Abstract
Purpose
18F-Fluciclovine PET imaging has been increasingly used in the restaging of prostate cancer patients with biochemical recurrence (BCR); however, its clinical utility in patients with low prostate-specific antigen (PSA) levels following primary radiation therapy has not been well-studied. This study aims to determine the detection rate and diagnostic accuracy of 18F-fluciclovine PET and the patterns of prostate cancer recurrence in patients with rising PSA after initial radiation therapy, particularly in patients with PSA levels below the accepted Phoenix definition of BCR (PSA nadir +2 ng/mL).
Methods
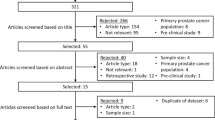
This retrospective study included patients from two tertiary institutions who underwent 18F-fluciclovine PET scans for elevated PSA level following initial external beam radiation therapy, brachytherapy, and/or proton therapy. Logistic regression and receiver operating characteristic (ROC) curve analyses were performed to determine the diagnostic accuracy of 18F-fluciclovine PET and associations of PSA kinetic parameters with 18F-fluciclovine PET outcome.
Results
One hundred patients were included in this study. The overall detection rate on a patient-level was 79% (79/100). 18F-Fluciclovine PET was positive in 62% (23/37) of cases with PSA below the Phoenix criteria. The positive predictive value of 18F-fluciclovine PET was 89% (95% CI: 80–94%). In patients with PSA below the Phoenix criteria, the PSA velocity had the highest predictive value of 18F-fluciclovine PET outcome. PSA doubling time (PSADT) and PSA velocity were associated with the presence of extra-pelvic metastatic disease.
Conclusion
18F-Fluciclovine PET can identify recurrent disease at low PSA level and PSA rise below accepted Phoenix criteria in patients with suspected BCR after primary radiation therapy, particularly in patients with low PSADT or high PSA velocity. In patients with low PSADT or high PSA velocity, there is an increased probability of extra-pelvic metastases. Therefore, these patients are more likely to benefit from PET/CT or PET/MRI than pelvic MRI alone.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the most prevalent noncutaneous malignancy in men and the second leading cause of cancer death among men in the USA [1]. Initial definitive radiation therapy is the cornerstone of treatment in 23% of patients aged 65 years or younger and 36% of those older than 65 [2]. Despite advancements in radiation therapy, 23–43% of patients with intermediate or high-risk cancer develop biochemical recurrence (BCR) [3]. BCR for patients who received definitive external beam radiation therapy (EBRT) or brachytherapy is defined based on the Phoenix Conference Consensus of RTOG-ASTRO (Radiation Therapy Oncology Group-American Society for Therapeutic Radiology and Oncology) [4]. According to the Phoenix Conference Consensus, BCR is defined as posttreatment PSA rising to 2.0 ng/mL above the lowest posttreatment value (nadir) after radiation therapy with or without hormone therapy. The NCCN guideline recommends recurrence evaluation in patients with rising PSA below the Phoenix criteria, particularly in men with a rapid increase of PSA or healthier candidates who may be eligible for salvage local therapy [4].
The synthetic amino acid anti-1-amino-3-[18F]-flurocyclobutane-1-carboxylic acid (18F-FACBC, 18F-fluciclovine, Axumin) is a widely available FDA-approved positron emission tomography (PET) radiotracer for localization of biochemically recurrent prostate cancer. There have been a number of studies investigating the role of 18F-fluciclovine PET in the staging of patients with prostate cancer [5]. However, these studies have either focused on patients before [6, 7] or after prostatectomy [8,9,10,11], or have a mixture of cases with initial prostatectomy and radiotherapy without treatment specific subgroup analysis [12,13,14,15,16,17,18]. Therefore, the clinical utility of 18F-fluciclovine in men with low and very low PSA levels following primary radiation therapy is not well-studied [19]. Additionally, the relationship between pre-scan PSA and PSA kinetic parameters and the ability of 18F-fluciclovine PET to identify recurrent disease after radiation therapy is still unclear. In this study, we aimed to determine (1) the detection rate of 18F-fluciclovine PET and the patterns of prostate cancer recurrence in patients with rising PSA after initial radiation therapy, particularly in patients with PSA rise less than the Phoenix criteria; (2) the relationship between pre-scan PSA and PSA kinetic parameters and the ability of 18F-fluciclovine PET to localize recurrent disease; and (3) the diagnostic accuracy of 18F-fluciclovine PET in patients with rising PSA after initial radiation.
