
In this review, we first consider normal scrotal anatomy, focusing on the sonographic appearance of structures pertinent to acute scrotal pathology. We then discuss acute scrotal disorders of infectious, vascular, traumatic, and miscellaneous etiologies with an emphasis on clinical features and key imaging findings pertinent to establishing a diagnosis.
Scrotal anatomy
The scrotum consists of a thin fibromuscular cutaneous external sac that is divided by a septum to house each of the two testicles. It is formed from the fusion of the labioscrotal folds and its layers are a continuation of the abdominal wall. From superficial to deep, the layers include skin, dartos fascia, external spermatic fascia, cremasteric muscle, internal spermatic fascia, and tunica vaginalis. The testis, epididymis, and spermatic cord are contained within the scrotum. The tunica vaginalis has two layers: the outer parietal layer lines the internal spermatic fascia of the scrotal wall, and the inner visceral layer partially surrounds the testicle and epididymis. A potential space between the tunica vaginalis layers normally contains a few milliliters of fluid but can be filled with fluid (hydrocele), blood (hematocele), or pus (pyocele) in cases of disease [6]. The testes have relatively free movement in the scrotal sac, with the gubernaculum (also known as the scrotal ligament) tethering the testis to the inferior scrotum to prevent torsion. A tough fibrous capsule called the tunica albuginea envelops each testis and invaginates to form the mediastinum testis. Developing sperm travel through multiple testicular seminiferous tubules to a central convergence at the rete testis in the mediastinum to enter the efferent ductules and epididymal head. The epididymis is divided into a head, body, and tail and is attached to the upper testes at the head. The majority of the blood and nerve supply for the epididymis and testis travel within the spermatic cord, a connective tissue cord-like structure that runs from the deep inguinal ring into the scrotum posteriorly. The spermatic cord contains three arteries, three veins, lymphatics, and two nerves (Fig. 1).
The testicle is enveloped by a fibrous capsule called the tunica albuginea, which projects into the testis to form the mediastinum testis. The tunica vaginalis is a two-layered membrane that covers the tunica albuginea. Multiple testicular seminiferous tubules run toward the mediastinum and coalesce into a network of channels called the rete testis. These channels pass through the mediastinum and tunica albuginea to form the epididymal head, body, and tail ducts, which continue as the vas deferens. The spermatic cord contains the vas deferens, testicular vessels, pampiniform venous plexus, and nerves
Ultrasound technique
Scrotal ultrasound is performed with the patient lying supine and a towel placed under the scrotum for elevation and support. A second towel is used to cover and retract the penis off the scrotum. Optimal scanning is performed using a linear high-frequency (> 7 MHz) transducer with broad bandwidth (6–12 MHz or higher). The equipment should be capable of performing color, power, and spectral Doppler scans [7].
Grayscale images of the testes and epididymides are obtained in transverse and sagittal planes. Testicular size is measured in three dimensions (length, width, height). Color and spectral Doppler imaging through each epididymis and testicle is essential for the assessment of blood flow. Doppler settings should be optimized to maximize detection of low-velocity flow. Color Doppler gain should be adjusted to eliminate artifacts. When set correctly, vascular flow should be easily identifiable within the testis and surrounding tissues. Power Doppler imaging has a higher sensitivity for detecting slow blood flow than color Doppler imaging and can therefore be used as a supplemental tool to distinguish between absent flow and slow flow. Transverse grayscale and color Doppler images including both testicles are also obtained to aid in side-to-side comparison [7].
Grayscale images of the scrotal skin and soft tissues surrounding the testes are obtained to assess for fluid collections, edema, and overall symmetry. Cine clips are helpful to better depict three-dimensionality and relationships between structures. Dedicated images of the spermatic cord from the external inguinal ring along its complete course through the scrotum should be obtained when testicular torsion is suspected [8]. The veins of the pampiniform plexus are evaluated for size and with augmentation through Valsalva or upright positioning.
Scrotal anatomy on ultrasound images
The scrotal wall contains several layers of muscle and fascia that cannot be discerned by ultrasound, contributing to its heterogeneous echogenic appearance. Scrotal wall thickness ranges from 2 to 8 mm depending on cremasteric muscle contraction [6]. The normal adult testicle is oval and measures approximately 5 × 3 × 2 cm, with a homogeneous echotexture and diffuse intermediate level echogenicity [6, 9]. The tunica albuginea appears as a thin hyperechoic rim encasing the testicle, which invaginates in the central testicle as a hyperechoic band corresponding to the mediastinum testis. The tunica vaginalis can be identified as a thin hyperechoic line, but this structure is not routinely visualized in the absence of hydrocele. The epididymis is best visualized on longitudinal views and appears isoechoic to slightly hypoechoic relative to the adjacent testis. The epididymal head measures 5 to 12 mm in maximum length; the body and tail measure 2 to 5 mm in diameter [6]. The spermatic cord has a straight course from the external inguinal ring along the posterior border of the testicle, with a normal transverse diameter of less than 5 mm (Fig. 2) [6, 9].
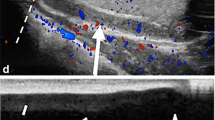
a Sagittal grayscale image shows a normal testicle with homogeneous echotexture. The scrotal wall contains several layers of muscle and fascia, which cannot be discerned by ultrasound, contributing to its heterogeneous echogenic appearance. The thin hyperechoic line surrounding the testicle is the tunica albuginea. The epididymis is slightly hypoechoic compared to the testicular parenchyma. b Sagittal grayscale image shows a linear hyperechoic line representing the mediastinum testis. c Sagittal image with color and spectral Doppler shows normal testicular perfusion throughout the testicle and a normal arterial spectral waveform. d Transverse image with color Doppler including both testicles shows symmetrical flow
Infectious etiologies of the acute scrotum
Epididymitis and epididymo-orchitis
Infection is the most common cause of acute scrotal pain and can involve the epididymis (epididymitis), testicle (orchitis), or both (epididymo-orchitis). Infection spreads through the urogenital tract in a retrograde fashion, from tail to head through the epididymis and only afterwards to the testicle. A full evaluation of the epididymis is essential in these cases, as early infection may be limited to the tail. Epididymitis with orchitis occurs in approximately 20% to 40% of cases [6]. Isolated cases of orchitis can be caused by viral infection and are most commonly associated with mumps; however, such cases are rare in the developed world because of widespread vaccination. For sexually active men younger than 35 years, Chlamydia trachomatis and Neisseria gonorrhea are the most common pathogens of epididymitis and epididymo-orchitis. In children and men older than 35 years, urinary tract-contaminating organisms such as Escherichia coli and Pseudomonas species are the more likely pathogens [10].
