Abstract
Purpose
Grade 3 NENs are aggressive tumours with poor prognosis. PRRT+/− radiosensitising chemotherapy is a potential treatment for disease with high somatostatin receptor (SSTR) expression without spatially discordant FDG-avid disease. We retrospectively evaluated the efficacy of PRRT in G3 NEN.
Methods
Kaplan–Meier estimation was used to determine progression-free survival (PFS) and overall survival (OS) defined from start of PRRT. Subgroup analysis was performed for patients with Ki-67 ≤ 55% and >55%. Anatomical response (RECIST 1.1) and toxicity 3 months after PRRT was determined. Disease control rate (DCR) was defined as complete response (CR), partial response (PR) and stable disease (SD) of those with prior progression.
Results
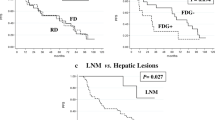
28 patients (M = 17; age 16–78 years; Ki-67 ≤ 55% = 22) were reviewed. 17 patients had pancreatic, 5 small bowel, 3 large bowel, 2 bronchial and 1 unknown primary disease. 25/28 had significant FDG-avid disease prior to treatment. Most had 177Lu-DOTA-octreotate (median cumulative activity 24.4 GBq, median 4 cycles). Twenty patients had radiosensitising chemotherapy. 89% were treated for disease progression; 79% after prior chemotherapy. Median follow-up was 29 months. The median PFS was 9 months for all patients. 16 patients died (Ki-67 ≤ 55% = 11; Ki-67 > 55% = 5) with median OS of 19 months. For Ki-67 ≤ 55% (N = 22), the median PFS was 12 months and median OS 46 months. For Ki-67 > 55% (N = 6), the median PFS was 4 months and median OS 7 months. On CT imaging, DCR at 3 months post-PRRT was 74%, 35% (8/23) PR and 39% (9/23) SD. Eleven patients received further PRRT due to recrudescent disease after response. Five patients developed progression of discordant FDG-avid disease and were referred for targeted therapy/chemotherapy. Grade 3 and 4 lymphopenia and thrombocytopenia occurred in five and five patients, respectively. No renal or liver toxicity related to treatment was seen.
Conclusions
PRRT achieves clinically relevant disease control with acceptable toxicity in G3 NENs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine neoplasia (NEN) is a diverse group of tumours arising from neuroendocrine cells, most commonly in the gastro-intestinal tract and respiratory system. In 2010, the World Health Organisation (WHO) and European Neuroendocrine Tumour Society (ENETS) classified these tumours into three subgroups (grade 1, 2 and 3) [1, 2]. Grade 1 and 2 (Ki-67 proliferation index of ≤2% and 3–20%, respectively) are classified as neuroendocrine tumours (NETs), whereas grade 3 (Ki-67 index of >20%) has been classified as neuroendocrine carcinoma (NEC). Grade 3 NEC is an aggressive subset with a median overall survival (OS) of 4–6 months [3] and has mainly been treated with chemotherapy regimens used for small cell lung cancer. This typically involves cisplatinum/etoposide (C/E) [4].
Over the last few years, several reports have suggested that the grade 3 (G3) NENs are more heterogeneous than previously thought [3, 5,6,7,8]. The NORDIC group proposed an intermediate category of NEC with Ki-67 of ≤55% based on a lower response to C/E but longer OS than those with Ki-67 > 55% [3]. Others have suggested an alternative classification based on morphological differentiation features on pathologic examination, independent of Ki-67 [5, 9]. Although not specifically mentioned, somatostatin receptor (SSTR) expression is a feature of neuroendocrine differentiation and, if retained, may enable peptide receptor radionuclide therapy (PRRT).
68Ga-DOTATATE PET/CT is used to determine tumour SSTR expression in order to select patients for PRRT [10]. In general, the likelihood of SSTR expression on neuroendocrine cells decreases with increasing grade of tumour, whereas the opposite applies for FDG uptake [11, 12]. However, there is significant overlap in the intermediate grade (grade 2) tumours in which both scans can be positive. This overlapping group of intermediate grade tumours may represent a ‘sweet spot’ for PRRT since these patients have simultaneously a greater likelihood of progression and death than the low-grade tumours but at the same time are likely to be more radio- and chemosensitive by virtue of having a higher proliferative fraction. PRRT has been shown to be effective and well tolerated for patients with SSTR expressing well-differentiated gastroenteropancreatic NENs [13]. However, PRRT can also be effective in patients with more aggressive intermediate grade NEN with an FDG-avid and concordant SSTR-expressing phenotype [14].
However, data on PRRT effectiveness in SSTR-expressing G3 NECs is very limited. A previous single-centre retrospective study (abstract form only) by Armagany et al. reported the use of PRRT in high-grade NEN for 17 cases [15]. Two out of six patients (33%) who received 177lutetium octreotate therapy (LuTate) and three out of six (50%) who received 111In octreotide therapy (In-Tate) had stable disease or partial response at 12 months. The median PFS was 9.3 months for LuTate and 10.2 months for In-Tate, and was 12 months when both LuTate and In-Tate were considered. Another study by Ezziddin et al. involving seven patients with G3 NEN examined the impact of Ki-67 index on response to PRRT [16]. The treatment response was, however, less favourable with 71% of the patients with Ki-67 > 20% progressing following therapy.
