Abstract
Purpose
The A/T/N model is a research framework proposed to investigate Alzheimer’s disease (AD) pathological bases (i.e., amyloidosis A, neurofibrillary tangles T, and neurodegeneration N). The application of this system on clinical populations is still limited. The aim of the study is to evaluate the topography of T distribution by 18F-flortaucipir PET in relation to A and N and to describe the A/T/N status through imaging biomarkers in memory clinic patients.
Methods
Eighty-one patients with subjective and objective cognitive impairment were classified as A+/A− and N+/N− through amyloid PET and structural MRI. Tau deposition was compared across A/N subgroups at voxel level. T status was defined through a global cut point based on A/N subgroups and subjects were categorized following the A/T/N model.
Results
A+N+ and A+N− subgroups showed higher tau burden compared to A−N− group, with A+N− showing significant deposition limited to the medial and lateral temporal regions. Global cut point discriminated A+N+ and A+N− from A−N− subjects. On A/T/N classification, 23% of patients showed a negative biomarker profile, 58% fell within the Alzheimer’s continuum, and 19% of the sample was characterized by non-AD pathologic change.
Conclusion
Medial and lateral temporal regions represent a site of significant tau accumulation in A+ subjects and possibly a useful marker of early clinical changes. This is the first study in which the A/T/N model is applied using 18F-flortaucipir PET in a memory clinic population. The majority of patients showed a profile consistent with the Alzheimer’s continuum, while a minor percentage showed a profile suggestive of possible other neurodegenerative diseases. These results support the applicability of the A/T/N model in clinical practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 2018, the National Institute on Aging and Alzheimer’s Association (NIA-AA) proposed a “research framework” based on the A/T/N model [1] for observational and interventional research on Alzheimer’s disease (AD) [2]. Differently from the NIA-AA diagnostic criteria [3], this framework defines AD as a biological rather than a clinical construct, characterized by extracellular deposits of β-amyloid peptide (Aβ; “A”), intraneuronal aggregates of hyperphosphorylated tau (“T”) and neurodegeneration (“N”). The A/T/N model considers A, T, and N status relatively independent from one another. As a consequence, this model takes into consideration possible alternative biomarker pathways leading to AD, together with clear negative (A−T−N−) and positive (A+T+N+) AD profiles. In particular, the description of subjects with an A−N+ profile (i.e., suspected non-Alzheimer’s pathology (SNAP)) [4], who represent approximately the 25% of both cognitively unimpaired individuals aged > 65 year and mildly cognitive impaired individuals [4], questions the classical temporal evolution of AD biomarkers. Overall, these findings call for the investigation of the dynamic interactions between AD-related pathological phenomena through multimodal biomarkers in order to characterize and identify differential disease trajectories, as this could lead to a significant improvement in guiding diagnostic and prognostic reasoning in clinical practice.
Studies applying the A/T/N model on clinical and preclinical populations are still limited [5,6,7,8,9]. Overall, they suggest an age effect in the A/T/N profile distribution in cognitively unimpaired subjects [7], and a variability in clinical population according to the clinical disease stage [8]. Notably, Ekman and colleagues explored the A/T/N frequencies in patients with stable mild cognitive impairment (MCI) or who progressed to dementia at 36 months of follow-up, showing that 84% of progressor MCI presented at baseline an A+T+ profile (A+T+N+ 54%, A+T+N− 30%), compared to 48% of stable MCI (29% A+T+N+ 19% A+T+N−) and 21% of healthy controls (A+T+N+ 12%, A+T+N− 9%) [8]. Thus, the presence of tau pathology associated to amyloid positivity might represent a strong indicator of clinical decline. The introduction of PET tracers with high affinity to paired helical tau filaments (see [10] for review) and successfully discriminating AD from other neurodegenerative disease [11] offers the opportunity not only to evaluate the T positivity but also to describe its topographical distribution, representing thus a biomarker of disease stage [2].
Aim of the study was to evaluate in a patient population enrolled in a prospective study currently ongoing at the Geneva University Hospitals the occurrence and distribution of tau pathology in the presence of A and N, on the basis of which the cutoff for T positivity was defined. Finally, we assessed by imaging biomarkers the frequency of A/T/N profiles.
Methods
Subjects
Eighty-one subjects were included in the context of an ongoing study investigating the pathological bases of AD as displayed through advanced PET and magnetic resonance imaging (MRI) biomarkers. Subjects with subjective cognitive decline (SCD n = 16), mild cognitive impairment (MCI n = 57), and AD dementia (n = 8) were prospectively recruited in the Geneva Memory Center at Geneva University Hospitals. Inclusion criteria were (i) subjects older than 50 (ii) cognitive complaints [12], satisfaction of Petersen’s criteria for MCI [13] or probable AD [14]. The presence of psychiatric disorders or stigmata of vascular dementia represented exclusion criteria for this prospective study.
