Abstract
Purpose
We aimed to assess and compare ex vivo MRI of resected colorectal carcinoma before and after formalin fixation.
Methods
We enrolled 45 consecutive patients (47 carcinomas) who underwent colorectal carcinoma surgery. Specimens underwent two MR scans at 1.5 T (after resection and 24 h after formalin fixation). Two radiologists evaluated all MR images independently regarding T-staging and the subserosal linear architecture. T-stage accuracy and frequency of linear architecture were calculated. A third radiologist measured vertical tumor distance and contrast-to-noise ratio (CNR) of the mucosa, submucosa, muscularis propria, subserosa, and tumor.
Results
T-stage accuracy compared to histopathology by the two readers was 91.5% and 87.2% before fixation and 91.5% and 85.1% after fixation, respectively. Linear architecture was observed in 11.1% of T2 tumors and 100% of T3 tumors by both readers. The vertical tumor distance between histopathological and MRI findings was well correlated before and after fixation. The measurement error of the vertical tumor distance between before and after fixation was within 3 mm. CNR of the tumor was significantly lower than those of the submucosa and subserosa before and after fixation (p < 0.05). CNRs of the tumor and muscularis propria were decreased after formalin fixation (p < 0.05).
Conclusions
Subserosal linear architecture represented fibrosis with tumoral invasion, suggesting a T3–4 tumor. The submucosa and subserosa showed high intensity and the mucosa and muscularis propria showed low intensity compared with tumor. CNRs of the tumor and muscularis propria were decreased by formalin fixation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Colorectal carcinoma is one of the most common malignant neoplasms worldwide. In 2012, an estimated 1.4 million patients presented with colorectal carcinoma and 693,00 died from this disease worldwide [1]. Accurate preoperative staging of colorectal carcinoma is important in determining optimal therapeutic strategy, and postoperative histopathologic stage is closely related to prognosis. Although CT can assess T-staging of rectal carcinoma with 64%–74% of accuracy [2], it is difficult to distinguish the different colorectal wall layers from actual tumor due to poor soft tissue contrast. Sensitivity and specificity of endoscopic ultrasound (EUS) have been reported to be 81%–96% and 91%–98% and that of MRI to be 87% and 75%, respectively [3], in a previous meta-analysis. EUS is appropriate for assessing superficial tumors and can accurately differentiate Tis–T1 from T2–T4 and Tis–T2 from T3–T4 [4, 5]; however, technical limitations include limited range, artifact in the layer interfaces, difficulty to insert an endoscopic ultrasound probe in stenotic tumor, and high operator dependance [6, 7]. EUS is the preferred technique for the differentiation and staging of T1 [8]. Conversely, MRI is the preferred method for assessing mesorectal fat invasion, mesorectal fascia, and the adjacent organs [9]. MRI can accurately determine extramural depth of tumor invasion [10]. MRI is the standard modality for preoperative local staging and restaging after neoadjuvant treatment of rectal carcinoma [9, 11,12,13] and should be performed for primary staging and restaging of rectal cancer with appropriate MR protocol and structured report system [8, 14]. Additionally, MRI can also assess the T-stage of colon as well as rectal carcinoma [15]. For diagnosing T3cd–T4 colon carcinoma, MRI was 43%–92% sensitive and 69%–77% specific compared to CT at 38%–47% sensitivity and 62%–91% specificity [16,17,18].
T-staging of colorectal carcinoma by MRI correlates well with histopathological findings owing to its high contrast resolution. Previous studies correlated ex vivo MRI obtained from formalin (formaldehyde)-fixed specimen and histopathological findings [19,20,21]. Few articles have mentioned ex vivo MRI findings of colorectal carcinoma before and after fixation [22]; in addition, ex vivo MRI only assessed qualitative signal intensity. It is not known how formalin fixation modifies ex vivo MRI. Therefore, the aim of this study was to compare ex vivo MRI of resected colorectal carcinoma before and after formalin fixation.
Materials and methods
This prospective study was approved by our institutional review board, and prior informed consent for participation was obtained from all patients.
