Abstract
Purpose
To evaluate the feasibility of assessing advanced T-stage (T3–T4) colorectal carcinomas by correlating MRI with histopathological findings.
Materials and methods
The study population comprised 31 patients with 32 lesions (22 colon and 10 rectal carcinomas). The relationship between the tumor and bowel layers on T2- and contrast-enhanced T1-weighted images (T2WI, CE-T1WI), bowel wall deformity, and the linear architecture of subserosal fat on T2WI scans was independently assessed by two radiologists. Diagnostic ability and interobserver agreement were evaluated using Fisher’s exact test and kappa statistics, respectively.
Results
The sensitivity/specificity for disrupting the outer layer on T2WI scans for the differentiation between Tis–T2 and T3–T4 colorectal carcinoma was 100/75 % (p < 0.05) for both observers; on CE-T1WI, it was 88.0/50 % (p = 0.13) for one and 96.0/50 % (p = 0.11) for the other. The sensitivity/specificity for recognizing the reticulated linear architecture to distinguish T3 from T4 colon carcinoma was 83.3/84.6 % (p < 0.05) for one reader and 100/92.3 % (p < 0.05) for the other reader.
Conclusion
Disruption of the outer low-intensity layer on T2WI scans was the most important finding for the diagnosis of T3–T4 colorectal carcinoma. The reticulated linear architecture of the fat tissue was suggestive of T4 colon carcinoma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 2012, an estimated 1.4 million patients presented with colorectal carcinoma, and 693,900 (49.6 %) died of the disease [1]. To improve the prognosis of patients with rectal cancer, the T-, N-, and M-stage must be known [2]. Endoscopic ultrasound (EUS) differentiates accurately between T1 and T2 and between T2 and T3 colorectal carcinomas [3, 4]. In patients with T3–T4 rectal carcinoma, magnetic resonance imaging (MRI) yields better results than EUS. Matsuoka et al. [5] reported that computed tomography (CT) and MRI studies were of equal usefulness for the local staging of rectal carcinoma. However, according to Beets-Tan et al. [6], MRI was highly accurate and superior to CT for predicting rectal tumor infiltration into surrounding structures. Others [7–9] have found that in patients with rectal carcinoma, MRI accurately assesses the extramural depth of tumor invasion and predicts clear surgical resection margins. Therefore, MRI is the accepted modality for predicting the surgical margin, for the indication of neoadjuvant therapy, and for the response assessment in patients with rectal carcinoma [10–14]; like EUS, it can be used for the evaluation of locally advanced colon cancer [15].
The T-stage of colon cancer dictates the surgical treatment of the primary lesion. Kotake et al. [16] treated T1–T2 colon cancer by D2 resection (standard low tie) and T3–T4 lesions by D3 resection (high tie). They reported that D3 resection with extended lymphadenectomy was life prolonging. Combined resection should be performed to address T4 colon cancers with adhesion or invasion to adjacent organs. In their phase II trial, Jakobsen et al. [15] found that neoadjuvant chemotherapy was effective in patients with locally advanced colon cancer. Therefore, the T-stage of colon and rectal cancers is important to reach appropriate treatment decisions.
While CT is commonly used for the T-staging of colon cancers, the T-staging ability of MRI requires closer evaluation. Rollvén et al. [17], suggested that MRI is superior to CT studies for the T-staging of colon cancer because their high soft-tissue discrimination yields information on extramural venous invasion.
We performed a prospective study of the ability of MRI to correctly T-stage 22 colon and 10 rectal cancers. We used the T-stage indicated by histopathological findings as the reference standard and compared it with the T-stage determined by MRI studies.
Materials and methods
Patients
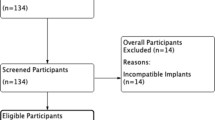
This prospective study was approved by our institutional review board; prior informed consent for participation was obtained from all of the patients.
Between November 2013 and September 2014, 45 consecutive patients with 48 colon or rectal cancers underwent surgery at our institution. We excluded 14 patients with 16 lesions because MRI-related preoperative clipping to mark the resection site was contraindicated.