The Peter MacCallum Cancer Centre (PMCC) commenced using PRRT in 1996 for treatment of patients with unresectable, SSTR-positive, symptomatic or progressive NET, not controlled with conventional therapy. In 1999, our protocol was adapted to include concomitant use of radiosensitising chemotherapy. It has long been dogma that chemotherapy should be used for high-grade tumours and that PRRT should be reserved for slowly proliferating tumours that are resistant to chemotherapy [13, 17]. However, the compassionate use protocol employed at PMCC has not precluded treatment of G3 NEC. Accordingly, a number of patients with G3 NEN have been treated either after failure of conventional therapies or because patients were deemed unsuitable for other treatment. All patients were discussed in our weekly NEN multidisciplinary team meeting prior to therapy.
The aim of this retrospective analysis was to assess outcomes following PRRT in patients with high-grade NEN as defined by Ki-67 > 20%. Primary end-points were OS, PFS and time to next treatment (TNT) modality. We also assessed molecular imaging and anatomical response, and toxicity.
Materials and methods
All patients with G3 NEN (Ki-67 > 20% on immunohistochemistry) and who had completed at least one cycle of PRRT between January 2005 and January 2017 were retrospectively reviewed.
Our eligibility criteria for PRRT included patients with high SSTR expression in all lesions, with the majority of lesions having higher uptake than background liver activity on Ga-68 DOTA-octreotate (GaTate) PET/CT. Patients were to have objective evidence of disease progression on anatomical or functional imaging over a period of <12 months, or uncontrolled symptoms despite conventional therapy. Patients with concordant highly FDG-avid disease even without prior progression were eligible given FDG avidity is a poor prognostic factor, particularly if this persisted following chemotherapy.
Exclusion criteria for PRRT included spatially discordant FDG-avid disease showing low or absent SSTR expression, glomerular filtration rate (GFR) <30 ml/min, hypoalbuminaemia (<25 g/L), platelet count <50,000/L or pancytopenia, ECOG performance score of 4, expected survival <3 month and pregnancy.
Our indication for treatment was largely based on data presented by Kwekkeboom et al. [18] but has evolved over time based on our clinical experience [19].
This retrospective study had been approved by the local ethics committee (project number: 17/07R). All patients provided written, informed consent for treatment.
Treatment regimen
PRRT was performed on an outpatient day-case basis unless the patient’s medical co-morbidities required inpatient observation or there was deemed to be a significant potential risk of disease flare following treatment.
177Lutetium (177Lu) was produced and transported to our institution from Europe (IDB Holland) and radiolabelled to the peptide octreotate (Erasmus Medical Centre, Rotterdam, Holland) with DOTA as the chelating agent, forming 177lutetium-DOTA-octreotate (177Lu-DOTATATE or LuTate). Some patients with bulky disease (>4 cm) were also treated with 90Yttrium (Perkin Elmer, Waltham, MA, USA), which was labelled onto DOTA-octreotate to form 90Y-DOTATATE (or Y-Tate) as previously reported [20].
Each cycle of treatment was administered intravenously with premedications including 2 mg of granisetron and 8 mg of dexamethasone [21], to reduce potential adverse effects of nausea related to amino acid infusion and post-treatment disease flare. The patients were provided with two additional days of 2 mg of granisetron and 4 mg of dexamethasone following treatment. Renoprotective amino acid infusion (25 g of lysine and 25 g of arginine in 1 L of normal saline) as previously proposed by others [18, 22] was commenced 30 min prior to treatment and continued for 4 h after Y-Tate and 3 h after LuTate therapy, except in patients with impaired renal function (GFR 60 ml/min) in whom infusion was also extended to 4 h based on our previous evaluation of blood clearance kinetics of LuTate [23].
The initial treatment regimen is typically planned for four cycles of PRRT at intervals of 6–10 weeks. The second to fourth cycles were usually given with radiosensitising chemotherapy using infusional 5-FU or oral capecitabine [24,25,26,27], or concomitant capecitabine and temozolomide (CAPTEM) [28,29,30] for pancreatic NEN, unless contraindicated. Infusional 5-FU chemotherapy (200 mg/m2/24 h) was given through a peripherally inserted central catheter (PICC) line, commencing 4 days prior to day of PRRT administration, and continued for 3 weeks in total. Capecitabine was given in 825 mg/m2 (bd), 2 days prior to PRRT administration and continued for 2 weeks. For the CAPTEM regimen, capecitabine was given as 750 mg/m2 oral bd (max 2500 mg/day) on days 1–14 commencing 9 days prior to PRRT, and temozolomide 100 mg/m2 bd (75 mg/m2 if extensive prior chemotherapy) on days 10–14, i.e. commencing on the day of PRRT for 5 days.
The number of cycles of PRRT was increased in patients with persistent large disease burden following completion of initial four cycles, whilst treatment cycles were abbreviated in patients with a marked early PRRT response leaving only a small volume of disease based on post-treatment scanning, or if there were complications from therapy. The administered activity for each cycle was empirically adjusted, based on individual disease burden, body habitus and renal function [19].
If there was a suspicion of tumour progression during the initial course of PRRT based on clinical, biochemical or imaging findings, FDG PET/CT was performed. Those who were confirmed to have progression of discordant FDG-avid disease were considered for alternative treatment modalities such as chemotherapy or molecular targeted therapy.