Methods
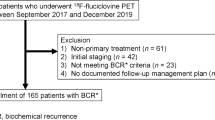
After obtaining institutional review board (IRB) approval from the University of California, San Francisco (UCSF) and the University of Minnesota (UMN), we retrospectively reviewed consecutive patients who underwent 18F-fluciclovine PET/CT or PET/MRI scans from April 2017 to February 2020 level for elevated PSA following initial definite external beam radiation therapy, brachytherapy, and/or proton therapy. Patients with an uncertain type of initial treatment or history of radiation therapy less than 1 year or brachytherapy less than 2 years before the 18F-fluciclovine PET scan were excluded (Fig. 1). Relevant clinical information, including demographic data, initial treatment, PSA levels with corresponding dates, PSA nadir, and pre-scan and follow-up imaging findings, was collected.
Image acquisition and radiopharmaceutical
The 18F-fluciclovine PET/CT and PET/MRI acquisitions were performed according to the ACR-ACNM practice parameters [20]. PET/CT scans were acquired on Biograph mCT-64HDTV PET/CT scanner (Siemens Healthcare, Erlangen, Germany) at UMN and Discovery (Discovery VCT, GE Healthcare, Waukesha, WI, USA) or Philips Vereos (Philips, Cleveland OH, USA) at UCSF. The PET/MRI scans were acquired on 3.0-T time-of-flight PET/MRI unit (Signa; GE Healthcare, Waukesha, WI, USA) at UCSF. All patients who underwent PET/MRI had dynamic contrast-enhanced (DCE) imaging of the pelvis unless there were contraindications.
Image interpretation
Scans were interpreted by board-certified nuclear radiologists and board-certified nuclear medicine physicians as part of routine clinical practice at these institutions. No image reinterpretation was performed in order to best replicate clinical practice. Based on clinical reports, 18F-fluciclovine-avid lesions were classified into four regions (intra-prostatic/prostate bed, pelvic lymph nodes, non-regional lymph node(s) (M1a), bone(s) (M1b), and distant metastasis with or without bone disease (M1c)).
Lesion validation
Clinical follow-up information including histopathologic analysis, imaging (CT, MRI, bone scan, PET), and serum PSA course after focal salvage therapy acquired during clinical routine was obtained. Combination of histopathologic analysis, follow-up imaging and PSA follow-up after local/focal treatment was considered the composite reference standard similar to a previous report [21]. In patients with the composite reference standard, 18F-fluciclovine-avid lesions were validated as true-positive or false-positive results. Region negative on 18F-fluciclovine PET, but with subsequently confirmed prostate cancer by histopathologic analysis, was considered a false-negative result. In patients with negative 18F-fluciclovine PET scans, a benign prostate biopsy was defined as true negative.
Calculating PSA kinetic parameters
All available posttreatment PSA values and corresponding dates were retrieved from the electronic health records. PSA nadir was identified from the urologists’ or radiation oncologists’ notes. To calculate PSA kinetic parameters, the three most recent PSA values prior to 18F-fluciclovine PET were entered into the Memorial Sloan Kettering online calculator [22]. If the slope of the linear regression of the natural log of PSA versus time (in months) was negative (decreased pre-scan PSA level after initial increased PSA levels following the PSA nadir) or 0 (elevated but stable PSA level), the PSADT was set to 100 months, as previously described [23].
Statistical analysis
Univariate and multivariate logistic regression analysis was used to estimate the association of Gleason sum, PSA, and PSADT with positive 18F-fluciclovine PET or extra-pelvic disease extension. The receiver operating characteristic (ROC) curve was performed to determine the predictive ability of PSA and PSA kinetic parameters for 18F-fluciclovine PET findings. The diagnostic performance of 18F-fluciclovine PET was computed in the prostate and at the patient level. The relationship between categorical variables was analyzed using Pearson χ2. Kruskal-Wallis test was used for nonparametric comparison of pre-scan PSA in subgroup analysis. If estimated individual cell frequencies were < 5, the Fisher exact test was conducted. Statistical analysis was performed using the MedCalc Statistical Software version 17.11.5 (MedCalc Software bvba, Ostend, Belgium). The alpha level for significance was set at 0.05.