At baseline, all subjects underwent in-depth neurological evaluation and standard neuropsychological assessment in agreement with that included in IMI Pharmacog WP5/European ADNI, adapted from US ADNI [15] (for the battery of tests see http://www.centroalzheimer.org/sito/contenuti/download/pharmacog_battery.pdf).
MRI scan, amyloid and tau PET scans were acquired within a year from inclusion between March 2016 and June 2018. The local review board (Commission cantonale d’éthique de la recherche—CCER de Genève) approved the study, which has been conducted in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice. Each subject provided written informed consent for participation in the study.
Structural imaging data acquisition
Magnetic resonance imaging was performed at Geneva University Hospitals’ radiology department in 72 individuals, using a 3 Tesla Siemens Magnetom Skyra scanner, equipped with a 64-channel head coil. T1-weighted (3D sagittal acquisition, square FOV = 256 mm, slice thickness = 0.9 mm, TR/TE = 1930/2.4 ms, flip angle = 8°, no fat suppression) and fluid-attenuated inversion recovery (FLAIR, 3D sagittal acquisition, FOV = 256 mm, slice thickness = 1 mm, TR/TE/TI = 5000/386/1800 ms, flip angle = 120°) images were acquired corresponding to IMI Pharmacog WP5/European ADNI sequences and published procedures [16]. Nine subjects underwent MRI for clinical reasons before study inclusion with various protocols, all including T1 images, and imaging according to the exact ADNI parameters was not repeated in these cases. Images were stored on the hospital’s Picture Archiving and Communication System. Lesion Prediction Algorithm [17] (LPA), a fully automated algorithm implemented in Lesion Segmentation Toolbox (LST), was used to segment FLAIR images. LST allows extracting the number of white matter lesions, as well as overall lesion volume.
Amyloid PET data acquisition
PET scanning using [18-F] radioligands was performed at the nuclear medicine and molecular imaging division at Geneva University Hospitals using a Siemens Biograph mCT PET scanner. Aβ images were acquired using 18F-florbetapir (n = 64) or 18F-flutemetamol (n = 17) tracers. 18F-florbetapir images were acquired 50 min after the intravenous administration of 200 Mbq of the radiotracer (3 × 5-min image frames). For 18F-flutemetamol the injected radiotracer’s dose was 150 MBq and images were acquired 90 min after the time of injection (4 × 5-min image frames).
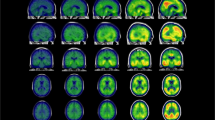
Tau PET data acquisition and preprocessing
18F-flortaucipir (18F-AV1451), synthesized at the Center for Radiopharmaceutical Sciences ETH-PSI-USZ in Zurich, Switzerland, under license from the IP owner (Avid/Lilly), was used for the tau PET scans. Subjects received 180 MBq of 18F-flortaucipir, with image acquisition performed 75 min after injection (acquisition time 30 min) [18]. Each emission frame was reconstructed in 6 × 5-min frames using a 3D OSEM iterative reconstruction (4 iterations, 12 subsets), corrected for randoms, dead time, normalization, scatter, attenuation, and sensitivity, and averaged after motion correction.
Tau-PET images were preprocessed using the SPM12 software package (Wellcome Department of Cognitive Neurology, London, UK) and MATLAB R2013a (MathWorks, Natick, MA, USA). For each subject, PET images were first rigidly co-registered to T1-weighted MRI scan images. The MRI images were spatially normalized into the Montreal Neurological Institute space to obtain the normalization matrix, which was then applied to the co-registered PET scans. Each individual image was smoothed with a 6-mm full-width at half-maximum Gaussian kernel with intensity normalization applied using the cerebellar crus as reference region [19] and data from specific regions of interest (ROIs) [20] were extracted using the automated anatomic labeling atlas [21].
Classification of A and N status
Criteria for N and A classification are summarized in Table 1. A positivity was determined in each patient by an expert in nuclear medicine (VG) using visual assessment and standard operating procedures approved from the European Medicines Agency (https://www.ema.europa.eu/documents/product-information/vizamyl-epar-product-information_en.pdf; https://www.ema.europa.eu/documents/product-information/amyvid-epar-product-information_en.pdf).
Depending on T1-weighted image availability, N status was defined by hippocampal volumetry and/or by visual assessment of medial temporal atrophy (MTA) following the 5-point Scheltens scale [22]. According to this scale, a score of 0 is assigned when no cerebrospinal fluid is seen surrounding the hippocampus, while a score of 4 represents severe atrophy of the medial temporal lobe with enlargement of the temporal horn and the choroid fissure. All subjects were classified according to the MTA scale, automated hippocampal volumetry was available in 72 subjects and was performed using ACM-AdaBoost software [23] on the neuGRID platform (www.neugrid2.eu) [24, 25]. Through this software, each hippocampal volume (left and right sides) was converted into an age-and-gender-normalized percentile [26]. For subjects without hippocampal volumetry (n = 9) N was defined through MTA. Three different age-corrected MTA cutoffs [27,28,29] and two different percentile-based cutoffs (i.e., at least one hippocampal volume < 5th percentile or at least one hippocampal volume < 10th percentile) were considered, and Cohen’s kappa agreement was computed in subjects with both measures to define the percentile-based and MTA cutoff with the highest agreement. The MTA cutoff proposed by Cotta Ramusino and colleagues [29] and ACM-Adaboost < 5th percentile showed the highest agreement (Cohen’s k = 0.60, 95% CI 0.40–0.79) compared to the others, thus these criteria were adopted to define N. Subjects with both hippocampal volumetry and MTA were classified according to the percentile-based cutoff method (see Table 1 for the adopted A and N criteria).