Follow-up
Blood tests including full blood count, and renal and liver function biochemistries were performed at 2 and 4 weeks following completion of each treatment cycle. Following the completion of the initial course of PRRT, patients were also routinely reviewed at 3 months by imaging and blood tests. On some occasions, especially those with a proliferation rate at the upper end of the G3 category or who had shown rapid disease progression prior to treatment, we elected to review them earlier for response assessment. Following the initial assessment, these patients were further followed up at 3 to 12-month intervals at our institution. Patients who had demonstrated symptomatic or objective response to initial PRRT treatment but had persisting or recrudescent SSTR-expressing disease were considered for further maintenance PRRT treatments. However, patients who progressed through or after PRRT with discordant FDG-avid but low/non-SSTR-expressing disease would be referred for consideration of other treatment modalities.
Response assessment
Molecular imaging response
Qualitative response on SSTR imaging was classified as complete response (total disappearance of abnormal uptake by previous avid lesions), partial response (reduction in intensity or extent of previous abnormal uptake), stable (no change in intensity or extent of disease) or progressive disease (increase in intensity or extent of previous abnormal uptake, or development of new avid lesions). Metabolic responses were assessed on the FDG PET images according to the “Hicks criteria” [31, 32]. A mixed response category was also allocated to patients with response at prior sites of targeted disease and progression of disease at previously lower avidity sites. Quantitative assessment was also performed for both Ga-68 octreotate and FDG PET/CT scans to compare pre-treatment to 3-month post-treatment scans using MIM (MIM 6.6.1, MIM Software Inc. Cleveland, OH, USA). The whole-body disease burden was contoured by adapting the PERCIST recommendation using a threshold that equalled 1.5 × mean liver SUV + 2SD [31]. This threshold was lowered in two patients to allow quantification of disease with lower intensities that would have been excluded by the PERCIST threshold. Any normal physiologic uptake was manually excluded. The change in whole-body disease in volume (ml) was measured.
CT response is categorised as stable, partial or complete response, or progression, defined by Response Evaluation Criteria in Solid Tumours (RECIST 1.1) [33]. Where available, contrast-enhanced CT images were directly compared. Otherwise, non-enhanced CT images from the SPECT or PET components of the study were assessed, using metabolic uptake as a guide to follow the dominant lesions.
Molecular imaging and CT responses were assessed at 3 months after the last cycle of induction PRRT. Best treatment response (and timing of best treatment response) by molecular or anatomical imaging were further identified from the start of treatment and prior to any commencement of maintenance PRRT or other treatment modalities, or death.
Toxicity profile including haematological, renal and liver function following induction cycles of PRRT by the Common Terminology Criteria for Adverse Events (CTCAE v4.0) based on serial blood tests and the physician’s report.
Statistics
Kaplan–Meier statistics were used to characterise OS, PFS and TNT, by assessing the length of time between date of commencement of PRRT to date of death from any cause (or to the date of censoring for patients known to be alive), disease progression biochemically or on imaging, and commencement of the next treatment modality (GraphPad Prism 7). Next treatment modality is defined as any other oncologic therapy other than PRRT.
Results
Patient characteristics
Twenty-eight patients (17 men, 11 women; median age at first treatment 62.5 years, range 16–78 years) met the eligibility criteria to be included in our study. The baseline characteristics and treatment parameters are summarised in Table 1. Of the 28 patients, 22 (79%) had Ki-67 ≤ 55%, 61% had a pancreatic primary disease and 64% had the dominant site of metastatic disease being the liver. Figure 1 shows Ki-67 values for all patients according to the primary site of disease. Approximately one third had functional secretory symptoms or raised hormone levels.
The majority (89%) were treated for disease progression (79% had prior chemotherapy). PRRT was the second-line systemic treatment for 45% and third-line for 29% of patients. Two out of 28 were treated for residual SSTR-expressing disease following chemotherapy to consolidate a partial treatment response, and one was treated with first-line treatment. Two patients had only one cycle of treatment, and both died from early disease progression.
Eight (29%) of the patients had significant FDG-avid disease (i.e. with intensity above liver parenchyma) prior to treatment. In retrospect, two patients who were treated had sites of FDG-avid disease without uptake on SSTR-imaging at baseline that we define as “discordant FDG-avid disease” and represent an exclusion criteria for PRRT.
Twenty patients were treated with concomitant radiosensitising chemotherapy. Of the eight patients not given chemotherapy, one had anaemia requiring transfusion before PRRT, two had received extensive prior chemotherapy, one had only a small volume of disease, one had pelvic collection suspected of infection post-surgery and one patient chose not to be treated with chemotherapy. The remaining two had only one cycle of PRRT (chemotherapy usually given from the second cycle onwards).
Objective response at 3 months (Table 2)
Molecular imaging response at 3 months post-PRRT
SSTR imaging
Five of the 28 patients had no SSTR imaging at 3 months post-PRRT (three died and two progressed during induction). The disease control rate of the remaining 23 patients was 61% (57% with partial response and 4% with stable disease).
The percentage change in tumour volume of SSTR-expressing disease is shown in Fig. 2 (N = 20). Quantitative assessment was not possible in three patients due to the following reasons: one patient had follow-up 111In-DOTATATE SPECT/CT, which had been used for serial evaluation of this patient prior to PRRT, precluding accurate quantitative assessments, two patients had scanning performed in other hospitals with incomplete imaging data to perform quantitative assessment.