Results
In total, 100 patients met the study inclusion criteria (n = 52 (52%) at UCSF; n = 48 (48%) at UMN. Ten patients underwent PET/MRI at UCSF; other patients underwent PET/CT, either at UMN or at UCSF. The median pre-scan PSA was 3.3 ng/mL (interquartile range (IQR), 1.6 to 6.4 ng/mL). Seventy-three men received EBRT, 24 men received brachytherapy, and three men received proton therapy. The median time between radiation therapy and 18F-fluciclovine PET was 66 (IQR: 36–120) months. There were 60 men with 18F-fluciclovine avidity in prostate (bed) (T), 18 men with pelvic lymph nodes (N), and 21 patients with distant metastases (M). Patient characteristics are described in Table 1.
Detection rate
Overall, 79 of 100 patients (79%) had positive findings on 18F-fluciclovine PET. We stratified the detection rate by Gleason sum (GS ≤ 7 versus GS ≥ 8), pre-scan PSA level, PSADT, and initial treatment (Table 2). In multivariate logistic regression using PSA and PSA velocity as continuous variables, only the pre-scan PSA value was significantly associated with a positive 18F-fluciclovine scan (OR 1.4, 95% CI 1.07–1.84, p < 0.001).
Phoenix criteria
Thirty-seven men had PSA rise below Phoenix criteria (PSA nadir +2 ng/mL). The median PSA in these patients was 1.4 ng/mL (IQR 1.0–2.0). 18F-Fluciclovine PET identified a site of suspected tumor recurrence in 62% (23/37) of these cases. Patients with pre-scan PSA greater than PSA nadir +2 ng/mL were significantly more likely to have a positive 18F-fluciclovine PET (88% versus 62%, OR 4.34, 95% CI 1.54–12.21, p = 0.004). In multivariate logistic regression using pre-PSA, PSADT, and PSA velocity as continuous variables and Phoenix criteria as a categorical variable, Phoenix criteria were the only independent predictor of a positive 18F-fluciclovine PET (OR 4.46, 95% CI 1.55–12.82, p = 0.004).
The ROC curves were generated to investigate the ability of PSA, PSADT, and PSA velocity to predict positive 18F-fluciclovine PET imaging in patients with PSA rise below Phoenix criteria (Fig. 2). PSA velocity had the highest area under curve (AUC) of 0.79 in comparison to the AUC of PSADT (0.66) and pre-scan PSA (0.54). Only PSA velocity significantly predicted the outcome of 18F-fluciclovine PET imaging (p < 0.001). The PSA velocity of 0.6 ng/mL/year generated the maximum Youden index with a sensitivity of 78% and specificity of 77% in predicting the outcome of the 18F-fluciclovine PET scan. The maximum Youden index for PSADT was estimated at 9.4 months, and this cutoff had a 61% sensitivity and specificity of 69% for predicting the outcome of the 18F-fluciclovine PET scan. In Fisher’s exact test, Gleason sum (GS ≤ 7 versus GS ≥ 8) was not able to predict positive 18F-fluciclovine PET in patients with PSA rise below Phoenix criteria (p = 0.20) or PSA < 2 ng/mL (p = 0.17).
Diagnostic accuracy
In 58 patients with biopsy (n = 44), or composite follow-up imaging, the positive predictive value of 18F-fluciclovine PET at the patient-level was 89% (95% CI: 80–94%). In 23 patients with PSA rise below the Phoenix criteria and biopsy or composite follow-up imaging, the positive predictive value of 18F-fluciclovine PET was 80% (95% CI: 60–91%).
In 35 men with prostate biopsy and findings limited to the prostate parenchyma, the sensitivity, positive predictive value, negative predictive value, and specificity of 18F-fluciclovine PET were 84.0% (95% CI: 64–95%), 80.7% (95% CI: 68.9–88.9%), 55.5% (95% CI: 29.6–78.8%), and 50.0% (95% CI: 18.7–81.3%), respectively.
Location of avid lesions
There were 102 sites of 18F-fluciclovine avidity in the 79 men. Local recurrence (intra-prostatic/prostate bed, pelvic lymph nodes) was the most common finding, occurring in 67% (67/100) of patients, with pelvic-confined disease in 58% (58/100) of cases. In patients with PSA rise below the Phoenix criteria with positive findings on 18F-fluciclovine PET, pelvic-confined disease was the most common finding (78% (18/23)).