Consequently, we enrolled 31 patients with 32 lesions (15 males and 16 females; mean age: 70.1 years; age range: 53–89 years). Of the 32 lesions, 5 were located in the ascending colon, 5 in the transverse colon, 1 in the descending colon, and 11 in the sigmoid colon; 10 were rectal lesions. While all patients underwent MRI studies, 3 patients with bronchial asthma could not undergo multiphase contrast-enhanced T1-weighted images (CE-T1WI). Therefore, we evaluated the CE-T1WI scans of 28 patients with 29 lesions. In one patient, the cancer was intraoperatively diagnosed as T4; the operation was palliative, and the cancer was not resected. Three patients with advanced lower rectal carcinoma underwent neoadjuvant chemotherapy.
Imaging technique
MRI studies were performed 2 or 3 days before the operation. Scopolamine butylbromide (20 mg; Buscopan, Boehringer Ingelheim Japan, Tokyo, Japan) was injected intravenously to suppress peristalsis. No bowel preparation was performed.
MRI studies were on a 3 T MR system (SIGNA HDxt Optimal Edition; GE Healthcare, Milwaukee, WI) using an 8-channel HD cardiac array coil (GE Healthcare). The scan timing for multiphase CE-T1WI was 40, 80, 120, and 200 s after the administration of gadopentetate dimeglumine (0.2 ml/kg, 2 ml/sec, Magnevist, Bayer Yakuhin Ltd., Osaka, Japan).
T-stage-based treatment
Based on the recommendations of The Japanese Society for Cancer of the Colon and Rectum, the primary T1–T2 tumors were addressed by D2 resection and T3–T4 tumors by D3 resection. The combined resection of adjacent organs was performed for tumors with adhesion (T3) or invasion (T4) to adjacent organs. Three patients with advanced lower rectal carcinoma (T3–T4) received neoadjuvant chemotherapy.
Pathological study
All of the specimens were cut axially and longitudinally through the center, embedded in paraffin, cut into thin sections, and stained with hematoxylin and eosin. A pathologist (R.K.) with 30 years of experience recorded the T-stage of all resected specimens histopathologically as Tis (limited to the mucosa), T1 (invading the submucosa), T2 (invading the muscularis propria), T3 (extending into the subserosa), and T4 (involving the serous membrane or adjacent organs). When invasion into the adjacent organs was observed intraoperatively without pathological confirmation of such invasion, adhesion to adjacent organs was recorded.
Image analysis
All of the images were reviewed by two radiologists (N.N. and S.O.) with 27 and 21 years of experience reading gastrointestinal images, respectively. They knew the purpose of the study and the location of the cancers but were blinded to the information on the T-stage of the disease. They assessed the MRI scans independently. The MRI findings were recorded for all patients and lesions. This process involved the following 4 steps.
-
Step 1 The readers reviewed the number of visible normal bowel layers near the tumor on T2WI- and CE-T1WI scans (Fig. 1). The times to peak enhancement (40, 80, 120, 200 s) on CE-T1WI were also recorded.
Fig. 1 Reference images of visible normal bowel layers in patients with rectal (a) and colon (b–d) cancer. a T2WI: Three layers (1: low-intensity-, 2: high-intensity-, 3: low-intensity) are observed in the rectum. b T2WI: Two layers (1: high-intensity, 2: low-intensity) are seen in the descending colon. The high-intensity area in the lumen is mucus (m). c CE-T1WI (40 s): Two layers (1: high-intensity, 2: low-intensity) are noted in the sigmoid colon. d CE-T1WI (40 s): Only one layer is observed in the transverse colon. Parameter for T2WI: TR 2500 ms, TE 80 ms, FOV 240 mm, matrix 512 × 512 mm, slice thickness 3.0 mm. Parameters for multiphase CE-T1WI: TR 6.4 ms, TE 1.7 ms, FOV 240 mm, matrix 512 × 512 mm, slice thickness 1.5 mm
-
Step 2 The status of the outer layer was evaluated on T2WI and CE-T1WI scans. Others [18, 19] based the staging on MRI scans on differences in signal intensity; T1 carcinomas are confined to the mucosa and submucosa (high-intensity layer), T2 tumors invade the muscularis propria (low-intensity layer), and T3 lesions extend beyond. We classified the tumors as manifesting (a) the integrity of the outer low-intensity layer, (b) disruption of the outer layer with no contact with the serosal membrane/adjacent organs, and (c) disruption of the outer layer with contact with the serosal membrane/adjacent organs (Fig. 2). To distinguish Tis–T2 from T3–T4, we defined tumors with the integrity of the outer layer as Tis–T2 and tumors manifesting disruption of the outer layer as T3–T4. Tumors without and with contact with the serosal membrane or adjacent organs were recorded as T3 and T4, respectively.