FDG imaging
Ten of the 28 patients had no comparable FDG imaging at 3 months post-PRRT (three died and two progressed during induction, two had no FDG scan at baseline, and three had no follow-up FDG scans performed at 3 months). Of the remaining 18 patients, one (6%) had complete metabolic response and seven (39%) had partial metabolic response at 3 months post-PRRT. Three of the nine patients who progressed had progression of new discordant FDG-avid lesions, with partial response seen in the targeted SSTR-expressing sites. All three were deemed unsuitable for further PRRT and were further treated with targeted therapy or systemic chemotherapy.
One patient with small bowel NET (Ki-67 35%) had mixed findings with partial response seen in some of the previously targeted SSTR-expressing sites of liver disease but progression of other sites of concordant FDG-avid liver and bony metastases at 3 months post-PRRT.
CT response at 3 months post-PRRT
Twenty-three of the 28 patients had evaluable CT scans available for comparison at 3 months post-PRRT. The disease control rate was 74%. Eight (35%) had partial RECIST 1.1 response and nine (39%) had stable disease. Figure 3 shows a reduction in targeted lesions up to 86% at 3 months post-PRRT.
Morphologic response by RECIST 1.1 criteria, 3 months post-PRRT (N = 23). Eight patients had a partial response (dark blue), nine patients with previously progressive disease had stabilisation of disease (light blue) and six patients had progressive disease (red). Of note, four of the six patients with progressive disease had partial response in previously targeted disease but developed new sites of disease on follow-up scans. Patient 22 also had new metastatic disease on follow-up
Best response
Response better than at 3 months post-treatment was identified in several patients. Five patients (all with Ki-67 ≤ 55%) showed further imaging response up to 15 months post-induction cycles of PRRT (Table 3). Two of the five patients only had two cycles of induction PRRT due to marked response during treatment. On the other hand, seven patients (Ki-67 ≤ 55%, 3 patients; Ki-67 > 55%, 4 patients) also had early partial response during induction PRRT. However, all eventually progressed and/or died at (or before) 3 months post-PRRT. Two developed discordant FDG-avid disease (Ki-67 ≤ 55%, 1 patient; Ki-67 > 55%, 1 patient) and 5 had progressive concordant disease.
Symptoms
Three patients with hormone-related symptoms were noted. Two of the three patients had improvement (flushing and diarrhoea) at 3 months post-PRRT. One of the patients continued to have exertional breathlessness and peripheral oedema as the dominant symptoms at 3 months follow-up and these were related to carcinoid heart disease. Tricuspid valve replacement was attempted but the patient had a flare response during pre-operative preparation with somatostatin injections. The patient remains on frusemide with regular cardiology review. Symptomatic benefit was not assessable in one patient who died after one cycle of PRRT.
Toxicity
In the 28 patients, grade 3 and 4 lymphopenia occurred in 5 patients without clinical consequences. Grade 3 thrombocytopenia occurred in three patients up to 3 months following completion of induction cycles of PRRT (Table 4). On subsequent follow-up, two new cases of persistent grade 3 and 4 thrombocytopenia (which were not seen up to 3 months follow-up) were further noted. Both had further cycles of PRRT due to recrudescence disease. Three of the five patients had concomitant CAPTEM chemotherapy and two patients had extensive skeletal metastases. Of note, nine other patients in our study received CAPTEM or temozolamide during their PRRT (five during induction, four during retreatment) and have had no issues with myelotoxicity. No myelodysplasia or leukaemia was recorded until death or study cut-off date in this cohort.
No grade 3 or 4 renal impairment was seen. Mild to moderate deterioration of GFR is seen in four patients (grade 1 in one patient; grade 2 in three patients). With regards to liver function, four patients had grade 3 dysfunction in one or more of the components of liver function test over baseline up to 3 months following completion of induction PRRT. Three had disease progression in the liver and one patient’s liver function test subsequently improved (up to a year) with scan findings showing good response to treatment in the liver metastases. After 3 months of follow-up, three additional patients (who had normal liver function up to 3 months following induction PRRT) had grade 3 dysfunction in their liver function tests. All three had extensive and progressive liver metastases and eventually died. None of the liver function dysfunction was directly related to PRRT.
Overall survival, time to progression, time to next treatment (TNT) modality and maintenance PRRT
Median follow-up was 29 months (range 4–85). The median PFS was 9 months (for Ki-67 ≤ 55%, 12 months; and Ki-67 > 55%, 4 months; Fig. 4). Sixteen patients died during the period of the study (11 patients with Ki-67 ≤ 55%, 5 patients with Ki-67 > 55%). Median OS was 19 months (for Ki-67 ≤ 55%, 46 months; and Ki-67 > 55%, 7 months; Fig. 5).
Five of the 6 patients with Ki-67 > 55% had early favourable response during PRRT of the sites of targeted disease. However, four patients subsequently progressed and/or died at 3 months of follow-up. One patient is alive with ongoing good response at 7 months of follow-up post-induction PRRT (Fig. 6).
