Abstract
Purpose
The aim of our study was to comprehensively evaluate the most valuable metabolic parameters of cervical tumours and pelvic lymph nodes (PLN) by FDG-PET/CT to predict para-aortic lymph node (PALN) metastasis and stratify patients for surgical staging.
Methods
The study included patients with locally advanced cervical cancer, negative PALN uptake on preoperative FDG-PET/CT, and para-aortic lymphadenectomy. Two senior nuclear medicine physicians expert in gynaecologic oncology reviewed all PET/CT exams, and extracted tumour SUVmax, MTV, and TLG, as well as PLN. Prognostic parameters of PALN involvement were identified using ROC curves and logistic regression analysis.
Results
One hundred and twenty-five consecutive locally advanced cervical cancer patients were included. The FDG-PET/CT false-negative rate was, respectively, 27.7% (13/47) and 5.1% (4/78) in patients with and without FDG-PET/CT PLN uptake. The AUC of cervical tumour size, SUVmax, MTV, and TLG was, respectively, 0.75 (0.62–0.87), 0.59 (0.44–0.76), 0.75 (0.60–0.90), and 0.71 (0.56–0.86). The AUC of PLN size, SUVmax, SUVmean, PLN SUVmax/Tumour SUVmax ratio, MTV, and TLG was, respectively, 0.57 (0.37–0.78), 0.82 (0.68–0.95), 0.77 (0.61–0.94), 0.85 (0.72–0.98), 0.69 (0.51–0.87), and 0.74 (0.57–0.91). The metabolic parameter showing the best trade-off between sensitivity and specificity to predict PALN involvement was the ratio between PLN and tumour SUVmax.
Conclusion
The risk of PALN metastasis in FDG-PET/CT negative PLN patients is very low, so para-aortic lymphadenectomy does not seem justified. In patients with preoperative PLN uptake on FDG-PET/CT, surgical staging led to treatment modification in more than 25% of cases and should therefore be performed. Patients with more than one positive PLN and high PLN metabolic activity are at high risk of para-aortic extension and recurrence. Further prospective evaluation is required to consider intensified treatment modalities without prior PALN dissection.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Worldwide, cervical cancer is one of the most common malignant diseases [1]. Although often curable if detected early, more than one-third of patients present locally advanced cervical cancer (LACC) at diagnosis [2]. Guidelines from the European Society for Medical Oncology (ESMO), NCI, and the American Society of Clinical Oncology (ASCO) recommended in 2016 the use of pelvic radiotherapy (RT) plus concurrent low-dose platinum-based chemotherapy, followed by uterovaginal brachytherapy (BT) for LACC [3, 4].
Para-aortic lymph node (PALN) status at initial assessment is a major prognostic factor and a key-point for therapeutic strategy, since it defines the extent of radiation fields. 18-Fluorine fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) is the most reliable imaging test for assessing PALN involvement [3, 4]. A recent meta-analysis found that pooled estimates for sensitivity and specificity of FDG-PET/CT in detecting PALN metastasis were, respectively, 0.71 (95% CI = 0.54–0.83) and 0.97 (95% CI = 0.93–0.98) [5]. Indeed, false-negative results in the para-aortic (PA) area have been recorded in 5–17% of patients with negative preoperative FDG-PET/CT [6, 7]. According to the European Society of Gynaecologic Oncology (ESGO) guidelines, laparoscopic PALN dissection may be considered in patients with negative PALN on pretreatment FDG-PET/CT for staging purposes [8]. The survival benefit of surgical staging remains unclear. Brockbank et al.’s systematic review concluded that evidence of pretreatment PALN dissection benefit in patients with cervical cancer is insufficient, being based on a single small prospective trial comparing clinical and radiologic (CT or magnetic resonance imaging (MRI) staging [9].
In addition to lymph node evaluation, FDG-PET/CT provides functional information on tumours according to semi-quantitative parameters such as SUVmax (maximum standardized uptake value) and volumetric criteria such as MTV (metabolic tumour volume) and TLG (total lesion glycolysis) values. The prognostic value of primary tumour metabolic parameters has been shown in many studies [10,11,12]. Furthermore, several authors suggest that the pretherapeutic primary tumour SUVmax correlates with the presence of lymph node uptake at diagnosis [13, 14]. Pelvic lymph node (PLN) uptake and metabolic activity have also been suggested as interesting prognostic biomarkers [7, 15,16,17]. We hypothesized that tumour and PLN metabolic activity may predict PALN involvement in patients with no PALN FDG uptake, thereby helping to stratify patients for surgical staging.