Patients
We included 47 patients who underwent colorectal surgery at our institution between November 2013 and September 2014. Two patients underwent neoadjuvant chemotherapy and one patient who did not undergo colectomy but underwent colostomy owing to peritoneal dissemination were excluded. We finally enrolled 44 consecutive patients with 47 carcinomas (18 males, 26 females; mean age 70.6 years, age range 51–89 years). Of patients, three had 2 simultaneous carcinomas. Histopathology-proved adenocarcinoma located in the cecum (n = 1), ascending- (n = 6), transverse- (n = 7), descending- (n = 3), and the sigmoid colon (n = 15), and rectum (n = 15). These cases included no mucinous type of adenocarcinoma.
MR examinations
Resected specimens underwent 2 MRI studies; the first study was performed immediately after resection with the mesocolon in place; next, the mesocolon was removed to harvest the lymph node, and the formalin-fixed specimen was obtained 24 h after fixation, for which the second MRI study was performed. MRI studies were performed on a 1.5 T scanner (SIGNA HDx 1.5 T, GE Healthcare, Milwaukee, WI) using a 5-channel GP surface coil (GE Healthcare). The specimens were opened along the anterior rectum and on the opposite side of the mesocolon in the colon and examined without fluid. Axial and longitudinal T2-weighted imaging (T2WI) scans were obtained. The parameters for T2WI were TR 5000 ms, TE 103.7 ms, FOV 80 mm, matrix 256 × 224 mm, slice thickness 2 mm, and scan time 9 min and 28 s.
Histopathological examination
All specimens were cut axially and longitudinally through the center to correspond with the MR image orientation. They were embedded in paraffin, cut into thin sections, and stained with hematoxylin–eosin. A pathologist (R.K.) with 30 years of experience determined the T-stage of all resected specimens.
Image analysis
All images were independently reviewed by two radiologists (N.N. and S.O. with 27 and 21 years of experience reading gastrointestinal images, respectively) who were blinded to clinical information. They classified the lesions as Tis (staying in mucosa), T1 (invading into submucosa), T2 (invading into muscularis propria), and T3–4 (invading beyond muscularis propria) on MRI before and after fixation and assessed linear subserosal architecture on MRI before fixation. Another radiologist (A.I. with 8 years of experience reading gastrointestinal images) measured the vertical tumor distance and the contrast-to-noise ratio (CNR) of the mucosa, submucosa, muscularis propria, subserosa, and tumor while correlating with the pathology specimens. Seven lesions were excluded from vertical distance measurement because they were not contained within one slide. CNR was calculated using the following formula:
Statistical analysis
T-staging agreement between histopathological examination and MRI before and after fixation was calculated, and frequency of linear architecture in respective T-stage was revealed. Interobserver agreement for T-stage and linear architecture was compared using kappa statistics and categorized as poor (< 0.20), fair (0.21–0.40), moderate (0.41–0.61), good (0.61–0.80), and excellent (0.81–1.00). The vertical distance by histopathological examination and MRI were compared using Pearson correlation coefficient and Bland–Altman plot. CNRs of the tumor, mucosa, submucosa, muscularis propria, and subserosa on MRI before fixation were compared with those on MRI after fixation using Wilcoxon signed-rank test, and tumor CNR was compared with CNR of the mucosa, submucosa, muscularis propria, and subserosa using Wilcoxon signed-rank test; p values of ≤ 0.05 were considered statistically significant.
Results
Representative microscopic images and ex vivo MRI scans were matched to confirm that the bowel layer on the MRI scan coincided with the pathologically examined structure. With respect to the relationship between MRI and microscopic findings, the first (low intensity) layer is the mucosa, the second (high intensity) is the submucosa, and the third (low intensity) is the muscularis propria; the fat (high intensity) layer is the subserosa (Figs. 1, 2).