Top row (a1–a3): Serial 68Ga-DOTATATE PET/CT maximum intensity projection (MIP) images. Bottom row (b1–b3): Serial FDG PET/CT MIP images. 34-year-old man with metastatic pancreatic neuroendocrine tumour, Ki-67 of 80%, with multifocal bilobar hepatic metastases. He progressed despite eight cycles of carboplatin and etoposide within a 6-month period and was treated with five cycles of induction PRRT, three with concomitant radiosensitising chemotherapy (CAPTEM). Imaging at 3 months showed marked partial response with reduction of liver span on 68Ga-DOTATATE PET/CT (a2) and FDG PET/CT (b2). In view of high Ki67 and residual FDG-avid disease, he was further treated with one consolidation cycle of PRRT at 4 months of follow-up with ongoing response seen at 7 months post-induction PRRT (a3, b3)
Median time to next treatment modality or death for all patients was 17 months (for Ki-67 ≤ 55%, 19 months; and Ki-67 > 55%, 4 months).
Eleven patients received subsequent maintenance cycles of PRRT due to recrudescent disease after response (Fig. 7). Median time to maintenance PRRT from first cycle induction was 12 months (range 8–29 months). In the 2 patients with Ki-67 > 55%, the time to maintenance PRRT was 8 and 9 months respectively. The remaining 9 patients with Ki-67 ≤ 55% had median time to maintenance PRRT of 16 months (range 9–29 months). Within these 11 patients, a median PFS of 12 months and median OS of 46 months were found on further analysis.
a1, a3–a8: Serial 68Ga-DOTATATE PET/CT maximum intensity projection (MIP) images. a2: 111In-octreotate SPECT/CT maximum intensity projection (MIP) image. 53-year-old man with a metastatic rectal neuroendocrine tumour, Ki-67 of 40%, with persisting extensive liver disease despite 6 cycles of carboplatin-etoposide chemotherapy (a1). He was subsequently treated with four induction cycles of 177Lu-DOTATATE with concomitant radiosensitising chemotherapy (5-FU). A restaging scan at 3 months showed marked partial response in the liver disease and stable findings in the presacral/peri-rectal disease (a2). Remarkably, resolution of SSTR-expressing liver metastases was noted at 9 months post-PRRT (a3). On further follow-up, he had recrudescence of disease (predominantly liver with small volume nodal and bony metastases; a4, a6) and received more PRRT throughout the years with favourable symptomatic and imaging response (a5, a7, a8). Overall, he benefited from 15 cycles of PRRT (total 114 GBq of 177Lu-DOTATATE and 3.1 GBq of 90Y–DOTATATE) before he eventually died of disease progression refractory of treatment 6 years and 5 months from first cycle of PRRT
Discussion
Current international guidelines support use of PRRT in patients with unresectable grade 1 or 2 NET [13, 22, 34]. Our centre, with 20 years of experience with PRRT, has seen favourable treatment response with this therapeutic modality in patients with NETs. Our reported outcomes, including those with bulky tumours as well as FDG-avid tumours, have seen a median PFS of 33 to 48 months following PRRT [14, 20], with median OS not reached up to a median follow-up of 60 months in another larger cohort of patients [24]. Most studies reported in the literature have been limited to well-differentiated, G1–2 disease (i.e. Ki-67 ≤ 20%) and only a small proportion have included G3 tumours [13]. Recently, the only randomised phase 3 trial reported to date, showed that 177Lu-DOTATATE was superior to somatostatin analogues for midgut NETs but also focused on well-differentiated disease [35].
Our study, to the best of our knowledge, is the first to evaluate the use of PRRT with concomitant radiosensitising chemotherapy in G3 NEN. As expected, the median PFS and OS were shorter when compared to the well-differentiated cohort. However, these results are encouraging given the multiple adverse prognostic factors, including failure of prior chemotherapy in a majority of the patients, FDG avidity of the tumours as well as high proliferation rate. Other centres [15, 16] have evaluated the use of PRRT in G3 NEN or impact of Ki-67 on response to PRRT. Our median PFS is comparable to that reported by Armagany et al. and contrary to that published by Ezziddin et al., in that our disease control rate was much higher.
The current recommendation for first-line treatment for non-resectable G3 NEN is platinum-based chemotherapy in combination with etoposide [17, 36]. The NORDIC study reported a median PFS of 4 months and a median OS of 11 months for patients who received first-line chemotherapy [3]. Our results have shown longer survival data with PRRT when compared to the NORDIC group, with overall median PFS of 9 months and median OS of 19 months. This result is promising, given that 79% of our patients had already received at least one line of chemotherapy (68% receiving platinum-based) prior to commencing PRRT. The median OS for those with Ki-67 ≤ 55% is markedly longer than the NORDIC group (46 months versus 14 months), but shorter in the Ki-67 > 55% arm (7 months for PRRT versus 10 months for chemotherapy). PRRT is potentially a superior first-line therapeutic option for patients with Ki-67 ≤ 55% as compared to platinum-based chemotherapy, provided the disease expresses high SSTR receptors with no discordant FDG-avid disease. Platinum-based chemotherapy may be better reserved as first-line therapy for patients with Ki-67 > 55%, in which a higher response rate to chemotherapy was observed in this group by the NORDIC study.