Ultrasound findings in patients with epididymitis include an enlarged and hypoechoic epididymis due to edema. Reactive hydroceles and scrotal wall thickening are secondary findings. Color Doppler imaging shows increased blood flow corresponding to hyperemia, which is the key criterion for the diagnosis of epididymitis (Fig. 3) [11]. Importantly, a normal epididymis exhibits blood flow on color Doppler images; thus, the mere detection of some flow does not necessarily imply the presence of an infection [12]. When the infection has spread to include the testicle, the testicular parenchyma also develops heterogeneous echogenicity with increased blood flow on color Doppler images (Fig. 4). Physical examination techniques such as Prehn’s sign (in which scrotal elevation above the pubic bone improves pain caused by epididymitis or epididymo-orchitis) have been shown to be inferior to color Doppler imaging in differentiating between infection and testicular torsion [13]. Additionally, urinalysis results will be abnormal in patients with infectious etiologies but normal in patients with testicular torsion. Ultrasound features, when combined with clinical history, physical examination, and laboratory data, can therefore help clinicians to make the correct diagnosis.
57-Year-old man with scrotal swelling and tenderness that began the night before presentation. a Transverse grayscale image shows the right epididymis is enlarged with heterogeneous echogenicity (arrows). b Color Doppler image at the same location shows increased vascular flow throughout the epididymis. c Side-by-side images of the right and left epididymal heads clearly depict right-sided hyperemia
53-Year-old man with scrotal swelling and tenderness after renal transplant. a Sagittal grayscale image shows mildly heterogeneous echotexture of both the left epididymal head (asterisk) and testicle (diamond). b and c Side-by-side comparison views with color Doppler of the right and left epididymal heads (b) and testes (c) show increased vascular flow in the left epididymis and testicle compared to the right
When left untreated, epididymitis and epididymo-orchitis can result in complications such as abscess formation, pyocele, and testicular ischemia (Fig. 5). An abscess appears as a focal, complex fluid collection with no internal vascularity and peripheral hyperemia. Pyocele refers to the collection of pus between the layers of the tunica vaginalis; this collection is complex on ultrasound images, often containing debris and septa. Testicular ischemia can occur when epididymal edema compresses the spermatic cord, restricting flow through the testicular vessels [14].
50-Year-old man with scrotal swelling and pain for 1 month that had acutely worsened over the previous 3 days. a Sagittal image with power Doppler shows a complex collection within an enlarged left epididymal head (asterisk). The collection contains internal septa and echogenic debris and surrounding hyperemia (arrow). Complex fluid with internal echoes surrounds the epididymis (arrowheads). b Sagittal grayscale image shows a complex, septated collection within the posterior scrotal wall (asterisk). Emergent surgical incision and drainage confirmed the presence of epididymal and scrotal wall abscesses with pyocele
BCG-related epididymitis
Originally developed from Mycobacterium bovis, bacillus Calmette–Guerin (BCG) is a weakened, live vaccine that is most commonly used against tuberculosis. Less recognized is its use as intravesical immunotherapy for the adjuvant treatment of intermediate- and high-grade bladder cancer. Despite the weakened state of this strain, BCG-contaminated urine can still lead to local complications of the genitourinary system such as cystitis, pyelonephritis, renal abscess, epididymitis, prostate abscess, and balanitis [15]. BCG-related epididymitis and epididymo-orchitis are rare but can occur up to 10 years after the final intravesical BCG treatment [16]. Differentiation of a mycobacterial scrotal infection from an infection caused by the more common bacterial pathogens is key for proper treatment. If routine antibiotics fail in a patient known to have received BCG therapy, BCG-related infection should be suspected and empiric antimycobacterial treatment should be initiated.
In addition to demonstrating hypoechoic epididymal enlargement on ultrasound images, mycobacterial infections also lead to the development of heterogeneous masses corresponding to granuloma formation. These granulomas have decreased internal flow on color Doppler images with surrounding hyperemia, which can appear less prominent than would be expected in the setting of non-mycobacterial infection (Fig. 6) [17]. The extensive overlap in appearance between mycobacterial infections and non-mycobacterial infections, malignant testicular disease, and testicular torsion make knowledge of previous BCG therapy critical to initiating appropriate treatment without delay.
57-Year-old man with medical history of bladder urothelial carcinoma who had undergone transurethral resection of a bladder tumor and intravesical BCG treatment presented with left scrotal pain. a Sagittal grayscale image shows markedly enlarged left epididymis with heterogeneous masses (arrows) compatible with granulomas. b Sagittal image with power Doppler shows hyperemia surrounding the granulomas, but less than would be expected in a case of bacterial epididymitis. The patient was treated for TB epididymitis as a complication of intravesical BCG treatment
Fournier gangrene
Fournier gangrene is necrotizing fasciitis of the external genitalia, perineum, and perianal region. Patients typically present with fever and sudden onset of pain, swelling, and erythema. This disease classically occurs in middle-aged men (mean age 50–60 years) with a history of diabetes, alcoholism, or immunocompromised state, although women and children can also be affected. The infection is caused by mixed aerobic and anaerobic bacterial flora, with the nidus usually located in the genitourinary tract, gastrointestinal tract, or skin. Fulminant development and progression of tissue necrosis can lead to multiorgan failure and death. Rapid diagnosis, initiation of surgical debridement, and aggressive antibiotic treatment are critical to reduce the high mortality rate, which ranges from 15 to 50% [18].
Fournier gangrene is a clinical diagnosis; when suspicion for this disease is high, treatment should not be delayed for imaging confirmation. On physical examination, the presence of gas-forming organisms cause the characteristic crepitus, although this finding is identified in only 19% to 64% of patients [18]. Cellulitis, deep vein thrombosis, and myositis can have similar appearances on physical examination, with different management approaches used for each condition.