Statistical analyses
Differences in demographic and clinical features between A/N subgroups were assessed by ANOVA (Bonferroni post hoc test) for continuous variables, with non-parametric statistics used for variables not distributed normally (Kruskal-Wallis variance analysis and Mann-Whitney U test for post hoc comparisons, normality test: Kolmogorov-Smirnov), or chi-square/Fisher exact test (χ2) for categorical variables. In order to evaluate tau deposition in A/N subgroups, whole-brain analyses were performed using SPM12 software package by computing two-sample t tests on normalized SUVR PET images, in order to compare degrees of 18F-flortaucipir tracer retention in A/N subgroups (p < 0.001 uncorrected at the voxel level, k = 100, p < 0.05 FWE-corrected at the cluster level). Considering the possible interaction between tau burden and age [30], this was added as a nuisance variable.
Subsequently, a global SUVR score was computed as the average uptake of specific regions according to previous literature recommendations (i.e., medio-temporal regions, lateral occipital cortex, inferior temporal cortex) [20]. In order to assess the association between tau deposition with clinical status, non-parametric correlation analyses between MMSE and global SUVR score were performed (Spearman’s rho) in the overall sample.
Finally, for subgroups showing significant differences in 18F-flortaucipir retention in comparison to A−N− subjects, receiver operator characteristic (ROC) curve analyses were performed, in order to compute a global cutoff score, then used to classify subjects according to T positivity and to assess the frequency of different A/T/N subgroups.
Results
Classification of subjects according to the A/N status
Subjects were classified according to A and N biomarkers as 24 A−N−, 29 A+N−, 10 A−N+, and 18 A+N+ (see Table 2 for demographic and clinical features). The frequency of A and N positivity was significantly different across syndromic diagnoses (Fisher’s exact test X2 = 19.16, p = 0.005) and higher in subjects with MCI and AD dementia, as shown in Table 2. Seventy-two percent of SCD subjects were N− and all AD dementia patients were A+ by definition. 61% of MCI patients were A+, while only 34% were classified as N+. No significant difference on demographic variables was found between A/N subgroups. However, the A+N+ subgroup showed a higher level of global cognitive impairment in comparison to the other subgroups (Table 2), as assessed by the MMSE global score (F(3,77) = 9.91, p < 0.001).
18F-flortaucipir distribution in A/N subgroups
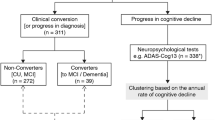
The two-sample t tests on whole-brain analyses showed higher tau burden in A+ subgroups (i.e., A+N− and A+N+). In particular, compared to A−N−, A+N+ subjects showed a widespread tau deposition in bilateral medial and lateral temporal lobes, in the retrosplenial/posterior cingulate cortex, in parietal, frontal, and occipital regions (Fig. 1a). The comparison between A−N− and A+N− revealed an elevated uptake in the latter subgroup, but restricted to the bilateral medial and lateral temporal regions (Fig. 1b). Moreover, A+N+ subjects showed a higher 18F-flortaucipir uptake compared to the A-N+ subgroup in a right temporal cluster including the fusiform gyrus, the inferior, middle, and superior temporal gyri, as well as in the left inferior temporal gyrus (Fig. 1c).
A/T/N classification
The global SUVR index computed according to previous literature [20] showed a significant negative correlation with clinical status (MMSE and global SUVR Spearman’s rho = − 0.34, p = 0.002). Moreover, the ROC curve analyses indicated an excellent discriminability of global SUVR in comparing A+N+ from A−N− subjects (area under the curve AUC = 0.84, SE = 0.07, p < 0.001, CI 95% 0.70–0.98) but lower discriminative power when comparing A+N− to A−N− subjects (AUC = 0.74, SE = 0.07, p = 0.003, CI 95% 0.60–0.87). A cutoff of 1.24 had 78% sensitivity and 79% specificity in distinguishing A+N+ from A−N−, and 51% of sensitivity (specificity 79%) in classifying A+N− from A−N−.
The A/T/N classification using the global SUVR cutoff score showed that the profiles most frequently observed in our sample were those in accordance with the amyloid cascade hypothesis (A−T−N− 23%, A+T−N− 16%; A+T+N− 20% or A+T+N+ 17%). A-subjects positive for either N or T comprised 19% of the overall sample (A−T−N+ 9%, A−T+N+ 4%, A−T+N− 6%) (Fig. 2).