Another study using temozolomide-based chemotherapy in G3 NEN patients following progression with at least one prior chemotherapy regimen has found that patients with Ki-67 < 60% had a better response, further reinforcing the heterogeneity of G3 NEN [37]. A majority of the patients (96%) received cisplatin/etoposide prior to temozolomide-based chemotherapy. The median PFS in all patients was shorter than our cohort (6 months vs. 9 months) but the median OS was longer (22 months vs. 19 months). Their reported response rate is lower (29% had partial response and 38% had stable disease), although it was not directly comparable to our study due to the difference in timing of follow-up (median time of duration of follow-up 18–19 months). A different group further focused their attention on evaluating the role of everolimus in G3 (pancreatic) NEN with Ki-67 ≤ 55% [38]. Four of the 15 patients received everolimus as first-line treatment and 11 had been pretreated with chemotherapy or PRRT. The median PFS and OS after everolimus initiation was significantly shorter compared to our patients (PFS: 6 months vs. 12 months; OS: 28 months vs. 46 months). The favourable survival data suggests that PRRT is also likely to be more effective than current second-line chemotherapy or targeted therapy, especially within the lower Ki-67 subgroup.
Three patterns of responses were seen in our cohort of patients: early and sustained response, early but unsustained response and delayed response following induction PRRT. Five patients had ongoing disease regression up to 15 months post-induction PRRT. Remarkably, two of these patients had only two cycles of PRRT. It was postulated that PRRT may have eradicated the poorly differentiated disease with remaining disease being of a more well-differentiated form and behaving like the more indolent G1/2 NET. On the contrary, seven other patients who had marked treatment response before their 3-month restaging scans eventually progressed or died at 3 months follow-up. This reflects significant heterogeneity in G3 NENs. The small study cohort, however, precludes the ability to identify predictors of response. Close monitoring is recommended for those with early marked response due to the potential of early disease relapse. Future studies incorporating pathology morphologic differentiation classification will be worthwhile. Of note, tumours that are discordant on FDG PET scans will not be targeted adequately by PRRT and will hence progress. All five of our patients with progressive discordant FDG-avid disease were referred for other treatment options. Discordant FDG-avid lesions, if confined to a certain organ, can be targeted by organ-directed therapy such as surgery, radiofrequency ablation, whilst more widespread discordant disease will require systemic therapy such as targeted therapy or chemotherapy.
Eleven of the 28 patients who initially responded to induction PRRT subsequently had recrudescence of disease and were treated with further cycles of PRRT. An encouraging median PFS of 12 months and median OS of 46 months in this particular group signify that retreatment is an option. A small percentage of patients with hormone-related symptoms prior to treatment also had symptom resolution or improvement following induction PRRT, indicating potential use for symptom control in G3 NEN.
In this population, it is difficult to ascertain how much of the toxicity relates to prior treatment, the burden of disease in marrow and liver and the effects of PRRT. Pre-existing impairment of bone marrow function from prior C/E and the potential for nephrotoxicity from cisplatin may predispose such patients to treatment-related toxicity. Nevertheless, treatment with PRRT was well tolerated in the majority of patients. Grade 3 or 4 thrombocytopenia was the predominant haematologic toxicity occurring in five patients, all previously treated with chemotherapy prior to PRRT. Three of these patients had PRRT combined with CAPTEM, with the alkylating agent temozolamide possibly contributing to toxicity. However, nine other patients in our study received CAPTEM or temozolamide during PRRT and have had no issues with myelotoxicity. A separate study that evaluated potential toxicity of concomitant radiosensitising chemotherapy in well-differentiated progressive metastatic gastroenteropancreatic NETs which were monitored over a 5-year period found that haematological toxicity is not significantly increased by the addition of CAPTEM in combination with PRRT [39]. Extensive skeletal disease was also noted in the two remaining patients who did not receive CAPTEM, and one had mild derangement of full blood count prior to commencement of treatment. Therefore, reduction in administered dose may be considered in such cases. Two of the five patients had widespread liver disease, with reduction in thrombopoietin production in the liver due to radiation effect post-treatment potentially being another cause of thrombocytopenia. Liver function derangement over the course of therapy in our study appeared to be disease- rather than treatment-related. No significant renal toxicity was observed, comparable to our prior reported results ( [23]).
There are some limitations in our study related primarily to eligibility for PRRT being determined on compassionate grounds rather than by strict criteria. The study is retrospective in nature, in a single-institution setting and derived from a small number of patients, especially in the Ki-67 > 55% group, because many such patients either lack SSTR expression at all disease sites or have too poor performance status after failing chemotherapy to be considered for PRRT. There is also some heterogeneity in our cohort, we had two bronchial NENs and one patient of unknown primary, although the majority had GEP NEN. There was some variation in the administered activity and number of cycles, though this reflects our individualised approach rather than a fixed regimen for all patients. Further, the additional value of concomitant radiosensitising chemotherapy is difficult to quantify in this setting as, although radiosensitising chemotherapy was used in the majority of patients, it was limited only to the PRRT treatment cycles and most patients had already failed at least one line of prior chemotherapy. A repeat biopsy was not performed in our patients prior to PRRT. However, a majority of these patients had disease progression on chemotherapy with significant FDG-avid disease prior to PRRT which suggests a high-grade phenotype.
Conclusion
This preliminary study has shown that PRRT, combined with radiosensitising chemotherapy or without, results in promising clinical outcome with acceptable toxicity profiles in G3 NEN, even in patients who had failed chemotherapy, especially for those with Ki-67 ≤ 55%, where first-line platinum-based chemotherapy has shown a lower rate of response. Since a number of patients failed PRRT with primarily FDG-avid disease lacking SSTR expression, it may be preferable and less toxic to treat suitable patients with PRRT as a first-line therapy and reserve chemotherapy for cases where this eventuates. The relatively poor outcome of patients with a Ki-67 > 55% suggests more effective combination therapies are particularly needed for this group.