Emergent computed tomography (CT) is generally considered the imaging modality of choice when a definitive diagnosis cannot be made clinically or when preoperative evaluation of the disease extent is desired. Imaging findings include soft tissue thickening, fat stranding, and subcutaneous emphysema dissecting the fascial layers (Fig. 7b). CT may also show the underlying source of infection such as bowel perforation or fistula. This modality can also be used to identify complications of Fournier gangrene such as abscess. Ultrasound is not routinely performed as first-line imaging for this condition, but this technique has been shown to be effective for facilitating early recognition in the emergency department setting (sensitivity 88.2%, specificity 93.3%) [19]. Diffuse subcutaneous tissue thickening, perifascial fluid accumulation, and bright echogenic foci with dirty shadowing and reverberation artifacts corresponding to the underlying soft tissue gas are indicative of Fournier gangrene (Fig 7a).
63-Year-old man with medical history of diabetes mellitus and HIV presented after 5 days of scrotal pain and swelling; he was tachycardic and hypotensive at presentation. a Sagittal grayscale image shows right scrotal wall thickening (asterisk) and multiple linear echogenic foci with dirty shadowing (arrowheads) indicative of soft tissue gas. b CT axial image better depicts the pockets of gas and inflammatory changes in the right inguinal canal and scrotal wall (arrows)
Vascular etiologies of the acute scrotum
Testicular torsion
Testicular torsion occurs when the testis and spermatic cord twist within the scrotum, resulting in vascular occlusion and subsequent infarction if not immediately corrected. Torsion can occur at any age, although it most commonly affects young boys in a bimodal distribution, with peaks in the first year of life and in early adolescence [20]. The “bell-clapper deformity” is a congenital anatomic variant involving failure of the normal posterior attachment of the tunica vaginalis, which instead completely encircles the epididymis, distal spermatic cord, and testis. This allows for increased movement and rotation of the testes within the scrotum, increasing the risk of testicular torsion. Twisting of the spermatic cord leads to obstruction of the testicular vessels; initially venous flow is compromised, followed by arterial flow. Partial torsion can occur when the spermatic cord is rotated less than 450°, allowing arterial inflow to persist, whereas complete torsion of the cord obstructs both arterial and venous flow [21]. Torsion can also be intermittent; this is sometimes referred to as torsion–detorsion syndrome. Patients with this condition typically report acute-onset unilateral scrotal pain of short duration (usually < 2 h) that spontaneously resolves and recurs. Adolescent boys are most commonly affected (mean age 12.2 years; range 4–17 years), with multiple episodes occurring before surgery is performed (mean 4.3 episodes; range 1–30 episodes) [22].
Testicular torsion is a clinical diagnosis, with a typical presentation of nausea, vomiting, and severe unilateral scrotal pain at rest. Physical examination may show an elevated testicle, absence of ipsilateral cremasteric reflex, and scrotal skin changes [23]. When patient history and physical examination are suggestive of torsion, immediate surgical exploration is indicated and should not be delayed for imaging confirmation, as testicular viability is directly related to the duration of ischemia. TWIST (Testicular Workup for Ischemia and Suspected Torsion) is an eight-point scoring system that uses urologic history and physical examination to stratify the risk of testicular torsion; this system has been validated in the pediatric population (3 months–18 years). Children with high TWIST scores benefit from immediate urological consultation without an initial scrotal ultrasound evaluation [3, 24]. Reducing the time to manual or surgical detorsion is of primary concern to preserve testicular viability. Surgical detorsion performed within 6 h of symptom onset is associated with 100% viability; the viability rate drops to 0% to 20% if detorsion takes place 12 to 24 h after symptom onset [1].
The clinical findings of testicular torsion overlap with those of other acute scrotal pathologies. When a diagnosis of torsion cannot be made based on clinical findings alone, scrotal ultrasound is indicated. When absent or decreased blood flow is identified on color Doppler images, the sensitivity and specificity of this modality for identifying torsion reach 90% and 98% to 99%, respectively [25]. Decreased or absent venous flow on color Doppler imaging is the earliest finding of torsion, followed by decreased or absent arterial flow. The imaging features on grayscale ultrasound vary with the degree of ischemia. For patients who present rapidly after the onset of symptoms, the testicle can still appear normal. During the first 24 h after symptom onset (acute phase), there is testicular enlargement, heterogeneity, and hypoechogenicity representing edema. Twisting of the spermatic cord, scrotal skin thickening, and secondary hydrocele may also be observed (Fig. 8). CEUS can clearly demonstrate the absence of testicular vascularity, but currently there are no data to suggest that the use of this modality adds any clinical significant information than that provided by unenhanced color Doppler ultrasound [4].
15-Year-old boy with right testicular pain and swelling for 3 days. a Transverse grayscale image shows mildly heterogeneous echotexture of the right testicle with swirling of the spermatic cord (whirlpool sign) (arrows). b Transverse image with power Doppler shows absent flow. Emergent surgical exploration demonstrated a 720° complete torsion of the right spermatic cord with a nonviable right testicle, requiring orchiectomy
Partial torsion demonstrates variable testicular flow on ultrasound depending on the severity of vascular obstruction; this can lead to false negative ultrasound studies and inaccurate alternative diagnoses. Testicular torsion has also been reported in cases demonstrating normal testis perfusion on color Doppler images [26]. Analysis of the spectral Doppler waveform can aid in the diagnosis of partial torsion. Reversal of diastolic flow or decreased amplitude of the arterial waveform can indicate vascular compromise [27, 28]. Power Doppler imaging has a higher sensitivity to low blood flow and can frequently detect slow flow when the color Doppler signal is absent. The grayscale features of the epididymis and testicle are more likely to appear normal or with mild enlargement due to delayed onset of ischemic changes. Identification of a twisted spermatic cord is the most specific ultrasound sign of torsion, particularly when testicular vascular flow is preserved, because it reveals the actual anatomic abnormality (Fig. 9). The “whirlpool sign” refers to a spiral twist of the spermatic cord at the external inguinal ring that may be associated with an oval, heterogeneously echogenic pseudomass below the point of torsion. The pseudomass corresponds to a congested epididymis, vas deferens, and distal cord vessels. Careful examination of the spermatic cord to identify the whirlpool sign is essential for detecting partial torsion in patients presenting with acute scrotal disease [8, 29,30,31].