The aim of our study was to evaluate whether cervical tumour FDG-PET/CT and PLN metabolic parameters can predict PALN metastasis, and to determine which criteria are the most accurate to identify lymph node extension to the PA area.
Methodology
The study included patients with LACC and negative aortic pretherapeutic FDG-PET/CT uptake treated at the Institut Claudius Regaud Cancer Center and the University Hospital in Toulouse, France, from January 2006 through March 2015. The project was approved by the institutional review board. Preoperative work-up in all cases included physical examination, cervical biopsy, pelvic MRI, FDG-PET/CT, and laparoscopic PALN retroperitoneal staging. Surgery began with a transperitoneal diagnostic laparoscopy to rule out occult carcinomatosis. A 10-mm port was inserted by open laparoscopy, and a 5-mm operative lateral trocar was used to improve peritoneal evaluation. Where peritoneal carcinomatosis was identified, the patient was excluded from the study and immediately sent for chemotherapy. If no anomaly was found, an extraperitoneal PA retroperitoneal lymph node dissection was immediately performed through an extraperitoneal approach, as previously described [18]. During surgical staging, a frozen section was performed if grossly positive lymph nodes were present. The procedure was aborted if lymph node involvement was confirmed. Patients underwent pelvic ± lombo-aortic external beam RT combined with chemotherapy. RT was administered to the whole pelvic region in 25 fractions of 1.8 Gray (Gy) for a total dose of 45 Gy for 5 weeks. The lombo-aortic area also received 45 Gy in 25 fractions when PA lymph node retroperitoneal staging was found to be positive. Concomitant chemotherapy with cisplatin 40 mg/m2 was administered weekly during RT for five courses. The treatment was then completed with an additional pulse dose rate intracavitary BT, for an equivalent total dose of 80–90 Gy. Before 2008, additional boosts (up to an equivalent total dose of 65 Gy) were sometimes given at the end of BT in cases of macroscopic lymph node and/or parametrial involvement. When Intensity-Modulated Radiation Therapy (IMRT) became available, a simultaneous integrated boost was performed on macroscopic PLN at doses of 57.5 Gy in 25 fractions. Completion surgery aimed at achieving clear margins was offered 6 weeks after BT in patients with residual tumours after chemoradiotherapy (CRT). Follow-up included clinical examination of patients every 4 months for 2 years, and every 6 months for the following 3 years.
Exclusion criteria consisted of non-available images of FDG-PET/CT for double reading, distant metastasis or peritoneal carcinomatosis found at laparoscopic examination of the abdominal cavity, and patients with PALN FDG-PET/CT uptake.
Medical data were extracted from computerized medical records and included demographics, clinical characteristics, imaging, surgical staging, surgicopathologic findings, treatment, and follow-up data, as well as recurrence and survival status at the end of the study.
FDG-PET/CT modalities and review
Prior to any treatment, FDG-PET/CT was performed in the initial work-up according to standardized institutional protocol. FDG-PET/CT whole-body images were obtained using a full-ring PET/CT scanner. Patients fasted for at least 6 h before scanning. Blood glucose levels were checked before FDG injection; injected dose and time between injection and acquisition were noted. If necessary regarding bladder repletion and urinary activity, complementary pelvic acquisitions could be done after administering 20 mg of furosemide. PET data were reconstructed using an iterative, fully 3D algorithm with CT images for attenuation correction. A senior nuclear medicine physician, expert in gynaecologic cancer, analyzed all FDG-PET/CT images in standard clinical fashion. All patients had a double-blinded review of metabolic parameters performed by another senior nuclear medicine specialist. Segmentation of cervical tumour volumes and PLN was done using General Electric AWserver 3.0 software with an automatic thresholding at 40% of SUVmax, following EANM (European Association of Nuclear Medicine) guidelines [19]. Manual correction was used in a few cases to exclude urinary tract activity, mostly in patients who had not received furosemide and whose bladder activity was equal or superior to tumour uptake. This was also the case when the AWServer automatic thresholding process was not suitable. For this modification, we used CT scan and visual uptake differences between tumour and urinary activity. Other tumour contours were not modified. The metabolic parameters studied were SUVmax, MTV, and TLG for primitive cervical tumour and for PLN when positive. The size of PLN was measured on CT imaging. The MTV and TLG of PLN used in our study were measured from the most FDG-avid lesion, allowing for quick assessment by means of a procedure that can be used in daily clinical practice.