Our data from this cohort support the need for larger prospective, randomised, controlled studies comparing the various therapeutic options in future.
Change history
20 November 2017
On page 4 of the original version of this article, the text “Eight (29%) of the patients had significant FDG-avid disease (i.e. with intensity above liver parenchyma) prior to treatment” needs to be corrected.
References
Rindi G, Arnold R, Bosman FT, Bosman T, Carneiro F, Hruban R, et al. Nomenclature and classification of neuroendocrine neoplasms of the digestive system. WHO Classification of Tumours of the Digestive System 4th edn. Lyon: International Agency for Research on Cancer (IARC); 2010. 13–4.
Öberg K, Knigge U, Kwekkeboom D, Perren A, ESMO Guidelines Working Group. Neuroendocrine gastro-entero-pancreatic tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23:vii124–30.
Sorbye H, Welin S, Langer SW, Vestermark LW, Holt N, Osterlund P, et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol. 2013;24:152–60. https://doi.org/10.1093/annonc/mds276.
Fazio N, Spada F, Giovannini M. Chemotherapy in gastroenteropancreatic (GEP) neuroendocrine carcinomas (NEC): a critical view. Cancer Treat Rev. 2013;39:270–4. https://doi.org/10.1016/j.ctrv.2012.06.009.
Velayoudom-Cephise FL, Duvillard P, Foucan L, Hadoux J, Chougnet CN, Leboulleux S, et al. Are G3 ENETS neuroendocrine neoplasms heterogeneous? Endocr Relat Cancer. 2013;20:649–57. https://doi.org/10.1530/ERC-13-0027.
Heetfeld M, Chougnet CN, Olsen IH, Rinke A, Borbath I, Crespo G, et al. Characteristics and treatment of patients with G3 gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer. 2015;22:657–64.
Milione M, Maisonneuve P, Spada F, Pellegrinelli A, Spaggiari P, Albarello L, et al. The clinicopathologic heterogeneity of grade 3 gastroenteropancreatic neuroendocrine neoplasms: morphological differentiation and proliferation identify different prognostic categories. Neuroendocrinology. 2017;104(1):85–93.
Tang LH, Basturk O, Sue JJ, Klimstra DS. A practical approach to the classification of WHO grade 3 (G3) well-differentiated Neuroendocrine tumor (WD-NET) and poorly differentiated Neuroendocrine carcinoma (PD-NEC) of the pancreas. Am J Surg Pathol. 2016;40(9):1192–202. https://doi.org/10.1097/PAS.0000000000000662.
Tang LH, Untch BR, Reidy DL, O'Reilly E, Dhall D, Jih L, et al. Well-differentiated Neuroendocrine tumors with a morphologically apparent high-grade component: a pathway distinct from poorly differentiated Neuroendocrine carcinomas. Clin Cancer Res. 2016;22(4):1011–7. https://doi.org/10.1158/1078-0432.CCR-15-0548.
Hofman MS, Hicks RJ. Changing paradigms with molecular imaging of neuroendocrine tumors. Discov Med. 2012;14(74):71–81.
Binderup T, Knigge U, Loft A, Federspiel B, Kjaer A. 18F-Fluorodeoxyglucose positron emission tomography predicts survival of patients with neuroendocrine tumors. Clin Cancer Res. 2010;16(3):978–85. https://doi.org/10.1158/1078-0432.CCR-09-1759.
Garin E, Le Jeune F, Devillers A, Cuggia M, de Lajarte-Thirouard AS, Bouriel C, et al. Predictive value of 18F-FDG PET and somatostatin receptor scintigraphy in patients with metastatic endocrine tumors. J Nucl Med. 2009;50(6):858–64. https://doi.org/10.2967/jnumed.108.057505.
Hicks RJ, Kwekkeboom DJ, Krenning E, Bodei L, Grozinsky-Glasberg S, Arnold R, et al. ENETS consensus guidelines for the standards of Care in Neuroendocrine Neoplasia: peptide receptor radionuclide therapy with Radiolabeled Somatostatin analogues. Neuroendocrinology. 2017; https://doi.org/10.1159/000475526.
Kashyap R, Hofman MS, Michael M, Kong G, Akhurst T, Eu P, et al. Favourable outcomes of (177)Lu-octreotate peptide receptor chemoradionuclide therapy in patients with FDG-avid neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2015;42(2):176–85. https://doi.org/10.1007/s00259-014-2906-4.
Armaghany T, Vahdati G, Thamake S, Hamidi M, Amerinia R, Delpassand E. Treatment of high grade metastatic neuroendocrine tumor (mNET) with peptide receptor radionuclide therapy (PRRT): Retrospective analysis in a single referral center. J Clin Oncol 33, 2015 (suppl; abstr e15175).
Ezziddin S, Opitz M, Attassi M, Biermann K, Sabet A, Guhlke S, et al. Impact of the Ki-67 proliferation index on response to peptide receptor radionuclide therapy. Eur J Nucl Med Mol Imaging. 2011;38(3):459–66. https://doi.org/10.1007/s00259-010-1610-2.