Fig. 2 Reference images of the relationship between the tumor and bowel layers on T2WI (a–c) and CE-T1WI (d–f) scans. T2WI (a) and CE-T1WI (d): The integrity of outer layer (arrow) is depicted. T2WI (b) and CE-T1WI (e): The outer layer (arrow) is disrupted. T2WI (c) and CE-T1WI (f): The tumor contacts the left ovary (O)
-
Step 3 Deformity of the bowel wall was evaluated on T2WI scans and was classified as flat, concave, or convex (Figs. 3, 4). When the bowel wall appeared flat, we recorded the tumor as Tis–T2; when its shape was deformed (concave or convex), the tumor was classified as T3–T4. A concave bowel wall appearance was recorded as T3, and a convex shape as T4 to distinguish T3 from T4.
Fig. 3 Schematic illustration of the deformity of the bowel wall and of the linear architecture. a Concave deformity: The tumor does not cross the estimated bowel wall line (black broken line). b Convex deformity: The tumor extends beyond the estimated bowel wall line (white broken line). c Spiculated linear architecture: The linear low intensity area in the mesocolon is concentrated on the tumor surface. d Reticulated linear architecture: The linear low intensity area in the mesocolon is distributed in various directions
Fig. 4 Reference images of bowel wall deformity and of the linear architecture of fat tissue. a Neither deformity of the bowel wall nor a linear architecture of fat tissue around the tumor (asterisk) is observed. b Concave bowel wall deformity (arrow head) and a spiculated linear architecture of the fat (arrow) are present around the tumor (asterisk). c Convex bowel wall deformity (arrow head) and a spiculated linear architecture of the fat (arrow) are observed around the tumor (asterisk). d Convex bowel wall deformity (arrow head) and a reticulated linear architecture of the fat (arrow) are observed around the tumor (asterisk)
-
Step 4 The linear architecture of the fat was evaluated on T2WI scans and was classified as absent, exhibiting a spiculated architecture, which is defined by the convergence of the linear architecture and tumor, and as manifesting a reticulated architecture, which is defined as the distribution of the linear architecture in an irregular pattern (Figs. 3, 4). To distinguish Tis–T2 from T3–T4, the absence and presence of a linear architecture was recorded as Tis–T2 and T3–T4, respectively. To distinguish T3 from T4, tumors with spiculation were designated as T3, and tumors with reticulation were classified as T4.
The results of radiological and pathological T-staging were compared by a radiologist (A.I.) who determined the radiological-histological correlation at the center of surgical specimens cut axially and longitudinally.
Statistical analysis
The number of visible layers observed in step 1 was classified based on their location (transverse colon ascending and descending colon, sigmoid colon, and rectum). We compared the findings made at the different locations using Tukey’s test. The number of specific MRI findings obtained in steps 2–4 was recorded. The sensitivity and specificity for distinguishing Tis–T2 from T3–T4 colorectal carcinoma, and T3 from T4 colon carcinoma were determined by recording the disruption of the outer layer and contact with the serosal membrane and adjacent organs on T2WI and CE-T1WI scans, deformity of the bowel wall, and linear architecture of the fat. These findings were assessed using Fisher’s exact test. p values of 0.05 or less were considered to indicate a statistically significant difference. Interobserver agreement was compared using kappa statistics and was categorized as poor (<0.20), fair (0.21–0.40), moderate (0.41–0.60), good (0.61–0.80), and very good (0.81–1.00). Statistical tests were performed using SPSS statistics 22 (IBM, Chicago, IL).
