Abstract
Purpose
Rectal neuroendocrine neoplasia (NEN) is more common than other NEN origins, but is less commonly metastatic. However, when present, distant disease carries a particularly poor prognosis. Evidence guiding optimal treatment of such patients is lacking. We assessed PRRT outcomes in patients with somatostatin receptor (SSTR) positive metastatic rectal NEN from two referral centres.
Methods
Patients treated with PRRT were retrospectively reviewed. Morphologic (RECIST 1.1), SSTR imaging responses and toxicity were assessed 3 months post-PRRT. Kaplan-Meier estimate was used to determine progression-free survival (PFS) and overall survival (OS) from start of PRRT.
Results
Twenty-seven consecutive patients (M = 20, age 31-81 years) were reviewed. The majority (70%) had ENETs grade 2 disease (19 patients), three had Grade 3, one Grade 1, and four not documented. Overall, 63% (10/16 patients with available FDG PET/CT) had FDG avid disease. Twenty-six patients were treated for disease progression. Most had 177Lu-DOTA-octreotate with median cumulative activity of 30 GBq, median four cycles. 14 patients had radiosensitising chemotherapy (5FU or capecitabine). At 3 months post-PRRT, CT disease control rate (DCR) was 96%: partial response was observed in 70% (19/27) and stable disease in 26%. All but one had partial SSTR imaging response. The median PFS was 29 months. Ten patients died, with median overall survival 81 months with a median follow-up of 67 months. Seventeen patients had further treatments after initial PRRT (10 had further cycles of PRRT). Three patients had grade 3 lymphopenia, without significant renal toxicity, MDS or leukaemia.
Conclusion
Our results indicate high efficacy and morphologic responses with minimal toxicity and very encouraging survival from PRRT in patients with metastatic rectal NEN despite the adverse prognostic features of this cohort. Further prospective PRRT trials are warranted in this subgroup.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine neoplasia (NEN) represents a heterogeneous group of tumours arising from the diffuse endocrine system. Tumour grade is currently categorised into three subgroups according to the 2010 WHO and ENETS classifications [1, 2], where Grade 3 disease (Ki67 > 20%) has the worst prognosis [3, 4]. The incidence of NEN has increased worldwide affecting most anatomical sites and involving both low and high grade neoplasms [5]. Of the many potential sites of origin, the rectum comprises 14–29% of gastroenteropancreatic (GEP) NEN [6, 7], and exhibits the greatest relative increase in incidence [8]. The majority of rectal NEN are, however, diagnosed incidentally at colonoscopy. These mostly comprise of small submucosal (<1-2 cm), low to intermediate grade (Grade 1 or 2) lesions, which rarely metastasize and generally have favourable prognoses [9, 10]. Localised and regional diseases have favourable 5-year overall survivals of 90 and 62%, respectively [11]. While distant metastases are uncommon at diagnosis (between 2 and 8%) [11], these patients have a worse prognosis with a 5-year survival of only 24% [11, 12], and a median survival of 10.4 months [10]. Prognosis is worse for metastatic colonic compared with rectal NEN (7 vs. 26 months, respectively) [11]. Whilst about 30% of GEP NENs are functional causing hormone-hypersecretion related symptoms, it is unusual for rectal tumours to be hormone-hypersecreting or to cause carcinoid syndrome [10].
There has been significant progress in the management of metastatic Grade 1 and 2 GEP NEN over recent years as a result of several published phase III trials [13]. However, evidence specific for metastatic rectal NEN is very limited, mainly due to its low occurrence relative to other NEN origins. Given the poor overall prognosis, further studies to establish effective treatments options are required for patients with metastatic rectal NEN. Somatostatin analogues (SSAs) may have an anti-proliferative effect, but the small number of colorectal NEN cases in the recent Phase III CLARINET study provided insufficient evidence in this group [14]. Systemic chemotherapy has little role in G1 and G2 NEN, but may be appropriate for high grade G3 or progressive disease [10, 13]. Options include cisplatin (or carboplatin) plus etoposide, oxaliplatin-based (XELOX, FOLFOX), irinotecan-based (FOLFIRI), or temozolomide-based regimes [15], but data for rectal NEN is lacking. The RADIANT-2 study using everolimus and octreotide showed improved progression-free survival compared to placebo plus octreotide for well-differentiated NEN with carcinoid syndrome, but the use for colorectal NEN remains to be verified [16].