Statistical analysis
Data were summarized by median and range (min–max) for continuous variables and according to frequency and percentage for qualitative variables. Comparisons between groups were done using a Mann-Whitney test for continuous variables and chi-square or Fisher’s exact test for qualitative variables. A multivariate analysis based on a logistic regression model was performed to evaluate the impact of tumour parameters on lymph node extension to the PA region. Area under the ROC curve (AUC), with 95% confidence intervals (CI), was calculated for each metabolic parameter to estimate the discrimination capacity between PALN+ and PALN−. A decision curve analysis was also performed to evaluate the clinical usefulness of each metabolic parameter by calculating net benefit. We defined a model as clinically useful if its curve was above None and All, assuming, respectively, that none of the patients or all of the patients had PALN involvement. All tests were two-sided with significance set at p < 0.05. Statistical analyses were carried out using Stata® version 13; net benefit curves were performed using the R package RMDA.
Results
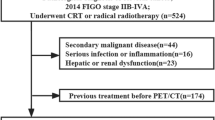
During the study period, 183 patients met inclusion criteria. Fifty-eight patients were excluded for the following reasons: 23 patients for unavailable PET CT images, 34 for PALN involvement, and one patient for incomplete CRT. Median tumour size was 5 cm (range 2.4–9 cm) at pretherapeutic FDG-PET/CT (Table 1). The median number of PALN removed was 18.5 (range 5–48). One additional patient had macroscopic lymph node involvement confirmed by frozen section, and she underwent extended-field radiotherapy dissection. The proportion of patients with no PA lymph node uptake on FDG-TEP/CT and with pathology-proven lymph node involvement after surgical staging (false-negative rate) was, respectively, 13.6% (17/125), 5.1% (4/78) in patients without FDG-PET/CT PLN uptake, and 27.7% (13/47) in patients with PLN FDG-PET/CT uptake. Among patients with PALN involvement, two had isolated tumour cells, five had micrometastatic disease, and 12 had macrometastasis. Eight patients with macrometastasis had two or more positive nodes. Among the four patients with negative PLN and positive PALN, two presented with micrometastasis of 0.5 and 0.2 mm. Clinical characteristics, age, tumour type, and FIGO stage were similar in patients with or without PALN involvement. Median tumour size was, respectively, 6 cm (range 3–8.3 cm) and 5 cm (range 2.4–9 cm) in patients with and without PALN involvement.
Metabolic parameters of cervical tumour and pelvic lymph nodes
Median values of cervical tumour SUVmax, MTV, and TLG for the whole population were, respectively, 14.5 (range 2.1–34.4), 37.5 cc (range 0.8–162), and 248.8 (range 1.2–2495). MTV, TLG, and size of the cervical tumour, as measured on pretherapeutic FDG-PET/CT, were significantly higher in PALN positive patients with medians of, respectively, 73.1 vs. 34, p = 0.0039; 496.8 vs. 234, p = 0.0167, and 6 cm vs. 5 cm, p = 0.0012 (Table 2).
Forty-seven patients had abnormal PLN uptake. Thirteen (27.7%) with positive PALN and 34 (72.3%) with negative PALN had positive PLN (p = 0.0028). PLN SUVmax, MTV, and TLG were significantly higher in PALN positive patients (Table 2).
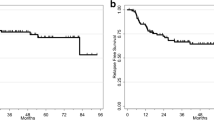
Tumour and PLN metabolic parameters that showed the best trade-off between sensitivity and specificity to predict PALN involvement were calculated using the ROC curve. The AUC of tumour size, SUVmax, MTV, and TLG of the cervical tumour was, respectively, 0.75 (0.62–0.87), 0.59 (0.44–0.76), 0.75 (0.60–0.90), and 0.71 (0.56–0.86). This analysis showed that size and MTV of tumours had the best discrimination capacity between PALN+ and PALN−, although there was little clinical benefit (Fig. 1). The AUC of PLN size, SUVmax, SUVmean, PLN SUVmax/Tumour SUVmax ratio, MTV, and TLG was, respectively, 0.57 (0.37–0.78), 0.82 (0.68–0.95), 0.77 (0.61–0.94), 0.85 (0.72–0.98), 0.69 (0.51–0.87), and 0.74 (0.57–0.91). This analysis showed that the PLN SUVmax/Tumour SUVmax ratio, PLN SUVmax, and PLN SUVmean had the best discrimination capacity and an acceptable net benefit (Fig. 2). The latter was positive for patients with a PALN metastasis probability of approximately 25 to 55% for PLN/Tumour SUVmax ratio and approximately 25 to 60% for SUVmax and SUVmean.