The frequency of T+ subjects differed in A−N− compared to the other A+ subgroups (A+N+ X2 (1) = 14.9, p < 0.001; A+N− X2 (1) = 7.5, p = 0.006) while no differences were found with the A−N+ subgroup (X2 (1) = 0.48, p = 0.49).
Discussion
After the publication of the A/T/N research framework in 2018 [2], the application of this biomarker-based system in both healthy aging and clinical population has grown. The available studies adopting this classification on memory clinic patients mainly used cerebrospinal fluid analysis to define N (i.e., overall tau) and/or T status (i.e., p-tau) [6, 8]. Thus, to the best of our knowledge, this is the first observational study in which the A/T/N status is assessed using imaging biomarkers in a sample of patients prospectively enrolled in a memory clinic.
Patients were initially characterized according to the A/N status. The whole-brain analyses comparing tau deposition in A/N subgroups showed a widespread tau deposition in A+N+ subjects, as compared to those with an A−N− profile, in temporo-limbic as well as in neocortical regions, while in A+N− subjects the significantly increase in tau burden involved bilateral medial and lateral temporal regions. These results are in line with the predominant AD biomarker model proposing a facilitating role of Aβ aggregation in disease progression [31,32,33,34,35,36,37], and identify medial and lateral temporal regions as early area of tau accumulation in A+ subjects without structural hippocampal neurodegeneration.
Despite the effect of tau-pathology on cognitive symptoms in subjects classified as N− is to be fully elucidated, recent evidence highlighted significant tau-related network derangements [38] prior than frank neurodegeneration, suggesting a possible direct effect of tau-pathology on clinical symptoms, together with a neurodegenerative-mediated one [39, 40]. Thus, tau accumulation in temporal regions in A+ subjects might represent a useful early marker of clinical changes in patients with a still undetectable pattern of structural neurodegeneration. However, further studies including other N biomarkers (e.g., global or parietal atrophy, FDG-PET hypometabolism) are required to test this hypothesis. Patients with atypical presentation might indeed show early neurodegeneration in brain regions other than the medial temporal lobe, and the choice of this region might have limited the sensitivity in detecting N. However, we opted for this definition to be consistent with previous studies on A/T/N that considered visual [6] or automated [7, 9, 41] measures of temporal atrophy as index of neurodegeneration, and to overcome the lack of other validated measures of cortical volumetry, as well as the low diagnostic value of existing visual scales [28, 42].
Following a binary approach as envisioned by the A/T/N model, we also computed a T-based cut point to classify patients according to tau positivity. This score was found to be only moderately associated to global cognitive functions. One explanation could be the high prevalence of MCI in our sample (70%), possibly including other etiologies than AD. It should be noted that we used a global SUVR index to assess T, while regional measures and analyses taking into account other variables affecting cognition, namely age or education, observed a higher association between 18F-flortaucipir load and cognitive status [43].
According to the A/T/N classification, 23% of the overall sample was classified as A−T−N, and 58% showed a biomarker profile in the Alzheimer’s continuum (i.e., abnormal amyloid regardless of tau status, according to the research framework recently proposed [2]). These percentages, as well as those for each subgroup, well overlap with the results of a recent study including 305 memory clinic patients evaluated trough CSF and imaging biomarkers of AD pathology (22% A−T−N− and 49% in the Alzheimer’s continuum) [6].
On the other hand, they slightly differ from those of another study [9] investigating the A/T/N distribution through imaging biomarkers, in which 29% of the sample was classified as A−T−N−, and a biomarker profile following the Alzheimer’s continuum was described only in 42% of subjects. The relative discrepancy between these data can be probably explained taking into consideration the different study design (population-based vs memory clinic patients). Even if the A/T/N research framework should not be considered as the only template in the investigation of age-related cognitive impairment and dementia, and it is not intended to be used in general medical practice as clinical guidelines [2, 44], patient classification according to this model might provide important information in the definition of the clinical trajectory and in the design of disease-modifying clinical trials. In fact, biologically defined AD, as proposed by the NIA-AA research framework [2], showed a higher prevalence compared to the conventional definitions based on clinical symptoms [45]. Thus, a biomarker-based definition of AD might represent a crucial step in the development of future clinical trials, particularly in the preclinical phase.
Overall, recent studies evaluating the progression of different A/T/N profiles showed a clinical stability at 8 years in A− patients positive to other biomarkers, suggesting a somewhat benign clinical trajectory [5]. On the other hand, both A+T+N− and A+T+N+ groups show a relevant cognitive decline at longitudinal follow-up [6, 9]. In addition to this evidence, our results suggest that the detection of significant tau deposition in medial and lateral temporal regions characterizing A+N− patients could thus represent an important marker in the early detection of patients at risk of clinical progression.
A longitudinal evaluation is not yet available in these patients and does not allow testing this hypothesis. However, the present cohort will be followed prospectively to evaluate clinical and biomarker trajectories.