Most well-to-moderately differentiated NEN retain high expression of somatostatin receptors (SSTR), a characteristic that can be identified by molecular imaging and targeted for treatment with radiolabelled somatostatin receptor analogue therapy. Peptide receptor radionuclide therapy (PRRT) has been shown to be highly effective in treatment for SSTR positive GEP NEN, with minimal toxicity [17, 18]. The response rates from PRRT based on relatively large international clinical experiences generally compare favourably with those obtained with chemotherapy, and are generally substantially higher than reported with targeted agents including everolimus and sunitinib [17], despite the lack of prospective trials. In this study, we aim to retrospectively review the therapeutic response, associated toxicity, and long-term outcome in patients with metastatic SSTR positive rectal NENs treated with PRRT from two referral centres.
Materials and methods
Patients
A total of 27 consecutive patients (M:F = 20:7; 31–81 years) with unresectable metastatic rectal NEN who received at least one cycle of 177Lu-DOTA-Octreotate (177Lu-DOTATATE) PRRT from two referral centres with at least 3 months follow-up from completion of PRRT, were retrospectively reviewed. Patients were followed up to death or study close-out date of 31st March 2018.
The primary objective was to assess morphologic response (RECIST 1.1) at 3 months post completion of induction PRRT. Secondary objectives included assessment of molecular imaging, biochemical responses and toxicity at 3 months post PRRT, and assessment of progression-free survival (PFS), overall survival (OS) and time to next treatment (TNT) from start of PRRT. Differences in patient outcome (PFS and OS) were compared for patients treated with radiosensitising chemotherapy versus without radiosensitising chemotherapy.
Eligibility for PRRT included lesions with high somatostatin receptor-expressing disease on Ga-68 DOTATATE PET/CT scan where the intensity of tumour uptake is greater than that of normal hepatic parenchyma at all sites of disease, together with evidence of progressive disease within 12 months, as assessed by combination of increasing biochemical marker (CgA), and new or enlarging lesions on SSTR PET/CT imaging, contrast-enhanced CT, or MRI, or symptoms despite conventional management.
Patients were excluded from PRRT if disease demonstrated low SSTR expression (uptake less than background liver activity), 18F-FDG-avid lesions showing low or absent SSTR analogue avidity (spatially discordant FDG+ and SSTR- scan pattern), hypoalbuminemia (<25 g/L), thrombocytopenia (<50 × 109/L for the Australian centre, <70 × 109/L for Israeli centre), pancytopaenia (haemoglobin <10 g/dL and white cell count <3 × 109/L for Israeli center), ECOG performance score 4, expected survival <3 months, or confirmed pregnancy.
All patients from Peter MacCallum Cancer Centre were treated on compassionate grounds under Special Access Scheme (SAS), which allows treatment of patients with life-threatening diseases with experimental therapies that have demonstrated efficacy in other studies. The use of SAS provisions was approved by the institutional ethics committee and all patients provided written informed consent to undergo treatment and follow-up. Institutional ethics committee approval for the follow-up of NEN patients was given at the Peter MacCallum Cancer Centre. The Israeli Ministry of Health approves PRRT treatment for patients with metastatic progressive neuroendocrine tumours and the study was approved by the Hadassah-Hebrew University Medical Center institutional ethical committee.