In patients with more than one PLN metastasis (n = 30), the PLN SUVmax/Tumour SUVmax ratio was significantly linked to PALN (p = 0.02), and more than 90% of patients with PALN involvement had a PLN SUVmax/Tumour SUVmax ratio higher than 0.5. Respectively, 8% and 53% of patients with a PLN SUVmax/Tumour SUVmax ratio of ≤ 0.5 and > 0.5 had PALN metastasis.
In univariate analysis, pretherapeutic tumour size, presence of PLN uptake, metabolic parameters, and number of PLN uptake at FDG-PET/CT were significantly linked to PALN involvement. After a backward selection, tumour MTV, odds ratio (OR) 1.24 (95% CI 1.02–1.50), and number of pelvic lymph nodes involved, OR 2.13 (1.33–3.40), remained significant factors linked to aortic metastasis in multivariate logistic regression analysis.
Discussion
PALN risk assessment based on clinical and metabolic data
Assessment of aortic lymph node involvement has been carried out using different imaging modalities, but none of them has demonstrated sufficient sensitivity [6, 20, 21]. FDG-PET/CT is used as a reference imaging test in pretreatment assessment of LACC to assess disease extent, lymph node involvement, and distant sites of metastatic disease [22]. FDG-PET/CT is also used for RT treatment planning in many institutions worldwide. However, FDG-PET/CT fails to detect between 10 and 15% of patients with negative FDG-PET/CT aortic nodes who will be seen to have lymph node metastasis upon pathologic staging [6, 21, 23]. In accordance with the literature, the false-negative rate in our series was 13.6%. In most cases, PALN involvement was associated with PLN status. Indeed, upon pathologic examination, 20–25% of patients with suspicious PLN metastasis at preoperative FDG-PET/CT had extension to the PA area [6, 24]. Surgical staging led to treatment modification in 24.4% of patients with PLN metastasis. This false-negative rate is probably related to the limited spatial resolution of FDG-PET/CT, since patients with negative PALN uptake are more likely to have small-volume lymph node metastasis [24, 25]. Indeed, metastases measuring less than 5 mm have been found in approximately half of the patients with negative PALN on preoperative FDG-PET/CT [24, 26].
As in other studies, PLN uptake was the most significant factor associated with PALN extension [24], and the risk of PA extension increased with the number of PLN involved [27]. Our results also show that each positive pelvic lymph node increased the risk of aortic involvement by 2.13, and each 10 cm3 increase in tumour MTV was associated with 1.24 higher risk of aortic involvement. SUVmax may be a less powerful variable in large cervical tumours, as in this series, and may be affected by statistical noise and voxel size. Advantages of MTV over SUVmax as a predictive prognostic parameter have been reported in several series [28, 29]. Our results also showed a strong correlation between high values of all PLN metabolic parameters, SUVmax, SUV mean, MTV, TLG, and risk of PALN metastasis. Furthermore, they indicate that the PLN and tumour SUVmax ratio was the best tool for predicting PALN involvement in patients whose disease had already spread to PLN. When more than one PLN was involved, the value of PLN SUVmax was at least half that of tumour SUVmax in 90% of patients with PALN metastasis.
Most studies have included all stages of cervical cancer and have focused on the relationship between metabolic parameters and clinical outcome [10, 12, 15, 29,30,31]. Other reports show that PLN metabolic activity is an accurate prognostic biomarker for predicting disease outcome [15, 30, 31]. Comprehensive analysis of tumour and lymph node metabolic parameters to stratify the risk of PALN involvement in order to select candidates for surgical staging has not yet been investigated. One study showed significantly higher rates of PALN metastasis in patients with PLN SUVmax ≥ 7.5 [16]. Another study focussing on the textural features of cervical tumour cell homogeneity showed that a large MTV coupled with a high degree of homogeneity or a high TLG mean coupled with a high level of homogeneity significantly increased the risk of PLN or PALN metastasis, and were more accurate than the SUVmax predictor [32].