We investigated the association of PSA, PSADT, PSA velocity, Gleason sum, and Phoenix criteria with extra-pelvic metastases in 18F-fluciclovine PET imaging. As a continuous variable, pre-scan higher PSA was significantly associated with identifying extra-pelvic 18F-fluciclovine PET positivity (OR 1.1, 95% CI 1.1–1.2, p = 0.02). PSADT as a continuous or categorical variable was significantly associated with extra-pelvic 18F-fluciclovine PET positivity, and PSA velocity as a continuous variable was significantly associated with positive extra-pelvic findings in 18F-fluciclovine PET (Table 3). Gleason sum, Phoenix criteria, pre-scan PSA > 2 ng/mL were not associated with extra-pelvic 18F-fluciclovine PET positivity. ROC curves were generated to compare the ability of PSA, PSADT, and PSA velocity to predict 18F-fluciclovine PET with positive extra-pelvic findings. These three parameters significantly predicted the presence of extra-pelvic findings. The PSADT had the highest AUC of 0.8 in comparison to AUC of PSA velocity (0.76) and pre-scan PSA (0.66) (Fig. 3); however, the difference between AUCs of PSADT, PSA velocity, and pre-scan PSA was not statistically significant. The PSADT of 5.2 months generated the maximum Youden index with a sensitivity of 79% and specificity of 70% in predicting the presence of extra-pelvic findings. The maximum Youden index for PSA velocity was estimated at 2.3 ng/mL/year, and this cutoff had sensitivity of 64% and specificity of 80% in predicting the presence of extra-pelvic findings. The PSA of 6.4 ng/mL generated the maximum Youden index with a sensitivity of 80% and specificity of 57% in predicting the presence of extra-pelvic findings.
Although the pre-scan PSA increased from M1a to M1c, the difference was not statistically significant (p = 0.3). Pre-scan PSA was 3.6 ng/mL (IQR 1.25–7.1), 7.6 ng/mL (IQR 2.2–15), and 8.1 ng/mL (IQR 6.5–10.6) for M1a, M1b, and M1c, respectively. The ROC curves were generated to investigate the ability of PSA, PSADT, and PSA velocity to differentiate M1a from M1c cases. The PSADT had the highest AUC of 0.86 in comparison to AUC of PSA velocity (0.73) and pre-scan PSA (0.8); however, the difference between AUCs was not statistically significant.
Discussion
In the current analysis, we aimed to determine the detection rate and diagnostic accuracy of 18F-fluciclovine PET in men with BCR and low/very low PSA levels (27 cases with PSA < 2 ng/mL) following primary radiation therapy. We focused on patients with PSA rise less than the Phoenix criteria (n = 37). 18F-fluciclovine PET identified recurrent disease with a PSA rise below the Phoenix criteria in 62% of patients, and in these patients, PSA velocity significantly predicted 18F-fluciclovine PET positivity. In patients with low PSA values, local recurrence (67%) and pelvic-confined disease (58%) were the most common findings. PSADT had the highest AUC (0.8), and PSADT of 5.2 months was shown to have a sensitivity of 79% to predict metastatic disease. 18F-Fluciclovine PET demonstrated a positive predictive value of 84% with relatively low specificity of 50% in the prostate bed. Patients with PSA rise below Phoenix criteriaand PSA velocity of 0.6 ng/mL/year or PSADT of less than 9 months, would likely benefit from 18F-fluciclovine PET imaging. By following the strict version of Phoenix criteria introduced in 2006, each patient can be compared with a large body of existing literature; however, our findings suggest that using more sensitive new radiotracers [24], patients would likely benefit from early identification of local recurrence and timely local salvage therapy.