Treatment regimen
Radio-labelling and administration of 177Lu-DOTATATE were performed under local institutional protocol. At Peter MacCallum Cancer Centre, 177Lu produced from Europe (IDB Holland) was transported as a radiochemical, then labelled to the peptide octreotate (Erasmus Medical Center, Rotterdam, Holland) through chelation to a DOTA molecule forming 177Lu-DOTA-Octreotate. 90Yttrium provided by Perkin Elmer, Waltham, WA was labelled onto DOTA-octreotate (Auspep, Victoria, Australia) to form 90Y-DOTA-Octreotate. At Hadassah-Hebrew University Medical Center, 177Lu produced by PerkinElmer, Inc., USA was transported as a radiochemical, then labelled to the peptide octreotate (Isorad Ltd., Israel) again, through chelation to a DOTA molecule forming 177Lu-DOTA-Octreotate.
Each cycle of PRRT was administered with premedication granisetron 2 mg, dexamethasone 8 mg, and renoprotective amino-acid infusion (25 g lysine and 25 g arginine in 1 L normal saline) commencing 30 min prior to PRRT and continuing for 3 h thereafter. The induction treatment regimen typically included four cycles of 177Lu-DOTATATE given 6–10 weeks apart. At Peter MacCallum Cancer Centre, patients with bulky tumours >4 cm will be considered for 90Y-DOTA-Octreotate (followed by 177Lu-DOTATATE) based on previous experience showing that bulky disease is an adverse prognostic factor for response to 177Lu-DOTATATE PRRT [19, 20]. The 2nd to 4th cycles of 177Lu-DOTATATE were usually given with radiosensitising chemotherapy, unless contraindicated. This is based on prior experiences showing enhanced efficacy without additional toxicity [21,22,23]. An earlier protocol used infusional fluorouracil (5-FU) as a radiosensitiser (typically 200 mg/m2 daily, starting 2 days prior to PRRT for 2 weeks in total). Subsequent regimen per local institutional protocol included the use of oral capecitabine (825 mg/m2 bd commencing 2 days prior to PRRT for 2 weeks).
Follow-up
Patients were clinically reviewed prior to, and after, each cycle of PRRT and typically at 3 months following the last cycle of treatment. Evaluation at 3 months included assessment of symptoms, molecular imaging by 68Ga-DOTATATE PET/CT scan, and CT. Biochemical marker serum chromogranin A (CgA) was reviewed. Symptomatic benefit was defined as an improvement in tumour-related symptoms based on patients’ subjective report relative to baseline symptoms. Biochemical response was assessed by comparing serum CgA before and 3 months after PRRT as percentage change from baseline. Molecular imaging: Descriptor for pathologic uptake on 68Ga-DOTATATE PET/CT scan has been adapted from a semi-quantitative visual scoring system originally designed for planar 111In-octreotide imaging known as the Krenning score, consisting of a scale from 0 to 4 using liver and spleen as reference organs (Score 0 = no uptake; 1 = very low uptake, less than background liver activity; 2 = lesion uptake similar to liver activity; 3 = greater than liver; 4 = greater than spleen) [24]. 68Ga-DOTATATE PET/CT scan response was defined as stable, partial response (reduction in intensity by one Krenning score in at least one tumour site), complete response (total disappearance of abnormal uptake of previous avid lesions) or progressive disease (development of new avid lesions). CT response was defined as stable, partial or complete response, or progression defined by Response Evaluation Criteria in Solid Tumours (RECIST 1.1) [25]. Minor response was also used to describe smaller size changes not meeting partial response on RECIST 1.1 (10–30% decrease in maximum diameter of target lesions). Where available, contrast-enhanced CT images were directly compared. Otherwise, non-enhanced CT from PET components of the study were assessed, using scintigraphic uptake as a guide to follow the dominant lesions. Time to next treatment has been included to capture the timing for treatment needed after induction PRRT. For TNT: indications for further treatment (either for uncontrolled symptoms, or disease progression), and treatment modality (such as SSAs dose escalation, further PRRT, everolimus, sunitinib, chemotherapy, external beam radiotherapy, surgery, palliative care) were documented from start of PRRT. Toxicity: all haematological and renal toxicities occurring from the time of PRRT administration were recorded. Toxicity was defined according to the Common Terminology Criteria for Adverse Events version 4.0.