A 69-year-old female with descending colon carcinoma (T1). The tumor invades the high-intensity submucosal layer on MRI before (A) and after fixation (B). The intensities of the tumor and muscularis propria decrease on MRI after fixation versus before fixation (A, B). The tumor invading the submucosa is confirmed on histopathology (hematoxylin–eosin stain) (C). Asterisk, tumor; m, mucosa; sm, submucosa; mp, muscularis propria
A 62-year-old male with sigmoid colon carcinoma (T3). The tumor invades subserosa with linear architecture on MRI before (A) and after fixation (B). Histopathology shows the T3 tumor invading the subserosa and speculated fibrosis around the tumor in the subserosa (hematoxylin–eosin stain) (C). Asterisk, tumor; mp, muscularis propria; ss, subserosa; arrow, linear architecture or fibrosis
T-stage accuracy between histopathological examination and MRI before fixation was 91.5% (43/47) for reader 1 and 87.2% (41/47) for reader 2 (Table 1) and between histopathological examination and MRI after fixation was 91.5% (43/47) for reader 1 and 85.1% (40/47) for reader 2 (Table 2). The linear architecture was observed in 1 of 9 (11.1%) T2 tumors and 31 of 31 (100%) T3 tumors by both readers (Table 3, Fig. 2). T-stage interobserver agreement was κ = 0.789 on MRI before fixation, κ = 0.751 on MRI after fixation, and κ = 0.902 in linear subserosal architecture.
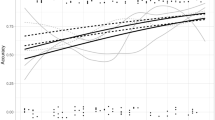
The vertical distance measured by histopathological findings and MRI was well correlated; the regression line and correlation coefficient were y = 0.7774x + 0.3384 and r = 0.894 on MRI before fixation (p < 0.001), and y = 0.7536x + 0.7055 and r = 0.880 on MRI after fixation (p < 0.001), respectively (Fig. 3). Invasion depth discrepancy on MRI between before and after fixation was < 3 mm (Fig. 4). CNRs of the tumor and muscularis propria after fixation were significantly lower than those before fixation (p < 0.001) (Table 4, Fig. 1). Tumor CNR was significantly lower than those of the submucosal layer and subserosa ex vivo MRI both before and after fixation (p < 0.05) (Fig. 5).
The discrepancy of invasion depth on MRI between before and after fixation. Bland–Altman plot demonstrates that discrepancy of invasion depth is within 3 mm. Vertical axis signifies Δinvasion depth calculated as follows: (invasion depth on MRI before fixation)–(invasion depth on MRI after fixation). Horizontal axis signifies mean invasion depth calculated as follows: [(invasion depth on MRI before fixation) + (invasion depth on MRI after fixation)]/2
Contrast-to-noise ratio (CNR) of the tumor, mucosa, submucosa, muscularis propria, and subserosa. CNR of the tumor is significantly lower than that of the submucosa and subserosa before (A) and after (B) fixation. m: mucosa, sm: submucosa, mp: muscularis propria, ss: subserosa. Significance difference (*p < 0.05)
Discussion
T-staging by two readers was almost accurate both before and after fixation. The linear subserosal architecture was observed more frequently in T3 than in T2 tumor. Interobserver agreement was good and excellent regarding T-staging and linear architecture assessment, respectively. Vertical tumor distances evaluated by histopathology and MRI before and after fixation were well correlated. Tumor CNR was significantly lower than in the submucosa and subserosa, and there was no significant difference among CNRs of the tumor, mucosa, and muscularis propria. CNRs of the tumor and muscularis propria decreased after formalin fixation.
Tumor was of low intensity, mucosa was of low intensity, submucosa was of high intensity, muscularis propria was of low intensity, and submucosa was of high intensity on T2WI of ex vivo MRI both before and after formalin fixation, which is consistent with previous studies [19,20,21,22]. Ex vivo MRI was well correlated with histopathological images; however, there was discrepancy in T-staging in some tumors because assessing tumor invasion into the muscularis propria is more difficult than assessing tumor invasion into submucosa and subserosa because tumor CNR was similar to CNR of the muscularis propria, whereas tumor CNR was different from CNR of the submucosa and subserosa.