It is worth empathizing that, in our study, equivocal interpretations in the prostate were analyzed as positive findings, since they commonly result in prostate biopsy. In the only published study focusing on non-prostatectomy definitive therapy [19], Akin-Akintayo and colleagues summarized the imaging findings of 18F-fluciclovine PET/CT of 24 patients with biochemical failure after non-prostatectomy definitive therapy and compared PET/CT findings with MRI and clinical or histopathologic reference standard. They demonstrated that the diagnostic performance of 18F-fluciclovine PET for extra-prostatic lesions was comparable to reported accuracy for patients with initial prostatectomy; however, for the treated prostate, 18F-fluciclovine PET/CT had high sensitivity (100%) with low specificity (11%). Although their study has strengths of prospective recruitment and comparison with MRI, the small sample size (n = 24) and relatively high pre-scan PSA (mean PSA of 8.5 ng/mL) limit the applicability to routine clinical practice. Moreover, patients with PSA less than 2 ng/mL or PSA rise below the Phoenix criteria (PSA nadir+2) were not recruited in their study. In our study, in 35 men with imaging findings limited to the prostate parenchyma and follow-up prostate biopsy, the 18F-fluciclovine PET showed lower sensitivity (84.0% versus 100%) and higher specificity (50.0% versus 11%) in comparison to Akin-Akintayo and colleagues’ study. Low specificity of 18F-fluciclovine PET for prostate parenchyma in these studies is in line with relatively high number of false-positive 68Ga-PSMA-11 PET/CT findings in prostate (bed) after radiotherapy as reported by Fendler et al. [25]. This can be due to inflammation and treatment changes. It is worth emphasizing that prostate biopsy was shown to have slightly limited accuracy when compared to whole-gland pathology [26], which can introduce more uncertainty in the evaluation of diagnostic performance of 18F-fluciclovine PET or PSMA PET.
Similar to our findings, Raveenthiran et al. [27] reported 75.3% (56/73) patients with suspected recurrent disease after initial definitive radiation therapy, and PSA < 2.0 ng/mL had evidence of recurrent disease on 68Ga-PSMA-11 PET/CT. The current study detection rate for patients with PSA < 2 ng/mL was slightly lower than Raveenthiran’s cohort (63.0% vs. 75.3%). In a comparative imaging trial, Calais et al. [11] also demonstrated 68Ga-PSMA-11 PET/CT had a higher detection rate than 18F-Fluciclovine in patients with BCR and PSA < 2.0 ng/mL after radical prostatectomy. Currently, 18F-fluciclovine is the only widely available FDA-approved PET radiotracer for prostate cancer in the USA. Given the higher accuracy and extensive theranostic applications of PSMA agents in various clinical settings [24, 28], 18F-fluciclovine PET would likely be replaced by PSMA PET in upcoming years. We believe that this study’s findings can be applied in early detection of extra-prostatic disease after radiation therapy usingmore sensitive radiotracers. However, implication of these findings in identification of prostate (bed) relapse after radiation therapy by newer radiotracers needs further investigating, since these agents have different uptake mechanism and can be affected by variable degrees of adjacent bladder/urine uptake [24, 25].
Our study’s strengths are the inclusion of patients with low PSA levels and PSA rise below Phoenix criteria, relatively high rate of patients with a reference standard, recruitment of patients from two institutions, and evaluation of the impact of PSA kinetic parameters. Our study is limited by retrospective design and relatively small sample size in subgroup analyses, for example, for the comparison of M1a versus M1c cases. Additionally, 10 patients underwent PET/MRI, and therefore, readers had access to simultaneous multiparametric MRI images with inherent higher accuracy for evaluation of prostate parenchyma than CT images (PET/CT), which is more widely used for evaluation of this group of patients. In eight patients with PET/MRI and biopsy of prostate, three PET/MRI demonstrated false-positive findings. Given the small number of cases with PET/MRI and biopsy, these findings were not highlighted in the results, and we recommend further studies to assess the diagnostic performance of 18F-fluciclovine PET/MRI or PSMA PET/MRI in patients with BCR after initial radiation therapy.
Conclusion
Our results indicate that 18F-fluciclovine PET can identify recurrent disease at low PSA level and PSA rise below accepted Phoenix criteria in patients with suspected BCR after primary radiation therapy. Particularly, this study supports the use of 18F-fluciclovine PET in patients with high PSA velocity or low PSADT even when the PSA rise is below Phoenix criteria. Finally, in patients with high PSA velocity or low PSADT, there is an increased probability of extra-pelvic metastases. Therefore, these patients are more likely to benefit from 18F-fluciclovine PET than pelvic MRI alone.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66:271–89.
Zumsteg ZS, Spratt DE, Romesser PB, Pei X, Zhang Z, Polkinghorn W, et al. The natural history and predictors of outcome following biochemical relapse in the dose escalation era for prostate cancer patients undergoing definitive external beam radiotherapy. Eur Urol. 2015;67:1009–16.
Roach M 3rd, Hanks G, Thames H Jr, Schellhammer P, Shipley WU, Sokol GH, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys. 2006;65:965–74.