Statistics
The overall survival (OS) and progression free survival (PFS) curves were estimated for the total cohort of patients using the Kaplan-Meier product-limit method measured from start of PRRT to date of death from any cause (or to the date of censoring for patients known to be alive). Progression free survival (PFS) was calculated to tumour progression or death from any cause. Progression was defined by biochemical recurrence and imaging progression on molecular imaging (SSTR+/-FDG) or RECIST 1.1. Patients who received radiosensitising chemotherapy were compared to those who did not receive radiosensitising chemotherapy.
Results
Patient characteristics and treatment parameters
Of the 27 patients treated with PRRT, 19 (70%) patients had ENETs Grade 2 disease, three (11%) had Grade 3, one (4%) had Grade 1, and in four (15%) grading was unavailable. All but one patient had rectal primary (one patient had sigmoid primary). Of 16 patients who had a baseline FDG PET/CT, 63% (11 pts) had FDG-avid disease. Twenty-six patients were treated for disease progression and one patient for uncontrolled symptoms (with abdominal pain, altered bowel habit and per rectal bleeding). Most patients had 177Lu-DOTATATE PRRT, whereas six patients had 90Y-DOTATATE (alone or with combined/sequential 177Lu-DOTATATE cycles). The median cumulative activity of 177Lu-DOTATATE was 30 GBq, median four cycles. Fourteen patients had radiosensitising chemotherapy (5FU or capecitabine). Refer to Table 1 for summary of patient characteristics.
Objective scan response 3 months post PRRT
Ct
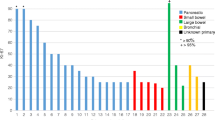
Disease control rate (DCR) was 96%: 70% (19/27) had partial response on RECIST 1.1 and 26% (7 pts) had stable disease, four patients of whom had minor regression on CT (size reduction of 10–30% from baseline); refer to Fig. 1 and Table 2. One patient progressed: this patient had high grade NEN (ENETs G3, Ki 67 of >90%) with an ACTH-secreting tumour with extensive osseous, hepatic and soft tissue metastases, and who had also progressed on prior multiple lines of chemotherapy prior to receiving PRRT. Whilst there was evidence of early molecular imaging response in areas of PRRT targeted disease after two cycles of PRRT, the patient progressed rapidly with spatially discordant FDG-avid disease, requiring further 3rd-line chemotherapy but deceased shortly thereafter due to progression.
57-year-old man, with Grade 2 (Ki67 of 10%) rectal NEN, with liver, pelvic nodal and bone metastases. Following progression on SSA (a, maximum intensity projection MIP images), he received three cycles of 177Lu-DOTA-octreotate. Treatment resulted in SSTR and morphologic partial response 3 months post-PRRT (b). Pre-treatment liver lesions highlighted in solid red arrows (a1), and primary rectal lesion in dotted red arrow (a2). Response of corresponding liver lesions demonstrated on 3 months post-PRRT images in blue arrows (b1), and rectal lesion (b2)
SSTR imaging
All but one had partial SSTR imaging response (Fig. 2, Table 2).