In correlating ex vivo MRI and histopathological findings, the linear architecture is equivalent to fibrosis with tumoral invasion, known as desmoplastic reaction. Desmoplastic reaction means that the most abundant mesenchymal cells, such as fibroblasts and myofibroblasts, in carcinomatous masses promote tumor progression [23, 24]. Desmoplastic reaction occurs in the submucosa, muscularis propria, and subserosa; however, MRI can depict linear architecture only in the subserosa, as the submucosa’s layer is thin and the muscularis propria is of low intensity same as fibrosis. Previous studies have reported that linear architecture (spiculation) represents a T2 tumor [25], whereas others revealed that this finding represents a T3 tumor [26]; however, our results found that linear architecture represented a T3 tumor. T2 tumor with ulcer or abscess is associated with reparative fibrosis resulting in overdiagnosis. To distinguish tumor with fibrosis is challenging, and recent studies have reported that T2 mapping on 3T MRI scanner can distinguish the tumor with fibrosis as well as the colorectal wall layer [27].
Several studies have been published on fixed specimen of colorectal carcinoma on ex vivo MRI; however, no study discusses specimens of colorectal carcinoma before fixation in detail. There is still uncertainty regarding the difference in MRI findings of colorectal carcinoma specimen before and after formalin fixation. Therefore, this research demonstrates the change in MRI findings of formalin-fixed colorectal carcinoma specimens.
Fixation preserves tissue morphology, prevents bacterial influence and change in volume and shape by protein stabilization, and prevents autolysis by means of alcohol-based fixatives, glutaraldehyde, or formalin [28]. Formalin is a widely used fixative in diagnostic pathology, and 10% buffered formalin is considered an appropriate fixative [29, 30]. The mechanism of action of formalin is the formation of intra- and intermolecular crosslinks. The main crosslink occurs between the side chain amino group, which results in the formation of methylene bridge [28]. The chemical formula for formalin fixation is shown as follows:
–NH2: amino group, HCHO: formaldehyde, –NH–CH2OH: hydroxymethyl group, –CH2–: methylene bridge, H2O: water.
The amino group binds to formaldehyde to form the hydroxymethyl group. Subsequently, the amino group binds to the hydroxymethyl group to form methylene bridge in protein and water. In the results, 2 hydrogens are extracted from the protein as water based on this chemical formula. The probability is that CNR of protein-rich tissue is decreased after formalin fixation by hydrogen extraction. In this study, CNRs of the tumor and muscularis propria were decreased after formalin fixation because this tissue is rich in protein. Conversely, CNR of the lipid-rich subserosa tissue was unchanged by formalin fixation.
There was no difference in error measurement of vertical tumor distance before and after formalin fixation. The chemical reaction of formalin is a molecular level crosslink (methylene bridge), which seems to influence little distance of the tumor and layers within the error range. The results of this study support previous studies reporting that maximum extramural depth measured by in vivo MRI accurately indicates the depth of rectal carcinoma invasion [10, 19].
Our study has some limitations. First, our study population was relatively small and seven lesions were excluded in vertical distance measurement because they could not be contained on one slide histopathologically due to their extremely large size, and it was difficult to correlate between MRI and histopathological image in vertical distance.
Second, the specimen was opened along the anterior rectum and on the side opposite the mesocolon of the colon immediately after resection, and the subserosa with the peritoneum was removed to harvest the lymph nodes according to pathology rules in our country. Consequently, opened specimens with the subserosa were examined before fixation and those without the subserosa were examined after fixation. Subserosal CNR could be measured because a small amount remained after removal, but the linear architecture of serosal fat tissue could not be evaluated on ex vivo MRI after fixation. Furthermore, T3 and T4 tumor could not be distinguished in this study because accurate correlation regarding the serosal invasion was impossible after removing the subserosa and peritoneum. To distinguish regarding T3 subgroups was impossible for the same reason.