Results
Histopathological diagnosis
The histopathological T-staging of colon and rectal carcinomas is shown in Table 1.
Step-wise correlation of MRI and histopathological findings
As two lesions, one T1 and the other T2, were not depicted by MRI, 30 were available for study. Table 2 shows the interobserver agreement for colon and rectal carcinomas, and Table 3 shows the sensitivity, specificity and p values recorded for the two observers. These parameters were not evaluated for the differentiation between T3 and T4 rectal cancer because our study included no T4 rectal cancers.
-
Step 1 Table 4 lists the number of visible normal bowel layers near the tumor on T2WI and CE-T1WI scans assessed by the two observers. Both T2WI and CE-T1WI scans tended to depict more layers in the large intestine of the lower abdomen such as the sigmoid colon and rectum than in the large intestine of the upper abdomen, especially the transverse colon. The outer layer representing the muscularis propria was depicted on both T2WI and CE-T1WI scans of the large bowel of all subjects. The time to peak enhancement was 40 s in 22 (75.9 %) and 80 s in 7 (24.1 %) of 29 lesions.
-
Step 2 T2WI scans were superior to CE-T1WI scans with respect to the sensitivity and specificity for determining the status of the outer layer for the differentiation of Tis–T2 from T3–T4 and of T3 from T4 colon carcinoma. As shown in Table 3, on T2WI scans, there were statistically significant differences between colorectal and colon carcinomas. Interobserver agreement for colon carcinoma was very good for T2WI and better for CE-T1WI scans (κ = 0.81 vs. κ = 0.49) (Table 2).
-
Step 3 Bowel wall deformity was identified by one observer in 16 and by the other in 17 of 19 T3–T4 colon carcinomas; both readers recorded wall convexity in 5 of 6 T4 colon cancers (Table 3). There was no significant difference in their distinguishing Tis–T2 from T3–T4 and T3 from T4 cancers; interobserver agreement was fair (κ = 0.35).
-
Step 4 One observer identified a linear architecture in 16 and the other in 17 of 19 T3–T4 colon carcinomas; of 6 T4 colon cancers, 5 were recorded as exhibiting a reticulated linear architecture by one reader; the other observed this structure in all 6 of these lesions. Reticulation was reported in 2 of 3 patients with T3 lower rectal cancers who had undergone neoadjuvant chemotherapy. The reticulated linear architecture was useful only for distinguishing between T3 and T4 colon cancer. Interobserver agreement was good (κ = 0.69).
T-stage-based treatment
One T2 rectal carcinoma was over-diagnosed as a T3 tumor; this patient underwent extended lymphadenectomy, including lateral lymph node (D3) resection. Three T3 colon carcinomas were over-diagnosed as T4 tumors because T2WI showed invasion into the serosa (n = 1), small intestine (n = 1) and colon (n = 1); these patients were treated by combined resection of the serosa or adhering organ. An example is presented in Fig. 5.
A 77-year-old male with sigmoid colon carcinoma adhering to the small bowel (T3). C cancer, S small bowel. a On the T2WI scan, the cancer is in extensive contact with the small intestine. b Hematoxylin-eosin staining showed fibrosis and inflammation between the cancer and small bowel. The broken line indicates the demarcation of the carcinoma
Discussion
We studied the correlation between the imaging features of T3 and T4 colon and rectal cancers and their histopathology. According to earlier ex vivo MRI studies, the 1st (low-intensity) layer is the mucosa, the 2nd (high-intensity) layer is the submucosa, and the 3rd (low-intensity) layer is the muscularis propria; the fat (high-intensity) layer is the subserosa [20–22]. For a diagnosis of tumor extension beyond the bowel wall (T3–T4), the status of the muscularis propria must be known. As the muscularis propria could be observed on T2WI and CE-T1WI scans of all colon and rectal cancers, we used its disruption to define T3–T4 carcinomas. Earlier studies reported that the accuracy of the T-staging of rectal carcinoma on T2WI scans acquired with phased-array coils was 65–95.8 % [19, 23–28]. We found that T2WI detected extramural spread not only in rectal- (T3–T4) but also in colon carcinomas (T3–T4). Disruption of the outer low-intensity layer on T2WI scans is the most reliable feature for the detection of extramural spread.