Benefit of lymphadenectomy
Lymph node aortic status is the most important prognostic factor in patients with LACC [24]. In addition, aortic involvement guides treatment planning to adapt the RT field. When aortic lymph node metastases are found, the RT field is extended to the upper abdomen [33]. Many institutions advocate surgical aortic staging to avoid aortic negative patients being overtreated with extended-field radiation and metastatic aortic patients being undertreated by exclusive pelvic RT. The benefit of surgical staging remains unclear and depends on several issues. Does PALN extension modify treatment strategy, and does it significantly improve survival? What is the surgically associated morbidity and its effect in delaying CRT? Does prophylactic PA radiation improve survival in high-risk patients? Studies addressing the survival benefit of PALN dissection remain controversial [20, 23, 24, 27, 34]. Only one randomized trial performed by Lai et al. has addressed this question, but this study was prematurely closed and was limited by many methodological biases [35]. Designed to determine survival difference of surgical and radiologic staging in patients with PLN uptake on preoperative FDG-PET/CT, the LiLACs trial is, unfortunately, no longer active (NCT02848716). The Cochrane review found no evidence that surgical staging was beneficial, and decision to offer lymphadenectomy in LACC should be individualized [9]. Our results indicate that preoperative FDG-PET/CT is a useful tool to stratify candidates for surgical staging.
When lymphadenectomy is performed by trained teams, both the risk of grades III–IV morbidity and the proportion of patients where CRT is delayed more than 30 days after surgery, due to surgically associated morbidity, are less than 5% [36]. In our experience, when retroperitoneal aortic lymphadenectomy is performed by expert teams, intraoperative morbidity is found in 1% of patients (due to vascular injuries all located above the inferior mesenteric artery (IMA)), and perioperative morbidity is identified in 6.5% of cases [26]. Since lymph node progression occurs in a stepwise manner, a staging procedure up to the IMA might be considered, thereby reducing both the risk of intraoperative complications and operative time, with less than 5% risk of misdiagnosing aortic lymphatic involvement [26].
Survival of patients with PALN involvement remains poor, with a 30–50% 3-year survival rate, and a majority of distant failures [37]. In our series, more than 50% of patients with PA extension presented with distant recurrence. When the radiation field is extended to the PA region, the risk of PA and distant disease is reduced [38]. In an attempt to limit systemic failures, adjuvant chemotherapy after CRT has emerged as a therapeutic option to improve survival rate. Gonzalez et al. reported both an improved survival rate and time to progressive disease in patients treated with combined cisplatin gemcitabine CRT followed by two cycles of cisplatin and gemcitabine [39]. Two ongoing randomized trials, OUTBACK (NCT01414608) and INTERLACE (NCT01566240), are evaluating the benefit of adjuvant chemotherapy in LACC. The French multicentric study ONCOCOL01 (NCT03534713) will address the role of neoadjuvant chemotherapy specifically in PALN positive patients.
Clinical implications of our study include stratification according to tumour and PLN metabolic activity. Our results, along with those of other authors, show that the risk of PALN involvement in PLN FDG-PET/CT negative patients is less than 5% and surgical staging procedure should be abandoned. In our series, metabolic parameters—TLG value in particular—increased in patients with isolated PALN metastasis. We therefore consider that surgical staging should be performed in patients with PLN involvement to adapt the RT field and to tailor adjuvant treatment. The risk of PALN involvement is increased by the number of suspicious PLN and by the increasing values of PLN metabolic parameters. In patients with more than one PLN and with high PLN metabolic activity, the risk of aortic involvement and recurrence is also high [15,16,17]. To decrease delay in starting CRT, intensified treatment with prophylactically extended-field RT may be considered (Fig. 3). However, further prospective clinical evaluation is required to confirm both the risk of aortic involvement and outcome according to PLN metabolic activity.
Strengths of our study were the homogeneity of our cohort including only LACC patients treated with CRT, with no PALN FDG uptake, and who all benefitted from PALN surgical staging and double FDG-PET/CT interpretation by expert nuclear medicine physicians. Limitations of our study include its retrospective character, and the fact that FDG-PET/CT results may be difficult to generalize, due to differences in image acquisition and interpretation procedures among institutions.