68-year-old woman, previously resected rectal NEN, presented with dominant hepatic liver metastases, Ki67 of 15% (a). PRRT was given due to rapid symptoms and radiological progression. Near complete response on 68Ga-DOTATATE PET/CT shown at 3 months after PRRT completion, red arrow (b). Further response at 9 months (c) and sustained response at 18 months (d) without intervening therapy
Symptom response
At 3 months post-PRRT, 22% (N = 6), reported complete resolution of symptoms (including complete resolution of pain in two patients, regaining weight in two patients, resolution of diarrhea and bloating in one, and disappearance of diarrhea in one patient). Overall 59% (16/27 patients) reported partial improvement of symptoms, mainly with reduction of pain, improvement in weight, prior bowel symptoms including bloating and altered bowel habits, improvement of neurological symptoms from bony disease in two patients and resolution of rectal bleeding in one patient. Two patients reported stable symptoms, and one patient progressed/died. Of note, only three patients of this cohort reported the presence of hormone-secretory symptoms with diarrhea prior to PRRT, but all reported improvement and one had complete symptoms resolution. Refer to Table 2.
Biochemical response 3 months post-PRRT
Baseline CgA results were unavailable for five patients, hence, results of 22 patients were available for review. The majority 59% (13/22) had normal baseline level. Out of the nine patients with baseline elevated CgA, five had significant reduction at 3 months (reduced by 35, 37, 55, 56 and 76%, respectively, from baseline), and four patients had stable results post-PRRT. Refer to Table 2.
Overall and progression free survival and follow-up, TNT
Median follow-up calculated using the reverse censoring method, was 67 months (3–124 months) from start of PRRT. Median overall survival was 81 months (Fig. 3). Ten deaths were observed prior to the close-out date. All patients died from progressive disease. The median progression free survival was 29 months (Fig. 3).
Patients who received radiosensitising chemotherapy (N = 14) were compared to those who did not receive radiosensitising chemotherapy (N = 13). Differences in PFS and OS in the group who received radiosensitising chemotherapy versus those without, were not statistically significant; PFS for radiosensitising chemotherapy group was 32 months vs. 25 months (P value 0.09); OS for radiosensitising chemotherapy 76 months vs. 56 months (P value 0.8).
Of note, one patient had metastatic disease from sigmoid origin; this patient had two cycles of PRRT resulting in complete symptom resolution, partial molecular and RECIST response, with PFS of 15 months and OS of 30 months. During follow-up, 16 patients received further active treatment following completion of induction PRRT. Three patients had further maintenance PRRT, one had elective surgery to primary tumour. Others (12 patients) had further treatment due to disease progression: median time to next treatment for disease progression was 28 months (3–66 months), modalities included further PRRT in five patients, PRRT and capecitabine + temozolomide chemotherapy in one, PRRT and surgery in one patient, increase SSA dosage in one patient, chemotherapy in one, everolimus and TACE in one, and external beam radiotherapy and surgery in two patients.
Toxicity
At 3 months post-PRRT, three patients developed Grade 3 lymphopaenia without clinical significance. No other Grade 3 or 4 haematological toxicities identified. No cases of myelodysplasia or leukaemia were observed during follow-up. Refer to Table 3.
No significant renal toxicities attributable to PRRT were identified. One patient had mild renal dysfunction prior to PRRT which remained stable post-treatment.
Discussion
Although uncommon among the GEP NEN subtypes, the incidence of metastatic rectal NEN is increasing. Patients with metastatic rectal NEN carry a poor prognosis, and robust evidence guiding treatment options of these patients is lacking. Hence, establishing effective and well-tolerated treatments are urgently needed to improve tumour control and patient outcome for such patients.