For the detection of extramural tumor spread, T2WI was superior to CE-T1WI. Interobserver agreement was better for T2WI than CE-T1WI scans of both colon and rectal cancers. The discrepancies of two readers were seen between the disruption of the outer layer (T3) and contact with the serosal membrane or adjacent organs (T4) on T2WI. Conversely, discrepancies have been shown not only between T3 and T4 but also with the integrity of the outer layer (T2) and disruption of the outer layer (T3) on CE-T1WI. Vliegen et al. [29] reported that CE-T1WI did not improve the diagnostic accuracy for the local assessment of rectal carcinoma, and Gollub et al. [30] found that the use of contrast medium for rectal MRI did not significantly improve the readers’ agreement or their ability to detect T4 carcinomas. We believe that with respect to the T-staging of colon cancers, the administration of contrast medium is not necessary.
Bowel wall deformity was present primarily in T3–T4 colorectal cancer. Interobserver agreement for the presence of bowel wall deformity in patients with colon carcinoma was fair. This was speculated as follows: the results of bowel wall deformity were susceptible to the differences in the focus point of the tumors by each reader.
The most abundant mesenchymal cells—i.e., fibroblasts and myofibroblasts—in carcinomatous masses promote tumor progression; histopathologically, this is known as a desmoplastic reaction [31, 32]. A linear architecture of the fat on MRI scans is indicative of this reaction in rectal carcinoma [33]. According to Brown et al. [19], spiculation into perirectal fat is indicative of a T2 tumor; we observed a spiculated linear architecture in one of two T2 rectal carcinomas. Conversely, Beets-Tan et al. [12] reported that pre-treatment spiculation into perirectal fat predicted a T3 tumor.
We observed no significant difference in spiculation between lower- and higher-stage colon cancers. However, the incidence of a reticulated architecture was significantly higher in T4 colon carcinomas than in T3 tumors. We noted spiculation indicative of a desmoplastic reaction in the advanced portion of carcinomas with mild subserosal invasion, and a reticulated pattern reflective of a multidirectional desmoplastic reaction in the fat of patients with severe invasion into the subserosa and adjacent organs. Therefore, we propose that a linear architecture should be considered as a secondary finding suggestive of T3–T4 tumors, while reticulation should alert to T4 lesions. The interobserver disagreement was seen between speculation and reticulation because the subtle direction of the linear architecture was difficult to interpret.
Quaia et al. [34] reported that the linear and reticular strands reaching the mesorectal fascia on CE-MRI scans were predictive of invasion into the mesorectal fascia after neoadjuvant therapy. We observed a reticulated linear architecture in 2 of 3 lower rectal carcinomas subjected to neoadjuvant chemotherapy; they were diagnosed as T3 tumors without invasion into the mesorectal fascia. Therefore, a linear architecture must be evaluated carefully to avoid over-diagnosing patients who had undergone neoadjuvant chemotherapy.
For the clinical differentiation between stage T3 and T4 colon carcinomas, we defined tumors in contact with adjacent organs on T2WI scans as T4 tumors. Consequently, based on our definition, three T3 colon tumors were over-diagnosed as T4 because it was difficult to distinguish invasion into from adhesion to adjacent organs. In addition to the findings of contact with the serosal membrane or adjacent organs, additional observations such as a reticulated linear architecture may suggest a T4 tumor, and combined resection is generally performed in the presence of preoperative MRI evidence of either adhesion to or invasion into adjacent organs.