Conclusion
PALN involvement is a surrogate marker of systemic disease and requires intensified treatment modalities. FDG-PET/CT is the most accurate diagnostic tool to evaluate PA extension in LACC, despite its significant false-negative rate. The present study of a cohort of 125 patients with LACC and negative FDG-PET/CT of the PALN region revealed that the risk of PALN false negatives in such patients is very low, eliminating the justification for PA lymphadenectomy. In patients with preoperative PLN uptake on FDG-PET/CT, surgical staging led to treatment modification in more than 25% of cases and should be performed. Patients with more than one PLN and high PLN metabolic activity run an elevated risk of PA extension and recurrence. Further prospective evaluation is required to consider intensified treatment modalities without prior PALN dissection.
References
Global Cancer Observatory, OMS. Estimated number of incident cases, worldwide ( top 10 cancer sites ) in 2012. Dispon. sur http//gco.iarc.fr/today/online-analysis-multi-bars?mode=cancer&mode_population=continents&population=900&sex=2&cancer=16&type=0&statistic=0&prevalence=0&color_palette=default. Accessed 2017. p. 2012
Quinn M a, Benedet JL, Odicino F, Maisonneuve P, Beller U, Creasman WT, et al. Carcinoma of the cervix uteri. FIGO 26th annual report on the results of treatment in gynecological cancer. Int J Gynaecol Obstet. 2006;95(Suppl 1):S43–103.
Marth C, Landoni F, Mahner S, McCormack M, Gonzalez-Martin A, Colombo N. Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28:iv72–83.
Chuang LT, Temin S, Camacho R, Feldman S, Gultekin M, Gupta V, et al. Management and care of women with invasive cervical cancer: American Society of Clinical Oncology resource-stratified clinical practice guideline. J Glob Oncol. 2016;2:1–30.
Yu W, Kou C, Bai W, Yu X, Duan R, Zhu B, et al. The diagnostic performance of PET / CT scans for the detection of para-aortic metastatic lymph nodes in patients with cervical cancer : a meta-analysis. PloS One. 2019;14(7):e0220080. https://doi.org/10.1371/journal.pone.0220080.
Gouy S, Morice P, Narducci F, Uzan C, Gilmore J, Kolesnikov-Gauthier H, et al. Nodal-staging surgery for locally advanced cervical cancer in the era of PET. Lancet Oncol. 2012;13:e212–20.
Gouy S, Morice P, Narducci F, Uzan C, Martinez A, Rey A, et al. Prospective multicenter study evaluating the survival of patients with locally advanced cervical cancer undergoing laparoscopic para-aortic lymphadenectomy before chemoradiotherapy in the era of positron emission tomography imaging. J Clin Oncol. 2013;31:3026–33.
Cibula D, Pötter R, Planchamp F, Avall-lundqvist E, Fischerova D, Haie C, et al. The European Society of Gynaecological Oncology / European Society for Radiotherapy and Oncology / European Society of Pathology guidelines for the management of patients with cervical cancer. Radiother Oncol. 2019;127:404–16 Available from: https://doi.org/10.1016/j.radonc.2018.03.003.
Brockbank E, Kokka F, Bryant A, Pomel C, Reynolds K. Pre-treatment surgical para-aortic lymph node assessment in locally advanced cervical cancer ( review ). Cochrane Database Syst Rev. 2013;(3):CD008217. https://doi.org/10.1002/14651858.CD008217.pub3.
Kidd EA, Siegel BA, Dehdashti F. The standardized uptake value for F-18 fluorodeoxyglucose is a sensitive predictive biomarker for cervical cancer treatment response and survival. Cancer. 2007;110(8):1738–44. https://doi.org/10.1002/cncr.22974.
Sarker A, Im H-J, Cheon GJ, Chung HH, Kang KW, Chung J-K, et al. Prognostic implications of the SUVmax of primary tumors and metastatic lymph node measured by 18F-FDG PET in patients with uterine cervical cancer. A meta-analysis. Clin Nucl Med. 2016;41(1):34–40. https://doi.org/10.1097/RLU.0000000000001049.
Voglimacci M, Gabiache E, Lusque A, Ferron G, Ducassou A, Querleu D, et al. Chemoradiotherapy for locally advanced cervix cancer without aortic lymph node involvement : can we consider metabolic parameters of pretherapeutic FDG-PET / CT for treatment tailoring ? Eur J Nucl Med Mol Imaging. 2019;46(7):1551–9. https://doi.org/10.1007/s00259-018-4219-5.