In conclusion, the linear subserosal architecture represented fibrosis with tumoral invasion, known as desmoplastic reaction, which suggested T3–4 tumor. The submucosa and subserosa were of high intensity, and the mucosa and muscularis propria were of low intensity compared with the tumor before and after fixation though CNR of the tumor and muscularis propria decreased by formalin fixation. Ex vivo MRI both before and after fixation is available to correlate between ex vivo MRI and histopathology.
References
Torre LA, Bray F, Siegel RL, et al. (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108. https://doi.org/10.3322/caac.21262
Fraum TJ, Owen JW, Fowler KJ (2016) Beyond histologic staging: emerging imaging strategies in colorectal cancer with special focus on magnetic resonance imaging. Clin Colon Rectal Surg 29:205–215. https://doi.org/10.1055/s-0036-1584288
Puli SR, Bechtold ML, Reddy JBK, et al. (2009) How good is endoscopic ultrasound in differentiating various T stages of rectal cancer? Meta-analysis and systematic review. Ann Surg Oncol 16:254–265. https://doi.org/10.1245/s10434-008-0231-5
Shimura T, Ebi M, Yamada T, et al. (2014) Magnifying chromoendoscopy and endoscopic ultrasonography measure invasion depth of early stage colorectal cancer with equal accuracy on the basis of a prospective trial. Clin Gastroenterol Hepatol 12(662–668):e2. https://doi.org/10.1016/j.cgh.2013.06.022
Fu KI, Kato S, Sano Y, et al. (2008) Staging of early colorectal cancers: magnifying colonoscopy versus endoscopic ultrasonography for estimation of depth of invasion. Dig Dis Sci 53:1886–1892. https://doi.org/10.1007/s10620-007-0104-y
Mondal D, Betts M, Cunningham C, et al. (2014) How useful is endorectal ultrasound in the management of early rectal carcinoma? Int J Colorectal Dis 29:1101–1104. https://doi.org/10.1007/s00384-014-1920-0
Ahuja NK, Sauer BG, Wang AY, et al. (2015) Performance of endoscopic ultrasound in staging rectal adenocarcinoma appropriate for primary surgical resection. Clin Gastroenterol Hepatol 13:339–344. https://doi.org/10.1016/j.cgh.2014.07.013
Beets-Tan RGH, Lambregts DMJ, Maas M, et al. (2017) Magnetic resonance imaging for clinical management of rectal cancer: updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol . https://doi.org/10.1007/s00330-017-5026-2
Moreno CC, Sullivan PS, Kalb BT, et al. (2015) Magnetic resonance imaging of rectal cancer: staging and restaging evaluation. Abdom Imaging 40:2613–2629. https://doi.org/10.1007/s00261-015-0394-z
Group MS (2007) Extramural depth of tumor invasion at thin-section MR in patients with rectal cancer: results of the MERCURY study. Radiology 243:132–139. https://doi.org/10.1148/radiol.2431051825
Balyasnikova S, Brown G (2016) Imaging advances in colorectal cancer. Curr Colorectal Cancer Rep 12:162–169. https://doi.org/10.1007/s11888-016-0321-x
Deprisco G (2015) MRI local staging and restaging in rectal cancer. Clin Colon Rectal Surg 28:194–200. https://doi.org/10.1055/s-0035-1555010
Iafrate F, Laghi A, Paolantonio P, et al. (2006) Preoperative staging of rectal cancer with MR imaging: correlation with surgical and histopathologic findings. Radiographics 26:701–714. https://doi.org/10.1148/rg.263055086
Tudyka V, Blomqvist L, Beets-Tan RGH, et al. (2014) EURECCA consensus conference highlights about colon & rectal cancer multidisciplinary management: the radiology experts review. Eur J Surg Oncol 40:469–475
Inoue A, Ohta S, Nitta N, et al. (2016) MRI can be used to assess advanced T-stage colon carcinoma as well as rectal carcinoma. Jpn J Radiol 34:809–819. https://doi.org/10.1007/s11604-016-0591-x