More layers were depicted in the large intestine of the lower abdomen on both T2WI and CE-T1WI scans. This may be attributable to motion artifacts due to respiratory movement and heart beats; they lower the quality of images of the upper abdomen (the transverse, ascending, and descending colon). Additionally, the large intestine of the lower abdomen (the sigmoid colon and rectum) tended to be contracted in our study. As a collapsed bowel helps to assess the bowel layers and depth of tumor invasion, earlier MRI studies in patients with rectal cancer were performed without bowel dilation [19, 23–26]. We chose the muscularis propria for T-staging because it was depicted on all images. In the presence of bowel wall distension, we over-diagnosed one T2 rectal tumor because the outer low-intensity layer (muscularis propria) was disrupted on T2WI scan. Based on our findings, we suggest that MRI can be used to identify T3–T4 colon cancer in any part of the abdomen, but especially in the sigmoid colon.
Although our results demonstrated that MRI is highly reliable for detecting the extramural spread of colon cancer, its diagnostic accuracy vis-a-vis CT in the same patient remains unclear. CT studies to assess the T-stage detected extramural spread (T3) in 47.5–80 % of colon carcinomas [35]. In their meta-analysis, Dighe et al. [36] found that preoperative staging on multi-detector CT scans was highly accurate in patients with T3–T4 colon cancer. As CT is fast and low-cost and can be used to assess metastatic lesions, it is an essential modality for the preoperative staging of colon cancers. However, CT involves radiation exposure and an iodine contrast medium that is contraindicated in patients with asthma or impaired renal function and must be injected for the T-staging of colon cancers. Our findings indicate that MRI is an alternative in such patients and an additional modality for the T-staging of colon cancers in whose presence it is difficult to rule in/rule out extramural spread and invasion into the serosa/adjacent organs on CT scans.
Our study has some limitations. First, our study population was relatively small because our investigation was prospective and funds were limited, and we focused on patients scheduled for colon or rectal cancer surgery. Consequently, it included 25 patients with T3–T4 tumors and only four patients with Tis–T2 tumors. The reticulated linear architecture of the fat tissue was suggestive of the involvement of the serosa or adjacent organ in the colon carcinoma, but this study included no patient with T4 rectal carcinoma.
Second, we did not perform N- and M-staging because our MRI studies focused on the primary lesion in a narrow field of view; additional sequences or modalities are required for N- and M-staging. Moreover, in compliance with Japanese pathology rules, the mesocolon and lymph nodes were removed before specimen fixation.
Third, it remains unclear whether MRI is helpful for assessing the advisability of endoscopic treatment in patients with early colon or rectal cancer. As 2 colon cancers, one T1 and the other T2, were not depicted on MRI scans, this modality may not be useful for assessing lower-stage colon cancers. Because MR colonoscopy does not involve ionizing radiation and is highly sensitive and specific for the diagnosis of colonic lesions measuring at least 10 mm [37], it may be useful for the detection of early colorectal carcinomas.
In conclusion, MRI can be used to assess T3–T4 colon cancer. Disruption of the outer low-intensity layer representing the muscularis propria on T2WI scans was the most important finding for a diagnosis of T3–T4 colon carcinoma. A reticulated linear architecture of the fat tissue is suggestive of involvement of the serosa or other organs (T4).
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
Tapan U, Ozbayrak M, Tatlı S. MRI in local staging of rectal cancer: an update. Diagn Interv Radiol (Ank). 2014;20(5):390–8.
Shimura T, Ebi M, Yamada T, Hirata Y, Nishiwaki H, Mizushima T, et al. Magnifying chromoendoscopy and endoscopic ultrasonography measure invasion depth of early stage colorectal cancer with equal accuracy on the basis of a prospective trial. Clin Gastroenterol Hepatol. 2014;12(4):662–8.
Fu KI, Kato S, Sano Y, Onuma EK, Saito Y, Matsuda T, et al. Staging of early colorectalcancers: magnifying colonoscopy versus endoscopic ultrasonography for estimation of depth of invasion. Dig Dis Sci. 2008;53(7):1886–92.
Matsuoka H, Nakamura A, Masaki T, Sugiyama M, Takahara T, Hachiya J, et al. A prospective comparison between multidetector-row computed tomography and magnetic resonance imaging in the preoperative evaluation of rectal carcinoma. Am J Surg. 2003;185(6):556–9.