10-Year-old boy with left testicular pain and swelling upon waking, associated with nausea, vomiting, and absent cremasteric reflex on physical examination. a Sagittal grayscale image shows homogeneous echogenicity of the left testicle with incidental microlithiasis (asterisk) and swirling of the spermatic cord (whirlpool sign) (arrows). b and c Transverse color Doppler image of both testicles (b) shows absent left testicular flow (asterisk), although sagittal spectral image (c) shows a waveform, indicating some residual vascular flow. Emergent surgical exploration demonstrated a 360° partial spermatic cord torsion with a viable left testis after detorsion. Bilateral orchiopexy was performed
Intermittent torsion can be a clinical and imaging diagnostic dilemma, as symptoms and torsion may have resolved by the time of presentation. The imaging features depend on the severity and duration of the torsion and the time between detorsion and ultrasound imaging. Ultrasound findings may be normal in cases of delayed presentation, intermittent partial torsion, and short durations of compromised vascular flow (Fig. 10). Ultrasound imaging in patients who present within a few hours after severe torsion and complete detorsion will demonstrate hypoechoic enlargement of the epididymis and testis and a straight spermatic cord. Reperfusion after early ischemia can induce a reactive hyperemia on color Doppler imaging, which is not sonographically distinguishable from the hyperemia seen with acute epididymo-orchitis. The most consistent ultrasound finding among patients with intermittent torsion is the horizontal lie of the testis, which corresponds to the clinical findings of a bell-clapper deformity. A clinical history of waxing and waning testicular pain, presence or absence of fever, and laboratory markers for infection (e.g., abnormal urinalysis and white blood cell count) must be integrated into the evaluation to differentiate between a spontaneously detorsed testis and epididymis/epididymo-orchitis. The diagnosis of intermittent torsion is critical, as this condition can develop into complete torsion if untreated. When intermittent torsion is correctly diagnosed, bilateral orchiopexy can prevent further testicular ischemia and potential testicular loss [31].
16-Year-old boy with acute-onset left testicle pain and swelling that occurred when he was lifting weights but had improved by the time of presentation. a Transverse color Doppler image shows swirling of the left spermatic cord and vessels (whirlpool sign) (arrows). b Transverse grayscale image shows a rounded heterogeneously echogenic “pseudomass” below the point of torsion (asterisk). c Sagittal image with color and spectral Doppler demonstrates a homogeneous left testicle with decreased flow and a tardus parvus arterial waveform suggestive of a partial nonocclusive torsion. At the time of emergent surgical exploration, the left testicle appeared slightly dusky but had spontaneously detorsed. Bilateral orchiopexy was performed to prevent a recurrence and further ischemia
Delayed presentations and misdiagnoses of patients with testicular torsion more than 24 h after symptom onset (subacute phase) directly affect testicular salvageability. Atypical cases more likely to lead to delayed presentation and treatment include patients with isolated abdominal pain; patients with developmental, cognitive, or social disorders; young patients, who tend to hide or minimize scrotal pain; and patients with a history of recent genital trauma. Orchiectomy is performed more than three times as often with a delayed rather than acute presentation, consistent with the natural progression of torsion [32]. On ultrasound, the degree of parenchymal heterogeneity and hypoechogenicity increases as ischemia progresses. After 24 h, focal regions of hypoechogenicity and hyperechogenicity represent areas of infarction and hemorrhage and the peritesticular tissues become hyperemic as a reactive vascular response (Fig. 11).
4-Year-old boy had nausea, vomiting, and abdominal pain for 1 day before parents noticed abnormal gait and discovered left scrotal swelling and pain. a Sagittal grayscale image shows an enlarged heterogeneous left testicle (arrows). b Sagittal color Doppler image shows absent flow within the left testicle, peritesticular hyperemia, and focal regions of hypoechogenicity (diamond) representing areas of infarction and hemorrhage. Emergent surgical exploration confirmed the presence of spermatic cord torsion and testicular infarction requiring orchiectomy
Torsed testicular appendage
Torsion of a testicular appendage is the most frequent cause of an acute scrotum in pediatric patients. Testicular appendages are vestigial remnants of the mesonephric and paramesonephric ducts, consisting of vascularized connective tissue along the testicle and epididymis. The appendages are most commonly sessile, stalk-like, or pedunculated structures, although they can have other shapes [33]. The appendages are freely mobile at their site of attachment to the testis, predisposing them to torsion, with the stalk-like morphology associated with the highest likelihood of torsion [34]. The most commonly affected patients are between 7 and 14 years old; presentation beyond the age of 20 is rare, perhaps because local fibrosis limits the risk of torsion [35]. The left side is more frequently affected than the right.
There are five described appendages: (1) the appendix testis (hydatid of Morgagni), (2) the appendix epididymis, (3) the cranial vas aberrans (cranial organ of Haller), (4) the caudal vas aberrans (caudal organ of Haller), and (5) the paradidymis (organ of Giraldes). The appendix testis is involved in 92% of cases of appendage torsion; this appendage is usually pedunculated and is present in more than 80% of children. It is located at the superior aspect of the testis in the groove between the testicle and the epididymal head. The appendix epididymis is located at the epididymal head and is present in approximately 20% of children [36,37,38]. The caudal and cranial vas aberrans originate off the epididymal body and tail, and the paradidymis attaches to the lower aspect of the spermatic cord, but these appendages are only occasionally identified (Fig. 12). Differentiation among the appendices is not clinically relevant for management of torsion.
Scrotal appendages are vestigial remnants along the testicle, epididymis, and spermatic cord. There are five appendages: (1) appendix testis, which attaches to the superior testicle pole; (2) appendix epididymis, which attaches to the epididymal head; (3) cranial vas aberrans, which attaches to the epididymal body; (4) caudal vas aberrans, which attaches to the epididymal tail; and (5) paradidymis, which attaches to the lower spermatic cord. Identification of the particular appendage affected is not clinically relevant for management; cases of appendage torsion are typically referred to as torsed testicular appendage regardless of the location
On ultrasound images, appendages are more readily apparent in the presence of a hydrocele. Normal appendages appear isoechoic to the epididymis, with flow demonstrated on color Doppler imaging (Fig. 13). When torsed, the appendages present as enlarged, rounded, extratesticular masses, with mixed hyperechoic and heterogeneous echotexture depending on the degree of ischemia. There is absent flow on color Doppler imaging, and hyperemia of the surrounding structures can be observed. Secondary findings include enlarged epididymal head, reactive hydrocele, and scrotal skin thickening (Fig. 14) [36, 39].