Tan N, Oyoyo U, Bavadian N, Ferguson N, Mukkamala A, Calais J, et al. PSMA-targeted radiotracers versus (18)F fluciclovine for the detection of prostate cancer biochemical recurrence after definitive therapy: a systematic review and meta-analysis. Radiology. 2020;296:44–55.
Turkbey B, Mena E, Shih J, Pinto PA, Merino MJ, Lindenberg ML, et al. Localized prostate cancer detection with 18F FACBC PET/CT: comparison with MR imaging and histopathologic analysis. Radiology. 2014;270:849–56.
Alemozaffar M, Akintayo AA, Abiodun-Ojo OA, Patil D, Saeed F, Huang Y, et al. [(18)F]Fluciclovine positron emission tomography/computerized tomography for preoperative staging in patients with intermediate to high risk primary prostate cancer. J Urol. 2020;204:734–40.
Nanni C, Zanoni L, Pultrone C, Schiavina R, Brunocilla E, Lodi F, et al. (18)F-FACBC (anti1-amino-3-(18)F-fluorocyclobutane-1-carboxylic acid) versus (11)C-choline PET/CT in prostate cancer relapse: results of a prospective trial. Eur J Nucl Med Mol Imaging. 2016;43:1601–10.
Akin-Akintayo OO, Jani AB, Odewole O, Tade FI, Nieh PT, Master VA, et al. Change in salvage radiotherapy management based on guidance with FACBC (fluciclovine) PET/CT in postprostatectomy recurrent prostate cancer. Clin Nucl Med. 2017;42:e22–e8.
Solanki AA, Savir-Baruch B, Liauw SL, Michalski J, Tward JD, Vapiwala N, et al. (18)F-Fluciclovine positron emission tomography in men with biochemical recurrence of prostate cancer after radical prostatectomy and planning to undergo salvage radiation therapy: results from LOCATE. Pract Radiat Oncol. 2020;10:354–62.
Calais J, Ceci F, Eiber M, Hope TA, Hofman MS, Rischpler C, et al. (18)F-fluciclovine PET-CT and (68)Ga-PSMA-11 PET-CT in patients with early biochemical recurrence after prostatectomy: a prospective, single-centre, single-arm, comparative imaging trial. Lancet Oncol. 2019;20:1286–94.
Odewole OA, Tade FI, Nieh PT, Savir-Baruch B, Jani AB, Master VA, et al. Recurrent prostate cancer detection with anti-3-[(18)F]FACBC PET/CT: comparison with CT. Eur J Nucl Med Mol Imaging. 2016;43:1773–83.
Bach-Gansmo T, Nanni C, Nieh PT, Zanoni L, Bogsrud TV, Sletten H, et al. Multisite experience of the safety, detection rate and diagnostic performance of fluciclovine ((18)F) positron emission tomography/computerized tomography imaging in the staging of biochemically recurrent prostate cancer. J Urol. 2017;197:676–83.
Andriole GL, Kostakoglu L, Chau A, Duan F, Mahmood U, Mankoff DA, et al. The impact of positron emission tomography with 18F-fluciclovine on the treatment of biochemical recurrence of prostate Cancer: results from the LOCATE trial. J Urol. 2019;201:322–31.
England JR, Paluch J, Ballas LK, Jadvar H. 18F-Fluciclovine PET/CT detection of recurrent prostate carcinoma in patients with serum PSA </= 1 ng/mL after definitive primary treatment. Clin Nucl Med. 2019;44:e128–e32.
Savir-Baruch B, Lovrec P, Solanki AA, Adams WH, Yonover PM, Gupta G, et al. Fluorine-18-labeled fluciclovine PET/CT in clinical practice: factors affecting the rate of detection of recurrent prostate cancer. AJR Am J Roentgenol. 2019;213:851–8.
Schuster DM, Nieh PT, Jani AB, Amzat R, Bowman FD, Halkar RK, et al. Anti-3-[(18)F]FACBC positron emission tomography-computerized tomography and (111)In-capromab pendetide single photon emission computerized tomography-computerized tomography for recurrent prostate carcinoma: results of a prospective clinical trial. J Urol. 2014;191:1446–53.
Schuster DM, Savir-Baruch B, Nieh PT, Master VA, Halkar RK, Rossi PJ, et al. Detection of recurrent prostate carcinoma with anti-1-amino-3-18F-fluorocyclobutane-1-carboxylic acid PET/CT and 111In-capromab pendetide SPECT/CT. Radiology. 2011;259:852–61.