Onal C, Reyhan M, Parlak C, Guler OC, Oymak E. Prognostic value of pretreatment F-18-fluorodeoxyglucose uptake in patients with cervical cancer treated with definitive chemoradiotherapy. Int J Gynecol Cancer. 2013;23:1104–10.
Vural GU, Akkas BE, Demirel BB. Standardized uptake value and metabolic tumor volume measured by 18 F FDG PET / CT are sensitive biomarkers for the presence of lymph node metastasis in patients with cervical carcinoma. Rev Esp Med Nucl Imagen Mol. 2014;33:268–73.
Kidd EA, Siegel BA, Dehdashti F, Grigsby PW. Pelvic lymph node F-18 fluorodeoxyglucose uptake as a prognostic biomarker in newly diagnosed patients with locally advanced cervical cancer. 2010;116(6):1469–1475. https://doi.org/10.1002/cncr.24972.
Onal C, Guler OC, Reyhan M, Fuat A. Prognostic value of 18 F-fluorodeoxyglucose uptake in pelvic lymph nodes in patients with cervical cancer treated with definitive chemoradiotherapy. Gynecol Oncol. 2015;137:40–6.
Chung HH, Cheon GJ, Kang KW, Kim JW, Park N-H, Song YS. Preoperative PET / CT FDG standardized uptake value of pelvic lymph nodes as a significant prognostic factor in patients with uterine cervical cancer. Eur J Nucl Med Mol Imaging. 2014;41(4):674–81.
Sonoda Y, Leblanc E, Querleu D, Castelain B, Papageorgiou TH, Lambaudie E, et al. Prospective evaluation of surgical staging of advanced cervical cancer via a laparoscopic extraperitoneal approach. Gynecol Oncol. 2003;91:326–31.
Boellaard R, Delgado-Bolton R, Oyen WJG, Giammarile F, Tatsch K, Eschner W, et al. FDG PET / CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42:328–54.
Gold MA, Tian C, Whitney CW, Rose PG, Lanciano R. Surgical versus radiographic determination of para-aortic lymph node metastases before chemoradiation for locally advanced cervical carcinoma. Cancer. 2008;112(9):1954–63. https://doi.org/10.1002/cncr.23400.
Havrilesky LJ, Kulasingam SL, Matchar DB, Myers ER. FDG-PET for management of cervical and ovarian cancer. Gynecol Oncol. 2005;97:183–91.
Marth C, Landoni F, Mahner S, McCormack M, Gonzalez-Martin A, Colombo N. Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28:iv72–83.
Leblanc E, Gauthier H, Querleu D, Ferron G, Zerdoud S, Morice P, et al. Accuracy of 18-Fluoro-2-deoxy-d-glucose positron emission tomography in the pretherapeutic detection of occult para-aortic node involvement in patients with a locally advanced cervical carcinoma. Ann Surg Oncol. 2011;18:2302–9.
Gouy S, Morice P, Narducci F, Uzan C, Martinez A, Rey A, et al. Prospective multicenter study evaluating the survival of patients with locally advanced cervical cancer undergoing laparoscopic para-aortic lymphadenectomy before chemoradiotherapy in the era of positron emission tomography. J Clin Oncol. 2013;31(24):3026–33. https://doi.org/10.1200/JCO.2012.47.3520.
Vergote I, Tsolakidis D, Mortier D, Neven P, Amant F, Mottaghy F, et al. Value of positron emission tomography of the para-aortic lymph nodes in cervical carcinoma stage IB2-IIIB. J Clin Oncol. 2008;26:5654–5 Available from: http://ascopubs.org/doi/10.1200/JCO.2008.19.5883. Accessed 2008
Imaging PPPET, Leblanc E, Katdare N, Narducci F, Bresson L, Gouy S, et al. Should Systematic Infrarenal Para-aortic Dissection Be the Rule in the Pretherapeutic Staging of Primary or Recurrent Locally Advanced Cervix Cancer Patients With a Negative Preoperative Para-aortic PET Imaging?. Int J Gynecol Cancer. 2016;26:169–75.
Han X, Wen H, Ju X, Chen X, Ke G. Predictive factors of para-aortic lymph nodes metastasis in cervical cancer patients: a retrospective analysis based on 723 para-aortic lymphadenectomy cases. Onctarget. 2017;8:51840–7.