a–c Sagittal grayscale images in three patients with hydroceles and incidentally detected small exophytic lesions isoechoic to the adjacent testicle or epididymis, representing normal scrotal appendages of different morphologies: bilobulated appendix epididymis (arrows) from the epididymal head (asterisk) (a), ovoid appendix testis from the superior testicular pole (arrow) (b), and elongated tube-shaped appendix testis from the superior testicular pole (arrow) (c)
10-Year-old boy with 10 days of increasing right testicular pain, swelling, and erythema. a Sagittal grayscale image shows a mixed echogenicity lesion anterior to the right epididymal head (arrow) and small hydrocele (asterisks). b Transverse color Doppler image of the same structure shows minimal internal flow. These findings were consistent with a torsed right appendix epididymis, which was treated nonsurgically with ibuprofen for pain
The onset of scrotal pain with appendage torsion is typically more gradual than with testicular torsion, with the pain progressing over several days before the patient seeks treatment. Less than one-third of patients develop a pathognomonic scrotal bluish nodule on physical examination (“blue dot sign”) [34]. Appendage torsion is a self-limiting condition that is managed by bed rest and nonsteroidal anti-inflammatory drugs, with pain usually resolving within a week. Differentiating appendage torsion from testicular torsion is a major challenge based on clinical findings alone. Accurate ultrasound diagnosis is therefore essential, as this can obviate the need for surgical exploration.
Segmental testicular infarction
Segmental testicular infarction is a partial ischemic process that can occur as a sequela of recent surgery, scrotal infection, or hematologic disorders such as sickle cell disease, polycythemia, or vasculitis. It is a rare entity, with most reported cases causing acute scrotal pain in men aged 20 to 40 years [40].
Segmental ischemia appears on ultrasound as a geographic or wedge-shaped hypoechoic abnormality that is avascular or hypovascular on color Doppler imaging. A peripheral hyperemic rim may be identified. The unaffected testicular parenchyma demonstrates normal blood flow. The ischemic region usually involves the superior aspect of the testicle due to poor collateral vessels (Fig. 15). CEUS can be used to confirm equivocal findings on conventional ultrasound studies. CEUS findings of segmental infarction include avascular lobules with a peripheral hyperemic rim in the subacute period (2 to 17 days). On surveillance imaging the peripheral hyperemic rim diminishes and the avascular lobule decreases in size [4, 41].
52-Year-old man developed right scrotal pain and swelling after right nephrectomy and lymph node dissection. a Sagittal grayscale image shows a geographic hypoechoic region in the superior aspect of the right testicle (asterisk). b Sagittal color Doppler image shows absent flow in the hypoechoic region (asterisk) and a peritesticular hyperemic rim. These findings were consistent with segmental infarct
The ability to definitively distinguish between this condition and a hypovascular testicular tumor on ultrasound can be difficult; therefore, MRI is often used for confirmation in equivocal cases. T1/T2-weighted signal intensity on MRI depends on the age of the infarct and whether hemorrhage is present. Postcontrast T1-weighted images show a nonenhancing geographic defect with peripheral enhancement (Fig. 16) [40]. Accurate diagnosis combined with short-term follow-up ultrasound or CEUS imaging to ensure expected evolution can prevent unnecessary orchiectomy, as conservative treatment is the standard of care for this condition.
52-Year-old man with left groin pain and subjective fever for several days. a Side-by-side color Doppler images of the left testicle in sagittal (left-side) and transverse (right-side) planes show an ill-defined hypoechoic area in the posterior lower pole with minimal flow (arrows) and small hydrocele (asterisks). Ultrasound findings were nonspecific, potentially representing a region of focal ischemia or a hypovascular tumor, and so follow-up MRI was performed. b Coronal T2-weighted MR image of the scrotum confirms the presence of a small T2 hyperintense hydrocele (asterisk). c Sagittal contrast-enhanced T1-weighted MR image shows wedge-shaped region of nonenhancement in the inferior posterior testis (arrow) corresponding to the abnormality on ultrasound imaging. No solid or enhancing mass was identified. These findings were consistent with a segmental testicular infarct
Traumatic etiologies of the acute scrotum
Scrotal trauma is the third most common cause of the acute scrotum after infection (epididymo-orchitis) and torsion (testicular appendage or spermatic cord), but this type of trauma represents < 1% of traumatic injuries overall. These traumatic injuries are most common in young men aged 15 to 24 years [42]. The typical mechanisms of injury include blunt trauma from sports-related injuries or from bicycle, car, or motorcycle crashes and penetrating trauma from assault by firearm [24, 43]. Testicular mobility within the scrotum can often prevent significant force from being generated during blunt trauma; it takes approximately 50 kg of force to rupture the tunica albuginea. Serious injury typically occurs when there is testicular entrapment and compression against the pubic bone or thigh [44]. The right testicle is often anatomically higher than the left testicle, leading to more frequent entrapment and injury during blunt trauma [43].
Clinical history and physical examination are usually sufficient for diagnosing testicular injury from scrotal trauma, although these methods are limited in determining the extent and severity of the injury. A variety of injuries can occur, including testicular rupture, dislocation, fracture, hematoma, and torsion, as well as epididymal, scrotal, and urethral injuries. The American Urological Association recommends early scrotal exploration and debridement in all patients with suspected testicular rupture to prevent testicular loss, infection, and infertility [45]. Exploratory surgery performed within 72 h after the injury can salvage up to 90% of blunt testicular rupture cases; when surgery is delayed beyond this time point, the orchiectomy rate is 45% [46]. Ultrasound is a valuable diagnostic technique for identifying scrotal and testicular traumatic injuries that require surgical intervention. CEUS can be used as a rapid, bedside imaging adjunct in the emergency setting when more precise delineation of tissue viability is needed to enable organ-sparing treatment [4].
Testicular rupture
Testicular rupture refers to a tear in the tunica albuginea that results in extrusion of testicular contents. In several studies, the sensitivity of ultrasound for detecting testicular rupture reached 100%, which provides reassurance when ultrasound results are negative for rupture [47, 48]. The main ultrasound findings for testicular rupture include a heterogeneous testicle, contour abnormality, and disruption of the tunica albuginea. Mixed echogenicity of the testicular parenchyma reflects hemorrhage and necrosis. Disruption of the normal testicular contour indicates parenchyma extrusion. Color Doppler imaging demonstrates focal or diffuse loss of vascularity, which usually requires surgical debridement (Fig. 17). In a retrospective review of patients sustaining blunt trauma with a non-diagnostic clinical examination, ultrasound findings of testicular heterogeneity with contour abnormality demonstrated a sensitivity of 100% and specificity of 93.5% for detecting testicular ruptures [47].