Akin-Akintayo O, Tade F, Mittal P, Moreno C, Nieh PT, Rossi P, et al. Prospective evaluation of fluciclovine ((18)F) PET-CT and MRI in detection of recurrent prostate cancer in non-prostatectomy patients. Eur J Radiol. 2018;102:1–8.
Savir-Baruch B, Banks KP, McConathy JE, Molchanova-Cook OP, Parent EE, Takalkar A, et al. ACR-ACNM practice parameter for the performance of fluorine-18 fluciclovine-PET/CT for recurrent prostate cancer. Clin Nucl Med. 2018;43:909–17.
Fendler WP, Calais J, Eiber M, Flavell RR, Mishoe A, Feng FY, et al. Assessment of 68Ga-PSMA-11 PET accuracy in localizing recurrent prostate cancer: a prospective single-arm clinical trial. JAMA Oncol. 2019;5:856–63.
Available from: https://www.mskcc.org/nomograms/prostate/psa_doubling_tim. Accessed between July 2019 - December 2020.
Trock BJ, Han M, Freedland SJ, Humphreys EB, DeWeese TL, Partin AW, et al. Prostate cancer-specific survival following salvage radiotherapy vs observation in men with biochemical recurrence after radical prostatectomy. JAMA. 2008;299:2760–9.
Lawhn-Heath C, Salavati A, Behr SC, Rowe SP, Calais J, Fendler WP, et al. Prostate-specific membrane antigen PET in prostate cancer. Radiology. 2021;299:248-260
Fendler WP, Calais J, Eiber M, Simko JP, Kurhanewicz J, Santos RD, et al. False positive PSMA PET for tumor remnants in the irradiated prostate and other interpretation pitfalls in a prospective multi-center trial. Eur J Nucl Med Mol Imaging. 2021;48:501–8.
Siddiqui MM, Rais-Bahrami S, Turkbey B, George AK, Rothwax J, Shakir N, et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA. 2015;313:390–7.
Raveenthiran S, Yaxley J, Gianduzzo T, Kua B, McEwan L, Wong D, et al. The use of (68)Ga-PET/CT PSMA to determine patterns of disease for biochemically recurrent prostate cancer following primary radiotherapy. Prostate Cancer Prostatic Dis. 2019;22:385–90.
Sonni I, Eiber M, Fendler WP, Alano RM, Vangala SS, Kishan AU, et al. Impact of (68)Ga-PSMA-11 PET/CT on staging and management of prostate cancer patients in various clinical settings: a prospective single-center study. J Nucl Med. 2020;61:1153–60.
Code availability
Not applicable.
Funding
Ali Salavati was supported by the Radiological Society of North America (RSNA) Research & Education Foundation, through grant number RR1963.The content is solely the responsibility of the authors and does notnecessarily represent the official views of the RSNA R&E Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of University of California, San Francisco, and University of Minnesota approved this study.
Consent to participate
Informed consent was waived by the local Ethics Committee of University of California, San Francisco, and University of Minnesota in view of the retrospective nature of the study, and all the procedures being performed were part of the routine care.
Consent for publication
Not applicable.
Conflict of interest
Ali Salavati, Mehmet Gencturk, Yasemin Koksel, Allyssa N. Schick, Steven P. Rowe, Courtney Lawhn-Heath, Jerry W. Froelich have no conflicts of interest to declare that are relevant to the content of this article. Thomas A. Hope served as a consultant toCurium and ITM and received research funding from Clovis and Philips. Thomas A. Hope also served on scientific advisory boards for Blue Earth, Ipsen. Peter R. Carroll served on an advisory board for Progenics. Felix Y. Feng has served as a consultant to Astellas, Bayer, Blue Earth, BMS, Exact Sciences, Foundation Medicine, Janssen, Myovant, Roivant, and Varian. Felix Y. Feng also serves on the scientifc advisoy boards of SerImmune and BlueStar Genomics.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology - Genitourinary
Rights and permissions
About this article
Cite this article
Salavati, A., Gencturk, M., Koksel, Y. et al. A bicentric retrospective analysis of clinical utility of 18F-fluciclovine PET in biochemically recurrent prostate cancer following primary radiation therapy: is it helpful in patients with a PSA rise less than the Phoenix criteria?. Eur J Nucl Med Mol Imaging 48, 4463–4471 (2021). https://doi.org/10.1007/s00259-021-05415-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-021-05415-y