Rollvén E, Holm T, Glimelius B, et al. (2013) Potentials of high resolution magnetic resonance imaging versus computed tomography for preoperative local staging of colon cancer. Acta Radiol 54:722–730. https://doi.org/10.1177/0284185113484018
Nerad E, Lambregts DMJ, Kersten ELJ, et al. (2017) MRI for local staging of colon cancer. Dis Colon Rectum 60:385–392. https://doi.org/10.1097/DCR.0000000000000794
Hunter C, Blake H, Jeyadevan N, et al. (2016) Local staging and assessment of colon cancer with 1.5-T magnetic resonance imaging. Br J Radiol . https://doi.org/10.1259/bjr.20160257
Brown G, Richards CJ, Newcombe RG, et al. (1999) Rectal carcinoma: thin-section MR imaging for staging in 28 patients. Radiology 211:215–222. https://doi.org/10.1148/radiology.211.1.r99ap35215
Yamada I, Okabe S, Enomoto M, et al. (2008) Colorectal carcinoma. in vitro evaluation with high-spatial- resolution 3d constructive interference in steady-state MR imaging. Radiology 246:444–453
Yamada I, Yoshino N, Tetsumura A, et al. (2009) Colorectal carcinoma: local tumor staging and assessment of lymph node metastasis by high-resolution MR imaging in surgical specimens. Int J Biomed Imaging . https://doi.org/10.1155/2009/659836
Imai Y, Kressel HY, Saul SH, et al. (1990) Colorectal tumors: an in vitro study of high-resolution MR imaging. Radiology 177:695–701. https://doi.org/10.1148/radiology.177.3.2243971
Allen M, Jones JL (2011) Jekyll and Hyde: the role of the microenvironment on the progression of cancer. J Pathol 223:162–176. https://doi.org/10.1002/path.2803
McAllister SS, Weinberg RA (2010) Tumor-host interactions: a far-reaching relationship. J Clin Oncol 28:4022–4028. https://doi.org/10.1200/JCO.2010.28.4257
Brown G, Richards CJ, Bourne MW, et al. (2003) Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology 227:371–377. https://doi.org/10.1148/radiol.2272011747
Beets-Tan RGH, Beets GL, Vliegen RF, et al. (2001) Accuracy of magnetic resonance imaging in prediction of tumour-free resection margin in rectal cancer surgery. Lancet 357:497–504. https://doi.org/10.1016/j.micinf.2011.07.011.Innate
Yamada I, Yoshino N, Hikishima K, et al. (2017) Colorectal carcinoma: ex vivo evaluation using 3-T high-spatial-resolution quantitative T2 mapping and its correlation with histopathologic findings. Magn Reson Imaging 38:174–181. https://doi.org/10.1016/j.mri.2016.12.028
Howat WJ, Wilson BA (2014) Tissue fixation and the effect of molecular fixatives on downstream staining procedures. Methods 70:12–19. https://doi.org/10.1016/j.ymeth.2014.01.022
Singhal P, Singh NN, Sreedhar G, et al. (2016) Evaluation of histomorphometric changes in tissue architecture in relation to alteration in fixation protocol—an invitro study. J Clin Diagnostic Res 10:ZC28–ZC32. https://doi.org/10.7860/jcdr/2016/19007.8236
Özkan N, Şalva E, Çakalağaoğlu F, Tüzüner B (2012) Honey as a substitute for formalin? Biotech Histochem 87:148–153. https://doi.org/10.3109/10520295.2011.590155
Acknowledgments
The authors would like to thank Hitoshi Saeki (Department of pathology, Higashi-Ohmi General Medical Center) for scanning histopathological images and Enago (www.enago.jp) for the English language review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest was reported by the authors.
Rights and permissions
About this article
Cite this article
Inoue, A., Ohta, S., Nitta, N. et al. Ex vivo MR imaging of colorectal carcinoma before and after formalin fixation: correlation with histopathologic findings. Abdom Radiol 43, 1524–1530 (2018). https://doi.org/10.1007/s00261-018-1538-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1538-8