Given favourable responses and effectiveness of PRRT for patients with SSTR expressing GEP NEN based on large international clinical experiences and more recently, the prospective phase III NETTER-1 trial in patients with midgut NEN [17, 18], we reviewed the efficacy of PRRT in patients with SSTR expressing metastatic disease specifically arising from rectal origin. Whilst there have been small case studies indicating effectiveness of PRRT in such patients [26, 27], to our knowledge, this is the largest series to date assessing the use of targeted radionuclide therapy in patients with rectal NEN. Our results indicate remarkable responses from PRRT in a high proportion of patients despite prior progressive disease. The majority of patients reported partial or complete resolution of symptoms, particularly with reduction of pain, regaining weight and improvement of bowel related symptoms including resolution of rectal bleeding in one patient. Our findings also confirm that most patients with metastatic rectal NEN do not have hormone-secretory symptoms nor measurable CgA biomarker at baseline. All but one patient (96%) had partial response on molecular imaging, and PRRT resulted in a high proportion achieving tumour regression on structural imaging with 70% having a partial RECIST 1.1 response, and an additional 15% having minor tumour shrinkage. This morphological response rate appears vastly superior to limited results of other treatment modalities and suggests a disease with high radiation-sensitivity. The RADIANT-2 trial using everolimus with octreotide showed improved PFS compared to placebo (29.9 months vs. 6.6 months), but no morphological RECIST response was observed in G1/2 colorectal patients on post-hoc analysis [16]. Therefore, PRRT results from this study are very encouraging, particularly in the context that most patients in this cohort have poor prognostic features (70% had Grade 2, and 11% Grade 3 disease) and prior progression.
Importantly, the treatment response from PRRT appears durable, with median progression-free survival of 29 months. Impressively, the median overall survival was 81 months despite the poor prognostic features of this cohort, which compares very favourably to historical data (prognosis of 26 months for metastatic rectal group) [11]. The majority of patients who subsequently progressed were treated with further cycles of PRRT, suggesting that retreatment is feasible and effective as long as SSTR expression is retained at all disease sites (Fig. 4). Survival outcomes for patients who received radiosensitising chemotherapy with PRRT were encouraging, but did not reach statistical significance, the numbers were likely too few for accurate assessment. However, no additional toxicity was apparent with its concomitant use. The use of radiosensitising chemotherapy with PRRT should be formally evaluated and incorporated into future prospective trials for patients with colorectal NEN. PRRT was overall well tolerated, without evidence of significant grade 3/4, long term haematologic or renal toxicity, MDS or leukaemia in this series.
33 yo female, with Grade 3 rectal NEN (Ki67 of 22%), with multifocal osseous and hepatic metastases (a). She was treated with two cycles of 177Lu-DOTA-octreotate PRRT resulting in significant near complete imaging response on 68Ga-DOTATATE PET/CT (b). Restaging 8 months after completion of PRRT showed disease recurrence, predominantly with new sites of osseous metastases and small volume hepatic lesions (c). Given high SSTR expression, one further cycle of 177Lu-DOTA-octreotate was administered, resulting again in significant imaging response indicating radiosensitive disease, and that retreatment is feasible
However, potential limitations of this study are recognised. The number of patients reviewed were relatively small, but nonetheless forms the largest series focusing on patients with unresectable rectal NEN given the rarity of this disease. This is a retrospective review of patients from two international institutions, using similar but not uniform treatment or follow-up protocols. Variability included total administered radiopharmaceutical activity, radiopharmaceutical selection, the use of radiosensitising chemotherapy administered, and the use of unenhanced CT of SPECT or PET for structural evaluation for some patients. This series included one case of metastatic NEN arising from the sigmoid, whilst this did not conform to the rest with rectal origin, this was included given rarity of the entity. The specific outcome of this case was discussed, and the outcome from PRRT also appeared favourable compared to historical data suggesting that this may be a potential treatment option requiring future evaluation in hindgut NEN. Validated quality of life questionnaires were not uniformly used in the two centres, and this important aspect should be incorporated in future prospective studies to allow formal assessment of patient reported outcome measures.
Conclusion
Our results indicate high efficacy and morphologic responses to PRRT in patients with metastatic rectal NEN who had progressed after prior therapies. PRRT was well tolerated with minimal toxicity, and results in very encouraging disease control and overall long survival particularly given the unfavourable historical outcome and poor prognostic features of this cohort. Further prospective PRRT trials are warranted given its potential high efficacy in patients with somatostatin receptor-expressing metastatic rectal NEN.