Finally, in our sample, 19% of patients showed an A− profile, despite being positive on one or both T and N biomarkers. The prevalent neuropathological model of AD disease progression, postulating that Aβ deposition leads to tau aggregation and neurodegeneration (i.e., synaptic dysfunction and/or brain atrophy), has been recently questioned by the discovery of subjects with an abnormal N [4] and/or T [46] status, despite a normal amyloid burden. Even though widespread neocortical tau deposits were almost exclusively observed in A+ individuals, literature shows evidence of possible tau deposits in mesial temporal regions in amyloid negative cases [46], and previous PET-based studies showed that a minor percentage of A− subjects might present tau deposition beyond the medial temporal lobe [35, 47]. However, consistently with the results of previous analyses at group level [48], we found no significant tau increase in our A−N+ sample when comparing regional tau burden with other A/N subgroups. Subjects with A− profile and positive on one or both T and N biomarkers might then be characterized by heterogeneous disease etiologies, including both tau-related diseases (primary age-related tauopathy [46] or other tauopathies [49]) and non-tau related conditions (e.g., limbic-predominant age-related TDP-43 encephalopathy [50]) mimicking AD clinical symptoms, as well as alpha-synuclein pathology [51]. The longitudinal follow-up will permit to evaluate the progression of A/T/N profiles, as well as the possible presence of false positive and negative cases, which can derive by the definition of a binary threshold. In particular, studying the evolution of subjects with A−T+N− and A−T+N+ profiles will help understanding whether they represent a distinct pathological entity or an alternative AD pathway, and will allow measuring the prognostic value of A, T, and N positivity.
Our study has some limitations worth mentioning. Despite the relatively large population included in this study, the identification of 8 different A/T/N profiles led to the definition of subgroups with a limited number of subjects. The other two major limitations are represented by the lack of pathological confirmation and information on hippocampal volumetry for some subjects due to multiple T1-weighted imaging protocols. These methodological constraints could have limited our sensitivity. Besides, the global SUVR cut point equal to 1.24 used in the current study, although falling within the range reported in previous literature (1.19–1.27) [9, 11, 20, 52] and effectively distinguishing A+N+ from A−N− subjects, showed only a limited sensitivity in A+N− subjects (51%). Even though previous evidence failed in providing substantial changes in the A/T/N prevalence using different reference regions [45], future studies should be aimed at investigating the utility of different cut points and regions of interests based on the clinical stage (i.e., earliest versus advanced stages on the AD pathway).
In conclusion, in this observational study, we characterized for the first time a memory clinic population adopting the A/T/N model using PET- and MRI-based biomarkers, providing evidence of higher tau tracer retention in A+ subjects and a heterogeneous picture in patients characterized by an A− profile. In A+ subjects, tau deposition in lateral temporal regions assessed through tau PET might represent a useful marker in the early detection of clinical changes. These findings are consistent with the stages proposed by Braak to describe the progression of tau-pathology [53], starting from medial temporal regions, and then spreading to lateral temporal and other neocortical areas. Besides, the unbalance between the frequency of A+T+N− (20%) and A+T−N+ (5%) further supports the current view that tau deposition is a required substrate for AD neurodegeneration.
Overall, the comparison of A/T/N frequencies between population samples with overlapping features represents an important step to possibly incorporate this research system into clinical practice.
References
Jack CR Jr, Bennett DA, Blennow K, Carrillo MC, Feldman HH, Frisoni GB, et al. A/T/N: an unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology. 2016;87:539–47. https://doi.org/10.1212/WNL.0000000000002923.
Jack CR Jr, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14:535–62. https://doi.org/10.1016/j.jalz.2018.02.018.
Jack CR Jr, Albert MS, Knopman DS, McKhann GM, Sperling RA, Carrillo MC, et al. Introduction to the recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:257–62. https://doi.org/10.1016/j.jalz.2011.03.004.
Jack CR Jr, Knopman DS, Chetelat G, Dickson D, Fagan AM, Frisoni GB, et al. Suspected non-Alzheimer disease pathophysiology--concept and controversy. Nat Rev Neurol. 2016;12:117–24. https://doi.org/10.1038/nrneurol.2015.251.
Soldan A, Pettigrew C, Fagan AM, Schindler SE, Moghekar A, Fowler C, et al. ATN profiles among cognitively normal individuals and longitudinal cognitive outcomes. Neurology. 2019;92:e1567–e79. https://doi.org/10.1212/WNL.0000000000007248.
Altomare D, de Wilde A, Ossenkoppele R, Pelkmans W, Bouwman F, Groot C, et al. Applying the ATN scheme in a memory clinic population: The ABIDE project. Neurology. 2019;93:e1635-e46. doi: https://doi.org/10.1212/WNL.0000000000008361
Jack CR Jr, Wiste HJ, Weigand SD, Therneau TM, Knopman DS, Lowe V, et al. Age-specific and sex-specific prevalence of cerebral beta-amyloidosis, tauopathy, and neurodegeneration in cognitively unimpaired individuals aged 50-95 years: a cross-sectional study. Lancet Neurol. 2017;16:435–44. https://doi.org/10.1016/S1474-4422(17)30077-7.