Beets-Tan RG, Beets GL, Borstlap AC, Oei TK, Teune TM, von Meyenfeldt MF, et al. Preoperative assessment of local tumor extent in advanced rectal cancer: CT or high-resolution MRI? Abdom Imaging. 2000;25(5):533–41.
Group MS. Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. BMJ. 2006;333(7572):779.
Salerno G, Daniels IR, Moran BJ, Wotherspoon A, Brown G. Clarifying margins in the multidisciplinary management of rectal cancer: the MERCURY experience. Clin Radiol. 2006;61(11):916–23.
Group MS. Extramural depth of tumor invasion at thin-section MR in patients with rectal cancer: results of the MERCURY study. Radiology. 2007;243(1):132–9.
Hötker AM, Garcia-Aguilar J, Gollub MJ. Multiparametric MRI of rectal cancer in the assessment of response to therapy: a systematic review. Dis Colon Rectum. 2014;57(6):790–9.
Zhao RS, Wang H, Zhou ZY, Zhou Q, Mulholland MW. Restaging of locally advanced rectal cancer with magnetic resonance imaging and endoluminal ultrasound after preoperative chemoradiotherapy: a systemic review and meta-analysis. Dis Colon Rectum. 2014;57(3):388–95.
Beets-Tan RG, Beets GL, Vliegen RF, Kessels AG, Van Boven H, De Bruine A, et al. Accuracy of magnetic resonance imaging in prediction of tumour-free resection margin in rectal cancer surgery. Lancet. 2001;357(9255):497–504.
Taylor FG, Quirke P, Heald RJ, Moran BJ, Blomqvist L, Swift IR, et al. Preoperative magnetic resonance imaging assessment of circumferential resection margin predicts disease-free survival and local recurrence: 5-year follow-up results of the MERCURY study. J Clin Oncol. 2014;32(1):34–43.
Patel UB, Taylor F, Blomqvist L, George C, Evans H, Tekkis P, et al. Magnetic resonance imaging-detected tumor response for locally advanced rectal cancer predicts survival outcomes: MERCURY experience. J Clin Oncol. 2011;29(28):3753–60.
Jakobsen A, Andersen F, Fischer A, Jensen LH, Jørgensen JC, Larsen O, et al. Neoadjuvant chemotherapy in locally advanced colon cancer. A phase II trial. Acta Oncol. 2015;54(10):1747–53.
Kotake K, Mizuguchi T, Moritani K, Wada O, Ozawa H, Oki I, et al. Impact of D3 lymph node dissection on survival for patients with T3 and T4 colon cancer. Int J Colorectal Dis. 2014;29(7):847–52.
Rollvén E, Holm T, Glimelius B, Lörinc E, Blomqvist L. Potentials of high resolution magnetic resonance imaging versus computed tomography for preoperative local staging of colon cancer. Acta Radiol. 2013;54(7):722–30.
Nougaret S, Reinhold C, Mikhael HW, Rouanet P, Bibeau F, Brown G. The use of MR imaging in treatment planning for patients with rectal carcinoma: Have you checked the “DISTANCE”? Radiology. 2013;268(2):330–44.
Brown G, Richards CJ, Newcombe RG, Dallimore NS, Radcliffe AG, Carey DP, et al. Rectal carcinoma: thin-section MR imaging for staging in 28 patients. Radiology. 1999;211(1):215–22.
Imai Y, Kressel HY, Saul SH, Chao PW, Schnall MD, Lenkinski RE, et al. Colorectal tumors: an in vitro study of high-resolution MR imaging. Radiology. 1990;177(3):695–701.
Yamada I, Okabe S, Enomoto M, Sugihara K, Yoshino N, Tetsumura A, et al. Colorectal carcinoma: in vitro evaluation with high-spatial-resolution 3D constructive interference in steady-state MR imaging. Radiology. 2008;246(2):444–53.
Yamada I, Yoshino N, Tetsumura A, Okabe S, Enomoto M, Sugihara K, et al. Colorectal carcinoma: local tumor staging and assessment of lymph node metastasis by high-resolution MR imaging in surgical specimens. Int J Biomed Imaging. 2009;2009:659836.