References
Öberg K, Åkerström G, Rindi G, Jelic S. On behalf of the ESMO Guidelines Working Group; Neuroendocrine gastroenteropancreatic tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010; 21(suppl-5):v223–7. https://doi.org/10.1093/annonc/mdq192.
Lloyd RVOR, Kloppel G, Rosai J, editors. WHO classification of tumours of endocrine organs. 4th ed; 2017.
Fazio N, Milione M. Heterogeneity of grade 3 gastroenteropancreatic neuroendocrine carcinomas: new insights and treatment implications. Cancer Treat Rev. 2016;50:61–7. https://doi.org/10.1016/j.ctrv.2016.08.006.
Perren A, Couvelard A, Scoazec JY, Costa F, Borbath I, Delle Fave G, et al. ENETS consensus guidelines for the standards of care in neuroendocrine tumors: pathology: diagnosis and prognostic stratification. Neuroendocrinology. 2017. https://doi.org/10.1159/000457956.
Leoncini E, Boffetta P, Shafir M, Aleksovska K, Boccia S, Rindi G. Increased incidence trend of low-grade and high-grade neuroendocrine neoplasms. Endocrine. 2017. https://doi.org/10.1007/s12020-017-1273-x.
Lawrence B, Gustafsson BI, Chan A, Svejda B, Kidd M, Modlin IM. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin N Am. 2011;40(1):1–18, vii. https://doi.org/10.1016/j.ecl.2010.12.005.
Niederle MB, Hackl M, Kaserer K, Niederle B. Gastroenteropancreatic neuroendocrine tumours: the current incidence and staging based on the WHO and European neuroendocrine tumour society classification: an analysis based on prospectively collected parameters. Endocr Relat Cancer. 2010;17(4):909–18. https://doi.org/10.1677/ERC-10-0152.
Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3(10):1335–42. https://doi.org/10.1001/jamaoncol.2017.0589.
Ramage JK, De Herder WW, Delle Fave G, Ferolla P, Ferone D, Ito T, et al. ENETS consensus guidelines update for colorectal neuroendocrine neoplasms. Neuroendocrinology. 2016;103(2):139–43. https://doi.org/10.1159/000443166.
Caplin M, Sundin A, Nillson O, Baum RP, Klose KJ, Kelestimur F, et al. ENETS consensus guidelines for the management of patients with digestive neuroendocrine neoplasms: colorectal neuroendocrine neoplasms. Neuroendocrinology. 2012;95(2):88–97. https://doi.org/10.1159/000335594.
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26(18):3063–72. https://doi.org/10.1200/JCO.2007.15.4377.
Weinstock B, Ward SC, Harpaz N, Warner RR, Itzkowitz S, Kim MK. Clinical and prognostic features of rectal neuroendocrine tumors. Neuroendocrinology. 2013;98(3):180–7. https://doi.org/10.1159/000355612.
Pavel M, O’Toole D, Costa F, Capdevila J, Gross D, Kianmanesh R, et al. ENETS consensus guidelines update for the management of distant metastatic disease of intestinal, pancreatic, bronchial neuroendocrine neoplasms (NEN) and NEN of unknown primary site. Neuroendocrinology. 2016;103(2):172–85. https://doi.org/10.1159/000443167.
Caplin ME, Pavel M, Ruszniewski P. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(16):1556–7. https://doi.org/10.1056/NEJMc1409757.
Garcia-Carbonero R, Sorbye H, Baudin E, Raymond E, Wiedenmann B, Niederle B, et al. ENETS consensus guidelines for high-grade gastroenteropancreatic neuroendocrine tumors and neuroendocrine carcinomas. Neuroendocrinology. 2016;103(2):186–94. https://doi.org/10.1159/000443172.