Ekman U, Ferreira D, Westman E. The A/T/N biomarker scheme and patterns of brain atrophy assessed in mild cognitive impairment. Sci Rep. 2018;8:8431. https://doi.org/10.1038/s41598-018-26151-8.
Jack CR Jr, Wiste HJ, Therneau TM, Weigand SD, Knopman DS, Mielke MM, et al. Associations of amyloid, tau, and neurodegeneration biomarker profiles with rates of memory decline among individuals without dementia. Jama. 2019;321:2316–25. https://doi.org/10.1001/jama.2019.7437.
Noirot C, Mainta I, Mendes A, Andryszak P, Visvaratnam H, Unschuld PG, et al. Tau PET imaging evidence in patients with cognitive impairment: preparing for clinical use. Clinical and Translational Imaging. 2018;6:471–82. https://doi.org/10.1007/s40336-018-0297-4.
Ossenkoppele R, Rabinovici GD, Smith R, Cho H, Scholl M, Strandberg O, et al. Discriminative accuracy of [18F] flortaucipir positron emission tomography for Alzheimer disease vs other neurodegenerative disorders. Jama. 2018;320:1151–62. https://doi.org/10.1001/jama.2018.12917.
Jessen F, Amariglio RE, van Boxtel M, Breteler M, Ceccaldi M, Chetelat G, et al. A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer’s disease. Alzheimers Dement. 2014;10:844–52. https://doi.org/10.1016/j.jalz.2014.01.001.
Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256:183–94. https://doi.org/10.1111/j.1365-2796.2004.01388.x.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–9. https://doi.org/10.1016/j.jalz.2011.03.005.
Frisoni GB, Prestia A, Zanetti O, Galluzzi S, Romano M, Cotelli M, et al. Markers of Alzheimer’s disease in a population attending a memory clinic. Alzheimers Dement. 2009;5:307–17. https://doi.org/10.1016/j.jalz.2009.04.1235.
Jovicich J, Marizzoni M, Sala-Llonch R, Bosch B, Bartres-Faz D, Arnold J, et al. Brain morphometry reproducibility in multi-center 3T MRI studies: a comparison of cross-sectional and longitudinal segmentations. Neuroimage. 2013;83:472–84. https://doi.org/10.1016/j.neuroimage.2013.05.007.
Schmidt P. Bayesian inference for structured additive regression models for large-scale problems with applications to medical imaging: lmu; 2017.
Shcherbinin S, Schwarz AJ, Joshi A, Navitsky M, Flitter M, Shankle WR, et al. Kinetics of the tau PET tracer 18F-AV-1451 (T807) in subjects with normal cognitive function, mild cognitive impairment, and Alzheimer disease. J Nucl Med. 2016;57:1535–42. https://doi.org/10.2967/jnumed.115.170027.
Schwarz AJ, Shcherbinin S, Slieker LJ, Risacher SL, Charil A, Irizarry MC, et al. Topographic staging of tau positron emission tomography images. Alzheimers Dement (Amst). 2018;10:221–31. https://doi.org/10.1016/j.dadm.2018.01.006.
Mishra S, Gordon BA, Su Y, Christensen J, Friedrichsen K, Jackson K, et al. AV-1451 PET imaging of tau pathology in preclinical Alzheimer disease: defining a summary measure. Neuroimage. 2017;161:171–8. https://doi.org/10.1016/j.neuroimage.2017.07.050.
Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage. 2002;15:273–89. https://doi.org/10.1006/nimg.2001.0978.
Scheltens P, Leys D, Barkhof F, Huglo D, Weinstein HC, Vermersch P, et al. Atrophy of medial temporal lobes on MRI in “probable” Alzheimer’s disease and normal ageing: diagnostic value and neuropsychological correlates. J Neurol Neurosurg Psychiatry. 1992;55:967–72.
Morra JH, Tu Z, Apostolova LG, Green AE, Avedissian C, Madsen SK, et al. Validation of a fully automated 3D hippocampal segmentation method using subjects with Alzheimer’s disease mild cognitive impairment, and elderly controls. Neuroimage. 2008;43:59–68. https://doi.org/10.1016/j.neuroimage.2008.07.003.
Frisoni GB, Redolfi A, Manset D, Rousseau ME, Toga A, Evans AC. Virtual imaging laboratories for marker discovery in neurodegenerative diseases. Nat Rev Neurol. 2011;7:429–38. https://doi.org/10.1038/nrneurol.2011.99.
Redolfi A, McClatchey R, Anjum A, Zijdenbos A, Manset D, Barkhof F, et al. Grid infrastructures for computational neuroscience: the neuGRID example. Future Neurol. 2009;4:703–22.