Chung HH, Kim JW, Han KH, Eo JS, Kang KW, Park N-H, et al. Prognostic value of metabolic tumor volume measured by FDG-PET/CT in patients with cervical cancer. Gynecol Oncol. 2011;120:270–4 Available from: https://linkinghub.elsevier.com/retrieve/pii/S0090825810007985. Accessed 2011.
Hong JH, Min KJ, Lee JK, So KA, Jung US, Kim S, et al. Prognostic value of the sum of metabolic tumor volume of primary tumor and lymph nodes using 18F-FDG PET/CT in patients with cervical cancer. Medicine (Baltimore). 2016;95:e2992 Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00005792-201603010-00074. Accessed 2016.
Chung HH. Prognostic importance of lymph node-to-primary tumor standardized uptake value ratio in invasive squamous cell carcinoma of uterine cervix. Eur J Nucl Med Mol Imaging. 2017;44(11):1862–9. https://doi.org/10.1007/s00259-017-3729-x.
Brunette LL, Bonyadlou S, Ji L, Groshen S, Shuster D, Mehta A, et al. Predictive value of FDG PET / CT to detect lymph node metastases in cervical cancer. Clin Nucl Med. 2018;43:793–801.
Shen W-C, Chen S-W, Liang J-A, Hsieh T-C, Yen K-Y, Kao C-H. [18]Fluorodeoxyglucose positron emission tomography for the textural features of cervical cancer associated with lymph node metastasis and histological type. Eur J Nucl Med Mol Imaging. 2017;44:1721–31 Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s00259-017-3697-1.
Varia MA, Bundy BN, Deppe G, Mannel R, Averette HE, Rose PG, et al. Cervical carcinoma metastatic to para-aortic nodes: extended field radiation therapy with concomitant 5-fluorouracil and cisplatin chemotherapy: a gynecologic oncology group study. Int J Radiat Oncol. 1998;42:1015–23 Available from: https://linkinghub.elsevier.com/retrieve/pii/S0360301698002673.
Pomel C, Martinez A, Bourgin C, Beguinot M, Benoit C, Naik R, et al. Survival effect of laparoscopic para-aortic staging in locally advanced cervical cancer : a retrospective cohort analysis. BJOG. 2017;124(7):1089–94. https://doi.org/10.1111/1471-0528.14492.
Lai C, Huang K, Hong J, Lee C, Chou H, Chang T, et al. Randomized trial of surgical staging ( extraperitoneal or laparoscopic ) versus clinical staging in locally advanced cervical cancer. Gynecol Oncol. 2003;89:160–7.
Uzan C, Souadka A, Gouy S, Debaere T, Duclos J, Lumbroso J, et al. Analysis of morbidity and clinical implications of laparoscopic para-aortic lymphadenectomy in a continuous series of 98 patients with advanced-stage cervical cancer and negative PET-CT imaging in the para-aortic area. Oncologist. 2011;16:1021–7 Available from: http://theoncologist.alphamedpress.org/cgi/doi/10.1634/theoncologist.2011-0007.
Manders DB, Sims TT, Bailey A, Hwang L, Richardson DL, Miller DS, et al. The Significance of Para-Aortic Nodal Size and the Sole of Adjuvant Systemic Chemotherapy in Cervical Cancer: An Institutional Experience. Am J Clin Oncol. 2018;41:1225–30.
Sapienza LG, Fernando V, Jr MML, Baiocchi G, Janeiro D, Sloan M, et al. HHS Public Access 2018;144:312–7.
Duen A. Phase III, Open-label, randomized study comparing concurrent gemcitabine plus cisplatin and radiation followed by adjuvant gemcitabine and cisplatin versus concurrent cisplatin and radiation in patients with stage IIB to. J Clin Oncol. 2019;29(13):1678–85. https://doi.org/10.1200/JCO.2009.25.9663.
Acknowledgements
Martina Aida Angeles acknowledges grant support from “La Caixa” Foundation, Barcelona, Spain. We would also like to thank Dr. Gail Taillefer, a native English speaker experienced in scientific publication, for her review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology – Genitourinary
Electronic supplementary material
ESM 1
(DOCX 39 kb)
Rights and permissions
About this article
Cite this article
Martinez, A., Voglimacci, M., Lusque, A. et al. Tumour and pelvic lymph node metabolic activity on FDG-PET/CT to stratify patients for para-aortic surgical staging in locally advanced cervical cancer. Eur J Nucl Med Mol Imaging 47, 1252–1260 (2020). https://doi.org/10.1007/s00259-019-04659-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04659-z