Castellano D, Bajetta E, Panneerselvam A, Saletan S, Kocha W, O’Dorisio T, et al. Everolimus plus octreotide long-acting repeatable in patients with colorectal neuroendocrine tumors: a subgroup analysis of the phase III RADIANT-2 study. Oncologist. 2013;18(1):46–53. https://doi.org/10.1634/theoncologist.2012-0263.
Hicks RJ, Kwekkeboom DJ, Krenning E, Bodei L, Grozinsky-Glasberg S, Arnold R, et al. ENETS consensus guidelines for the standards of care in neuroendocrine neoplasia: peptide receptor radionuclide therapy with radiolabeled somatostatin analogues. Neuroendocrinology. 2017. https://doi.org/10.1159/000475526.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 trial of 177Lu-Dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125–35. https://doi.org/10.1056/NEJMoa1607427.
Kong G, Thompson M, Collins M, Herschtal A, Hofman MS, Johnston V, et al. Assessment of predictors of response and long-term survival of patients with neuroendocrine tumour treated with peptide receptor chemoradionuclide therapy (PRCRT). Eur J Nucl Med Mol Imaging. 2014;41(10):1831–44. https://doi.org/10.1007/s00259-014-2788-5.
Kong G, Callahan J, Hofman MS, Pattison DA, Akhurst T, Michael M, et al. High clinical and morphologic response using (90)Y-DOTA-octreotate sequenced with (177)Lu-DOTA-octreotate induction peptide receptor chemoradionuclide therapy (PRCRT) for bulky neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2017;44(3):476–89. https://doi.org/10.1007/s00259-016-3527-x.
Kong G, Johnston V, Ramdave S, Lau E, Rischin D, Hicks RJ. High-administered activity in-111 octreotide therapy with concomitant radiosensitizing 5FU chemotherapy for treatment of neuroendocrine tumors: preliminary experience. Cancer Biother Radiopharm. 2009;24(5):527–33. https://doi.org/10.1089/cbr.2009.0644.
Hubble D, Kong G, Michael M, Johnson V, Ramdave S, Hicks RJ. 177Lu-octreotate, alone or with radiosensitising chemotherapy, is safe in neuroendocrine tumour patients previously treated with high-activity 111In-octreotide. Eur J Nucl Med Mol Imaging. 2010;37(10):1869–75. https://doi.org/10.1007/s00259-010-1483-4.
Claringbold PG, Brayshaw PA, Price RA, Turner JH. Phase II study of radiopeptide 177Lu-octreotate and capecitabine therapy of progressive disseminated neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2011;38(2):302–11. https://doi.org/10.1007/s00259-010-1631-x.
Krenning EP, Valkema R, Kooij PP, Breeman WA, Bakker WH, deHerder WW, et al. Scintigraphy and radionuclide therapy with [indium-111-labelled-diethyl triamine penta-acetic acid-D-Phe1]-octreotide. Ital J Gastroenterol Hepatol. 1999;31(Suppl 2):S219–23.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Ryan J, Akhurst T, Lynch AC, Michael M, Heriot AG. Neoadjuvant (90) yttrium peptide receptor radionuclide therapy for advanced rectal neuroendocrine tumour: a case report. ANZ J Surg. 2017;87(1–2):92–3. https://doi.org/10.1111/ans.12854.
Abdulrezzak U, Kula M, Tutus A, Buyukkaya F, Karaca H. PET/CT and bremsstrahlung imaging after 90Y DOTANOC therapy for rectal net with liver metastases. Clin Nucl Med. 2015;40(10):799–801. https://doi.org/10.1097/RLU.0000000000000894.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent for treatment was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kong, G., Grozinsky-Glasberg, S., Hofman, M.S. et al. Highly favourable outcomes with peptide receptor radionuclide therapy (PRRT) for metastatic rectal neuroendocrine neoplasia (NEN). Eur J Nucl Med Mol Imaging 46, 718–727 (2019). https://doi.org/10.1007/s00259-018-4196-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4196-8