Bosco P, Redolfi A, Bocchetta M, Ferrari C, Mega A, Galluzzi S, et al. The impact of automated hippocampal volumetry on diagnostic confidence in patients with suspected Alzheimer’s disease: a European Alzheimer’s disease consortium study. Alzheimers Dement. 2017;13:1013–23. https://doi.org/10.1016/j.jalz.2017.01.019.
Pereira JB, Cavallin L, Spulber G, Aguilar C, Mecocci P, Vellas B, et al. Influence of age, disease onset and ApoE4 on visual medial temporal lobe atrophy cut-offs. J Intern Med. 2014;275:317–30. https://doi.org/10.1111/joim.12148.
Rhodius-Meester HFM, Benedictus MR, Wattjes MP, Barkhof F, Scheltens P, Muller M, et al. MRI visual ratings of brain atrophy and white matter hyperintensities across the spectrum of cognitive decline are differently affected by age and diagnosis. Front Aging Neurosci. 2017;9:117. https://doi.org/10.3389/fnagi.2017.00117.
Cotta Ramusino M, Altomare D, Bacchin R, Ingala S, Bna C, Bonetti M, et al. Medial temporal lobe atrophy and posterior atrophy scales normative values. Neuroimage Clin. 2019;24:101936. doi: https://doi.org/10.1016/j.nicl.2019.101936
Pontecorvo MJ, Devous MD Sr, Navitsky M, Lu M, Salloway S, Schaerf FW, et al. Relationships between flortaucipir PET tau binding and amyloid burden, clinical diagnosis, age and cognition. Brain. 2017;140:748–63. https://doi.org/10.1093/brain/aww334.
Jack CR Jr, Knopman DS, Jagust WJ, Petersen RC, Weiner MW, Aisen PS, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207–16. https://doi.org/10.1016/S1474-4422(12)70291-0.
Blurton-Jones M, Laferla FM. Pathways by which Abeta facilitates tau pathology. Curr Alzheimer Res. 2006;3:437–48.
Tosun D, Landau S, Aisen PS, Petersen RC, Mintun M, Jagust W, et al. Association between tau deposition and antecedent amyloid-beta accumulation rates in normal and early symptomatic individuals. Brain. 2017;140:1499–512. https://doi.org/10.1093/brain/awx046.
Scholl M, Ossenkoppele R, Strandberg O, Palmqvist S, Swedish Bio F, Jogi J, et al. Distinct 18F-AV-1451 tau PET retention patterns in early- and late-onset Alzheimer’s disease. Brain. 2017;140:2286–94. https://doi.org/10.1093/brain/awx171.
Maass A, Landau S, Baker SL, Horng A, Lockhart SN, La Joie R, et al. Comparison of multiple tau-PET measures as biomarkers in aging and Alzheimer’s disease. Neuroimage. 2017;157:448–63. https://doi.org/10.1016/j.neuroimage.2017.05.058.
Brier MR, Gordon B, Friedrichsen K, McCarthy J, Stern A, Christensen J, et al. Tau and Abeta imaging, CSF measures, and cognition in Alzheimer’s disease. Sci Transl Med. 2016;8:338ra66. https://doi.org/10.1126/scitranslmed.aaf2362.
Bischof GN, Jessen F, Fliessbach K, Dronse J, Hammes J, Neumaier B, et al. Impact of tau and amyloid burden on glucose metabolism in Alzheimer’s disease. Ann Clin Transl Neurol. 2016;3:934–9. https://doi.org/10.1002/acn3.339.
Menkes-Caspi N, Yamin HG, Kellner V, Spires-Jones TL, Cohen D, Stern EA. Pathological tau disrupts ongoing network activity. Neuron. 2015;85:959–66. https://doi.org/10.1016/j.neuron.2015.01.025.
Bejanin A, Schonhaut DR, La Joie R, Kramer JH, Baker SL, Sosa N, et al. Tau pathology and neurodegeneration contribute to cognitive impairment in Alzheimer’s disease. Brain. 2017;140:3286–300. https://doi.org/10.1093/brain/awx243.
Saint-Aubert L, Almkvist O, Chiotis K, Almeida R, Wall A, Nordberg A. Regional tau deposition measured by [(18)F]THK5317 positron emission tomography is associated to cognition via glucose metabolism in Alzheimer’s disease. Alzheimers Res Ther. 2016;8:38. https://doi.org/10.1186/s13195-016-0204-z.
Roberts RO, Knopman DS, Syrjanen JA, Aakre JA, Vassilaki M, Kremers WK, et al. Weighting and standardization of frequencies to determine prevalence of AD imaging biomarkers. Neurology. 2017;89:2039–48. https://doi.org/10.1212/WNL.0000000000004652.
Ferreira D, Cavallin L, Larsson EM, Muehlboeck JS, Mecocci P, Vellas B, et al. Practical cut-offs for visual rating scales of medial temporal, frontal and posterior atrophy in Alzheimer’s disease and mild cognitive impairment. J Intern Med. 2015;278:277–90. https://doi.org/10.1111/joim.12358.