14-Year-old boy with left scrotal pain 5 days after being kneed in the groin at wrestling camp. a Sagittal color Doppler image of the left testicle shows focal disruption of the tunica albuginea (arrow) with heterogeneous material extending beyond the expected margin of the testis (circle), indicative of extruded parenchyma. An associated hematocele is present (diamond). There is absent flow in the extruded lower pole (circle) and preserved flow in the remaining testicular parenchyma (asterisk). b Surgical exploration confirmed testicular rupture with extruded testicular parenchyma (arrow) and approximately 50% viable testicle
Testicular fracture
Testicular fracture occurs when there is disruption of the testicular parenchyma with preserved testicular shape and integrity of the hyperechoic tunica albuginea. The fracture plane appears as an avascular linear hypoechoic band extending across the parenchyma. Associated hematocele and testicular hematomas can be present. Identification of vascular flow on color Doppler images in the surrounding parenchyma is critical for determining salvageability; preserved flow allows for conservative management, whereas absent flow requires emergent surgical debridement (Fig. 18) [49]. When conventional ultrasound findings are equivocal, CEUS can better delineate fracture lines and distinguish between surrounding enhancing viable parenchyma and nonenhancing devascularized tissue [4].
54-Year-old man with right testicular swelling after being hit with a baseball 1 week earlier. a Sagittal grayscale image of the right testicle shows a linear hypoechoic fracture line extending across the parenchyma (arrows) with preservation of the tunica albuginea and an associated hematocele (asterisk). b Sagittal color Doppler image shows preserved flow in the surrounding parenchyma, prompting conservative management. Serial follow-up ultrasound imaging demonstrated interval improvement, and surgical debridement was avoided
Scrotal hematoma
Post-traumatic hematomas can occur anywhere within the scrotum, appearing as intratesticular hematomas, extratesticular hematomas involving the epididymis and scrotal wall, and hematomas collecting between the visceral and parietal layers of the tunica vaginalis (hematoceles). Ultrasound features depend on the chronicity of the evolving blood products; hematoceles and focal testicular, epididymal, and scrotal wall hematomas are acutely hyperechoic with decreasing echogenicity and increasing complexity (septa, loculations, and fluid levels) as they evolve to subacute and chronic phases. Hematomas have no internal flow on color and power Doppler images.
Whereas scrotal hematomas in the presence of suspected testicular rupture (physical examination or ultrasound findings) have been shown to benefit from prompt surgical exploration, the management for cases in which testicular rupture is not suspected is less well-defined. Current recommendations suggest that conservative management can be used for small intratesticular hematomas, subcutaneous hematomas without hematocele, and small hematoceles when the tunica albuginea is intact, but that large hematomas should be surgically explored. The size of hematoma that should prompt surgical exploration has not been defined. When conservative management is used, serial ultrasound examinations in the first 72 h should be performed to confirm stability. When there is increasing pain or expansion of the hematoma, scrotal surgical exploration should be considered [50,51,52].
Testicular tumors
Testicular germ cell tumors are the most common solid cancer in males aged 15 to 35 years, accounting for approximately 21% of all neoplasms in male adolescents and young adults [53]. Because traumatic injury preferentially affects this age group, up to 10% to 15% of testicular tumors are incidentally identified by ultrasound performed in patients with acute scrotal trauma [5]. Testicular tumors frequently appear as well-defined, hypoechoic or heterogeneous echogenicity intratesticular lesions. Differentiating between these lesions and evolving focal hematomas can be difficult in cases of trauma. A short-term follow-up ultrasound examination increases confidence in the diagnosis, as a hematoma would be expected to improve over time whereas a mass would be expected to grow. When ultrasound findings are equivocal, scrotal MRI with and without intravenous contrast can be used for more definitive characterization (Fig. 19).
26-Year-old man with right testicular pain and swelling after scrotal trauma. a Sagittal color Doppler image shows a well-circumscribed, heterogeneous, primarily solid-appearing process in the center of the right testicle, with no internal flow (arrows). This was initially believed to represent a hematoma in the context of trauma; however, because a neoplasm could have a similar appearance, MRI was recommended. b Sagittal precontrast T2-weighted MR image shows a well-circumscribed, complex mass with cystic and solid components (arrowhead) and a large hydrocele (asterisk). c and d Sagittal precontrast T1-weighted image (c) and postcontrast T1-weighted image (d) demonstrate enhancing solid components within the mass (arrowheads). Right orchiectomy was performed, confirming testicular teratoma
Miscellaneous etiologies of the acute scrotum
Acute idiopathic scrotal edema
Acute idiopathic scrotal edema is a benign, self-limiting condition that is characterized by acute-onset edema and erythema of the scrotal skin and dartos fascia without involvement of the testes or epididymis. Additional involvement of the perineum and inguinal region is common. Patients have mild or no associated pain, normal white blood cell counts and urinalysis results, and no fever. Most cases occur in young children (5–8 years old) and account for up to 12% of prepubertal acute scrotum presentations. Adult cases are reported rarely. Infectious and allergic angioedema etiologies have been suggested, although strong supportive evidence is lacking. Bed rest, nonsteroidal anti-inflammatory drugs, and antibiotics have been used to manage this condition with unclear efficacy; symptoms tend to resolve regardless of treatment in 3 to 5 days, but approximately 10% of patients experience a recurrence [54,55,56].
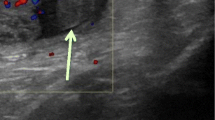
Characteristic findings on ultrasound are marked edematous thickening of the scrotal wall and normal appearance of the testes and epididymis. A small reactive hydrocele may be observed. Hypervascular peritesticular scrotal soft tissues on color Doppler images are highly suggestive of the diagnosis (“fountain sign”). There is no associated testicular or epididymal hyperemia and testicular perfusion is preserved, which can help to distinguish this condition from more concerning infectious and ischemic diseases (Fig. 19). Acute idiopathic scrotal edema is a diagnosis of exclusion, but knowledge of this entity and correct identification can prevent unnecessary surgery [54,55,56].
Referred scrotal pain
Acute scrotal pain can present as referred pain from non-scrotal disease. Renal colic refers to the type of flank pain associated with obstructing urinary calculi, which can radiate to the scrotum or occasionally present as localized acute scrotal pain. The referred pain is due to common innervation of the renal pelvis, proximal ureter, and ipsilateral testicle, as well as the distal ureter and scrotum. The common associated symptoms of nausea, vomiting, and dysuria with gross or microscopic hematuria can be used to differentiate renal colic from acute scrotal pathology [57, 58]. When the presentation is clinically indeterminate or when the initial workup shows a normal scrotum on ultrasound, renal ultrasound is warranted to evaluate for a urinary tract obstruction (calculus or hydronephrosis) as the cause of referred pain.