Algebally AM, Mohey N, Szmigielski W, Yousef RR, Kohla S. The value of high-resolution MRI technique in patients with rectal carcinoma: pre-operative assessment of mesorectal fascia involvement, circumferential resection margin and local staging. Pol J Radiol. 2015;80:115–21.
Winter L, Bruhn H, Langrehr J, Neuhaus P, Felix R, Hänninen LE. Magnetic resonance imaging in suspected rectal cancer: determining tumor localization, stage, and sphincter-saving resectability at 3-Tesla-sustained high resolution. Acta Radiol. 2007;48(4):379–87.
Park JS, Jang YJ, Choi GS, Park SY, Kim HJ, Kang H, et al. Accuracy of preoperative MRI in predicting pathology stage in rectal cancers: node-for-node matched histopathology validation of MRI features. Dis Colon Rectum. 2014;57(1):32–8.
Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM, Stoker J. Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging––a meta-analysis. Radiology. 2004;232(3):773–83.
Gowdra Halappa V, Corona Villalobos CP, Bonekamp S, Gearhart SL, Efron J, Herman J, et al. Rectal imaging: part 1. High-resolution MRI of carcinoma of the rectum at 3 T. AJR Am J Roentgenol. 2012;199(1):W35–42.
Jhaveri KS, Hosseini-Nik H. MRI of rectal cancer: an overview and update on recent advances. AJR Am J Roentgenol. 2015;205(1):W42–55.
Vliegen RF, Beets GL, von Meyenfeldt MF, Kessels AG, Lemaire EE, van Engelshoven JM, et al. Rectal cancer: MR imaging in local staging––Is gadolinium-based contrast material helpful? Radiology. 2005;234(1):179–88.
Gollub MJ, Lakhman Y, McGinty K, Weiser MR, Sohn M, Zheng J, et al. Does gadolinium-based contrast material improve diagnostic accuracy of local invasion in rectal cancer MRI? A multireader study. AJR Am J Roentgenol. 2015;204(2):W160–7.
McAllister SS, Weinberg RA. Tumor-host interactions: a far-reaching relationship. J Clin Oncol. 2010;28(26):4022–8.
Allen M, Louise Jones J. Jekyll and Hyde: the role of the microenvironment on the progression of cancer. J Pathol. 2011;223(2):162–76.
Iafrate F, Laghi A, Paolantonio P, Rengo M, Mercantini P, Ferri M, et al. Preoperative staging of rectal cancer with MR imaging: correlation with surgical and histopathologic findings. Radiographics. 2006;26(3):701–14.
Quaia E, Gennari AG, De Paoli L, Angileri R, Ukmar M, Cova MA. Predictors of mesorectal fascia invasion after gadolinium injection in rectal carcinoma after neoadjuvant therapy. Clin Imaging. 2014;38(5):698–703.
Dighe S, Swift I, Brown G. CT staging of colon cancer. Clin Radiol. 2008;63(12):1372–9.
Dighe S, Purkayastha S, Swift I, Tekkis PP, Darzi A, A’Hern R, et al. Diagnostic precision of CT in local staging of colon cancers: a meta-analysis. Clin Radiol. 2010;65(9):708–19.
Zijta FM, Bipat S, Stoker J. Magnetic resonance (MR) colonography in the detection of colorectal lesions: a systematic review of prospective studies. Eur Radiol. 2010;20(5):1031–46.
Acknowledgments
This study was funded by Bayer Yakuhin Ltd. The study data was independently analyzed and interpreted form the funder.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict interest of interest to disclose with respect to this article.
Ethical statement
This prospective study was approved by our institutional review board; prior informed consent for participation was obtained from all patients.
About this article
Cite this article
Inoue, A., Ohta, S., Nitta, N. et al. MRI can be used to assess advanced T-stage colon carcinoma as well as rectal carcinoma. Jpn J Radiol 34, 809–819 (2016). https://doi.org/10.1007/s11604-016-0591-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-016-0591-x