Cho H, Choi JY, Hwang MS, Lee JH, Kim YJ, Lee HM, et al. Tau PET in Alzheimer disease and mild cognitive impairment. Neurology. 2016;87:375–83. https://doi.org/10.1212/WNL.0000000000002892.
Khachaturian AS, Hayden KM, Mielke MM, Tang Y, Lutz MW, Gustafson DR, et al. Future prospects and challenges for Alzheimer’s disease drug development in the era of the NIA-AA research framework. Alzheimers Dement. 2018;14:532–4. https://doi.org/10.1016/j.jalz.2018.03.003.
Jack CR Jr, Therneau TM, Weigand SD, Wiste HJ, Knopman DS, Vemuri P, et al. Prevalence of biologically vs clinically defined Alzheimer spectrum entities using the National Institute on Aging-Alzheimer’s Association research framework. JAMA Neurol. 2019. https://doi.org/10.1001/jamaneurol.2019.1971.
Crary JF, Trojanowski JQ, Schneider JA, Abisambra JF, Abner EL, Alafuzoff I, et al. Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol. 2014;128:755–66. https://doi.org/10.1007/s00401-014-1349-0.
Scholl M, Lockhart SN, Schonhaut DR, O’Neil JP, Janabi M, Ossenkoppele R, et al. PET imaging of tau deposition in the aging human brain. Neuron. 2016;89:971–82. https://doi.org/10.1016/j.neuron.2016.01.028.
Mormino EC, Papp KV, Rentz DM, Schultz AP, LaPoint M, Amariglio R, et al. Heterogeneity in suspected non-Alzheimer disease pathophysiology among clinically normal older individuals. JAMA Neurol. 2016;73:1185–91. https://doi.org/10.1001/jamaneurol.2016.2237.
Lee VM, Goedert M, Trojanowski JQ. Neurodegenerative tauopathies. Annu Rev Neurosci. 2001;24:1121–59. https://doi.org/10.1146/annurev.neuro.24.1.1121.
Nelson PT, Dickson DW, Trojanowski JQ, Jack CR, Boyle PA, Arfanakis K, et al. Limbic-predominant age-related TDP-43 encephalopathy (LATE): consensus working group report. Brain. 2019. https://doi.org/10.1093/brain/awz099.
Goedert M. Alpha-synuclein and neurodegenerative diseases. Nat Rev Neurosci. 2001;2:492–501. https://doi.org/10.1038/35081564.
Wang L, Benzinger TL, Su Y, Christensen J, Friedrichsen K, Aldea P, et al. Evaluation of tau imaging in staging Alzheimer disease and revealing interactions between beta-amyloid and tauopathy. JAMA Neurol. 2016;73:1070–7. https://doi.org/10.1001/jamaneurol.2016.2078.
Braak H, Braak E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 1991;82:239–59.
Acknowledgments
We thank all patients and volunteers for participating in this study. We thank Avid Radiopharmaceuticals (Lilly) for supplying the precursor for the manufacturing of 18F-flortaucipir.
Funding
The study has been supported by the Swiss National Science Foundation (“The Biological Basis of Cognitive Impairment due to SNAP: Studying the interplay between amyloidosis and tau-related neurodegeneration”—SNF 320030_169876) and partially supported by the Personalized Health and Related Technology Initiative (“Advanced Translational Imaging”—PHRT 2017-512).
This study is part of CoSTREAM (www.costream.eu) and received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement no. 667375.
The Centre de la mémoire at Geneva University Hospital is funded by private donors: A.P.R.A.—Association Suisse pour la Recherche sur la Maladie d’Alzheimer, Genève; Fondation Segré, Genève; Ivan Pictet, Genève; Fondazione Agusta, Lugano; Fondation Chmielewski, Genève.
Author information
Authors and Affiliations
Contributions
Study concept and design: Dodich, Frisoni, Garibotto. Clinical consultant and data acquisition: Mendes, Assal, Chicherio, Rakotomiaramanana, Andryszak, Sheffler, Zekry, Lovblad. Statistical analysis and data interpretation: Dodich, Festari, Ribaldi, Frisoni, Garibotto. Drafting of the manuscript: Dodich, Garibotto. All the authors contributed to the critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and consent to participate
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee (Commission cantonale d’éthique de la recherche—CCER)) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All subjects participating in this study have signed an informed consent form.
Data policy
The datasets generated during and/or analyzed during the current study are part of the Geneva Memory Clinic dataset and available from the corresponding author on founded request.
Consent for publication
The manuscript has been seen and approved by all authors for submission to EJNMMI.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurology
Rights and permissions
About this article
Cite this article
Dodich, A., Mendes, A., Assal, F. et al. The A/T/N model applied through imaging biomarkers in a memory clinic. Eur J Nucl Med Mol Imaging 47, 247–255 (2020). https://doi.org/10.1007/s00259-019-04536-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04536-9