Conclusion
Patients presenting with an acute scrotum require Rapid diagnoses so that clinicians can differentiate between nonsurgical cases and those requiring acute surgical intervention. Acute testicular torsion, testicular rupture, and Fournier gangrene necessitate rapid scrotal exploration to salvage testicular function and decrease associated morbidity and mortality. Epididymitis, epididymo-orchitis, torsed testicular appendage, segmental testicular infarction, scrotal hematomas, testicular neoplasms, and acute idiopathic scrotal edema can have similar presentations, but these conditions do not require immediate surgery. Clinical history and physical examination alone are often insufficient for determining the correct care pathway, and in such cases, adjunct imaging should be performed. Ultrasound is the first-line imaging test to evaluate scrotal pathology due to its rapid availability in the emergency setting and its ability to assess vascular flow. When ultrasound findings are combined with clinical presentation, laboratory values, and physical examination, the radiologist can differentiate between surgical and nonsurgical scrotal pathology. For equivocal nonsurgical cases, MRI can provide superior localization; identification of fat, blood products, and fibrous tissue; and differentiation between avascular cases, such as intratesticular hematoma or segmental testicular infarct, and hypovascular neoplasms. More recently, CEUS has shown utility as a rapid, non-nephrotoxic, nonionizing imaging adjunct that can aid in the detection of segmental infarction, assessment of viable parenchyma after trauma, and differentiation of testicular tumors, potentially reducing the need for further imaging. The ability to identify the various acute scrotal entities is critical for the initiation of proper treatment.
References
Middleton WD, Middleton MA, Dierks M, Keetch D, Dierks S (1997) Sonographic prediction of viability in testicular torsion: preliminary observations. J Ultrasound Med 16:23-27.
Remer EM, Casalino DD, Arellano RS et al (2012) ACR Appropriateness Criteria ® acute onset of scrotal pain–without trauma, without antecedent mass. Ultrasound Q 28:47-51.
Wang CL, Aryal B, Oto A, et al (2019) ACR Appropriateness Criteria: Acute Onset of Scrotal Pain-Without Trauma, Without Antecedent Mass. J Am Coll Radiol, 16:5:S38-S43.
Sidhu P, Cantisani V, Dietrich C, et al (2018) The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med 39:e2-e44.
Dogra V, Bhatt S (2004) Acute painful scrotum. Radiol Clin North Am 42:349-363.
Dogra VS, Gottlieb RH, Oka M, Rubens DJ (2003) Sonography of the scrotum. Radiology 227:18-36.
Guideline developed in collaboration with the American College of Radiology; Society for Pediatric Radiology; Society of Radiologists in Ultrasound (2015) AIUM Practice Guideline for the Performance of Scrotal Ultrasound Examinations. J Ultrasound Med 34:1-5.
Baud C, Veyrac C, Couture C, Ferran JL (1998) Spiral twist of the spermatic cord: a reliable sign of testicular torsion. Pediatr Radiol 28:950-954.
Kühn AL, Scortegagna E, Nowitzki KM, Kim YH (2016) Ultrasonography of the scrotum in adults. Ultrasonography 35:180-197.
Berger RE, Alexander ER, Harnisch JP, et al (1979) Etiology, manifestations and therapy of acute epididymitis: prospective study of 50 cases. J Urol 121:750-754.
Horstman WG, Middleton WD, Melson GL (1991) Scrotal inflammatory disease: color Doppler US findings. Radiology 179:55-59.
Keener TS, Winter TC, Nghiem HV, Schmiedl UP (1997) Normal adult epididymis: evaluation with color Doppler US. Radiology 202:712-714.
Lavallee ME, Cash J (2005) Testicular torsion: evaluation and management. Curr Sports Med Rep 4:102-104.
Fehily SR, Trubiano JA, McLean C, et al (2015) Testicular loss following bacterial epididymo-orchitis: Case report and literature review. Can Urol Assoc J 9:E148-E151.
Green DB, Kawashima A, Menias CO, et al (2019) Complications of Intravesical BCG Immunotherapy for Bladder Cancer. Radiographics 39:80-94.
Lamm DL, van der Meijden PM, Morales A, et al (1992) Incidence and treatment of complications of bacillus Calmette-Guerin intravesical therapy in superficial bladder cancer. J Urol 147:596-600.
Demers V, Pelsser V (2012) “BCGitis”: A rare case of tuberculous epididymo-orchitis following intravesical Bacillus Calmette- Guérin therapy. J Radiol Case Rep 6:16-21.
Levenson RB, Singh AK, Novelline RA (2008) Fournier gangrene: role of imaging. Radiographics 28:519-528.
Yen Z, Wang HP, Ma HM, Chen SC, Chen WJ (2002) Ultrasonographic screening of clinically-suspected necrotizing fasciitis. Acad Emerg Med 9:1448-1451.
Zhao LC, Lautz TB, Meeks JJ, Maizels M (2011) Pediatric testicular torsion epidemiology using a national database: incidence, risk of orchiectomy and possible measures toward improving the quality of care. J Urol 186:2009-2013.
Lee FT Jr, Winter DB, Masden FA, et al (1996) Conventional color Doppler velocity sonography versus color Doppler energy sonography for the diagnosis of acute experimental torsion of the spermatic cord. AJR Am J Roentgenol 167:785-790.
Eaton SH, Cendron MA, Estrada CR, et al (2005) Intermittent testicular torsion: diagnostic features and management outcomes. J Urol 174:1532-1535.
Srinivasan A, Cinman N, Feber KM, Gitlin J, Palmer LS (2011) History and physical examination findings predictive of testicular torsion: an attempt to promote clinical diagnosis by house staff. J Pediatr Urol 7:470-474.
Frohlich LC, Paydar-Darian N, Cilento BG Jr, Lee LK (2017) Prospective Validation of Clinical Score for Males Presenting With an Acute Scrotum. Acad Emerg Med 24:1474-1482.
Baker LA, Sigman D, Mathews RI, Benson J, Docimo SG (2000) An analysis of clinical outcomes using color doppler testicular ultrasound for testicular torsion. Pediatrics 105:604-607.
Bentley DF, Ricchiuti DJ, Nasrallah PF, McMahon DR (2004) Spermatic cord torsion with preserved testis perfusion: initial anatomical observations. J Urol 172:2373-2376.
Cassar S, Bhatt S, Paltiel HJ, Dogra VS (2008) Role of spectral Doppler sonography in the evaluation of partial testicular torsion. J Ultrasound Med 27:1629-1638.
Dogra VS, Rubens DJ, Gottlieb RH, Bhatt S (2004) Torsion and beyond: new twists in spectral Doppler evaluation of the scrotum. J Ultrasound Med 23:1077-1085.
Munden MM, Williams JL, Zhang W, Crowe JE, Munden RF, Cisek LJ (2013) Intermittent testicular torsion in the pediatric patient: sonographic indicators of a difficult diagnosis. AJR Am J Roentgenol 201:912-918.
Kalfa N, Veyrac C, Baud C, Couture A, Averous M, Galifer RB (2004) Ultrasonography of the spermatic cord in children with testicular torsion: impact on the surgical strategy. J Urol 172:1692-1695.
Vijayaraghavan SB (2006) Sonographic differential diagnosis of acute scrotum: real-time whirlpool sign, a key sign of torsion. J Ultrasound Med 25:563-574.
Bayne CE, Villanueva J, Davis TD, Pohl HG, Rushton HG (2017) Factors Associated with Delayed Presentation and Misdiagnosis of Testicular Torsion: A Case-Control Study. J Pediatr 186:200-204.
Rafailidis V, Apostolou D, Charsoula A, Rafailidis D (2015) Sonography of the scrotum: from appendages to scrotolithiasis. J Ultrasound Med 34:507-518.
Sellars ME, Sidhu PS (2003) Ultrasound appearances of the testicular appendages: pictorial review. Eur Radiol 13:127-135.
Puri P, Boyd E (1976) Torsion of the appendix testis. A survey of 22 cases. Clin Pediatr (Phila) 15:949-950.
Baldisserotto M, de Souza JC, Pertence AP, Dora MD (2005) Color Doppler sonography of normal and torsed testicular appendages in children. AJR Am J Roentgenol 184:1287-1292.
Skoglund RW, McRoberts JW, Ragde H (1970) Torsion of testicular appendages: presentation of 43 new cases and a collective review. J Urol 104:598-600.
Ruiz Montes AM, Jimenez Alvarez C, Nunez Nunez R, Cabrera R, Blesa Sanchez E (1994) [The clinical characteristics of patients with torsion of the testicular and epididymal appendages]. Cir Pediatr 7:140-142.
Lev M, Ramon J, Mor Y, Jacobson JM, Soudack M (2015) Sonographic appearances of torsion of the appendix testis and appendix epididymis in children. J Clin Ultrasound 43:485-489.
Fernández-Pérez GC, Tardáguila FM, Velasco M, et al (2005) Radiologic findings of segmental testicular infarction. AJR Am J Roentgenol 184:1587-1593.
Bertolotto M, Derchi LE, Sidhu PS, et al (2011) Acute segmental testicular infarction at contrast-enhanced ultrasound: early features and changes during follow-up. AJR Am J Roentgenol 196:834-841.
Søreide K (2009) Epidemiology of major trauma. Br J Surg 96:697-698.
Bhatt S, Dogra VS (2008) Role of US in testicular and scrotal trauma. Radiographics 28:1617-1629.
Mulhall JP, Gabram SG, Jacobs LM (1995) Emergency management of blunt testicular trauma. Acad Emerg Med 2:639-643.
Morey AF, Brandes S, Dugi DD 3rd, et al; American Urological Association (2014) Urotrauma: AUA guideline. J Urol 192:327-335
Lupetin AR, King W 3rd, Rich PJ, Lederman RB (1983) The traumatized scrotum: ultrasound evaluation. Radiology 148:203-207.
Buckley JC, McAninch JW (2006) Use of ultrasonography for the diagnosis of testicular injuries in blunt scrotal trauma. J Urol 175:175-178.
Guichard G, El Ammari J, Del Coro C, et al (2008) Accuracy of ultrasonography in diagnosis of testicular rupture after blunt scrotal trauma. Urology 71:52-56.
Deurdulian C, Mittelstaedt CA, Chong WK, Fielding JR (2007) US of acute scrotal trauma: optimal technique, imaging findings, and management. Radiographics 27:357-369.
Bowen DK, Gonzalez CM (2014) Intratesticular hematoma after blunt scrotal trauma: a case series and algorithm-based approach to management. Cent European J Urol 67:427-429.
Lynch TH, Martínez-Piñeiro L, Plas E, et al; European Association of Urology (2005) EAU guidelines on urological trauma. Eur Urol 47:1-15
Morey AF, Metro MJ, Carney KJ, Miller KS, McAninch JW (2004) Consensus on genitourinary trauma: external genitalia. BJU Int 94:507-515.
Bleyer A, O’Leary M, Barr R, Ries LAG (eds) (2006) Cancer Epidemiology in Older Adolescents and Young Adults 15 to 29 Years of Age, Including SEER Incidence and Survival: 1975-2000. National Cancer Institute, NIH Pub. No. 06-5767. Bethesda, Maryland.
Mesquita RD, Rosas JL (2017) Adult Acute Scrotal Edema - When Radiologists Can Help to Avoid Unnecessary Surgical Treatment. J Radiol Case Rep 11:24-30.
Breen M, Murphy K, Chow J, Kiely E, O’Regan K (2013) Acute idiopathic scrotal edema. Case Rep Urol 2013:829345.
Santi M, Lava SAG, Simonetti GD, Bianchetti MG, Milani GP (2018) Acute idiopathic scrotal edema: Systematic literature review. Eur J Pediatr Surg 28:222-226.
Bueschen AJ (1990) Flank pain. In: Walker HK, Hall WD, Hurst JW (eds) Clinical methods: The history, physical, and laboratory examinations, 3rd edn, chap 182. Butterworths, Boston.
McGee SR (1993) Referred scrotal pain: case reports and review. J Gen Intern Med 8:694-701.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
CME activity This article has been selected as the CME activity for the current month. Please visit https://ce.mayo.edu/node/99487 and follow the instructions to complete this CME activity.
Rights and permissions
About this article
Cite this article
Sweet, D.E., Feldman, M.K. & Remer, E.M. Imaging of the acute scrotum: keys to a rapid diagnosis of acute scrotal disorders. Abdom Radiol 45, 2063–2081 (2020). https://doi.org/10.1007/s00261-019-02333-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02333-4