Garcia-Carbonero R, Sorbye H, Baudin E, Raymond E, Wiedenmann B, Niederle B, et al. ENETS consensus guidelines for high-grade gastroenteropancreatic neuroendocrine tumors and neuroendocrine carcinomas. Neuroendocrinology. 2016;103:186–94. https://doi.org/10.1159/000443172.
Kwekkeboom DJ, de Herder WW, Kam BL, van Eijck CH, van Essen M, Kooij PP, et al. Treatment with the radiolabeled somatostatin analog [177Lu-DOTA0,Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol. 2008;26:2124–30.
Hofman MS, Hicks RJ. Peptide receptor radionuclide therapy for neuroendocrine tumours: standardized and randomized, or personalized? Eur J Nucl Med Mol Imaging. 2014;41(2):211–3. https://doi.org/10.1007/s00259-013-2621-6.
Kong G, Callahan J, Hofman MS, Pattison DA, Akhurst T, Michael M, et al. High clinical and morphologic response using 90Y-DOTA-octreotate sequenced with 177Lu-DOTA-octreotate induction peptide receptor chemoradionuclide therapy (PRCRT) for bulky neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2017;44(3):476–89. https://doi.org/10.1007/s00259-016-3527-x.
Hofman MS, Michael M, Hicks RJ. 177Lu-Dotatate for Midgut Neuroendocrine tumors. N Engl J Med. 2017;376(14):1390–1. https://doi.org/10.1056/NEJMc1701616.
Bodei L, Mueller-Brand J, Baum RP, Pavel ME, Hörsch D, O'Dorisio MS, et al. The joint IAEA, EANM, and SNMMI practical guidance on peptide receptor radionuclide therapy (PRRNT) in neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2013;40(5):800–16. https://doi.org/10.1007/s00259-012-2330-6.
Kashyap R, Jackson P, Hofman MS, Eu P, Beauregard JM, Zannino D, et al. Rapid blood clearance and lack of long-term renal toxicity of 177Lu-DOTATATE enables shortening of renoprotective amino acid infusion. Eur J Nucl Med Mol Imaging. 2013;40(12):1853–60. https://doi.org/10.1007/s00259-013-2504-x.
Kong G, Thompson M, Collins M, Herschtal A, Hofman MS, Johnston V, et al. Assessment of predictors of response and longterm survival of patients with neuroendocrine tumour treated with peptide receptor chemoradionuclide therapy (PRCRT). Eur J Nucl Med Mol Imaging. 2014;41(10):1831–44. https://doi.org/10.1007/s00259-014-2788-5.
Kong G, Johnston V, Ramdave S, Lau E, Rischin D, Hicks RJ. High-administered activity in-111 octreotide therapy with concomitant radiosensitizing 5FU chemotherapy for treatment of neuroendocrine tumors: preliminary experience. Cancer Biother Radiopharm. 2009;24(5):527–33. https://doi.org/10.1089/cbr.2009.0644.
Hubble D, Kong G, Michael M, Johnson V, Ramdave S, Hicks RJ. 177Lu-Octreotate, alone or with radiosensitising chemotherapy, is safe in neuroendocrine tumour patients previously treated with high-activity 111In-octreotide. Eur J Nucl Med Mol Imaging. 2010;37(10):1869–75. https://doi.org/10.1007/s00259-010-1483-4.
Claringbold PG, Brayshaw PA, Price RA, Turner JH. Phase II study of radiopeptide 177Lu-octreotate and capecitabine therapy of progressive disseminated neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2011;38(2):302–11. https://doi.org/10.1007/s00259-010-1631-x.
Fine RL, Gulati AP, Krantz BA, Moss RA, Schreibman S, Tsushima DA, et al. Capecitabine and temozolomide (CAPTEM) for metastatic, well-differentiated neuroendocrine cancers: the pancreas Center at Columbia University experience. Cancer Chemother Pharmacol. 2013;71(3):663–70. https://doi.org/10.1007/s00280-012-2055-z.
Strosberg JR, Fine RL, Choi J, Nasir A, Coppola D, Chen DT, et al. First-line chemotherapy with capecitabine and temozolomide in patients with metastatic pancreatic endocrine carcinomas. Cancer. 2011;117(2):268–75. https://doi.org/10.1002/cncr.25425.
Claringbold PG, Price RA, Turner JH. Phase I-II study of radiopeptide 177Lu-octreotate in combination with capecitabine and temozolomide in advanced low-grade neuroendocrine tumors. Cancer Biother Radiopharm. 2012;27(9):561–9. https://doi.org/10.1089/cbr.2012.1276.
Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50(Suppl 1):122S–50S. https://doi.org/10.2967/jnumed.108.057307.
Hicks RJ. The role of PET in monitoring therapy. Cancer Imaging. 2005;5:51–7.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Rindi G. The ENETS guidelines: the new TNM classification system. Tumori. 2010;96(5):806–9.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 trial of 177Lu-Dotatate for Midgut Neuroendocrine tumors. N Engl J Med. 2017;376(2):125–35. https://doi.org/10.1056/NEJMoa1607427.
Strosberg JR, Coppola D, Klimstra DS, Phan AT, Kulke MH, Wiseman GA, et al. The NANETS consensus guidelines for the diagnosis and management of poorly differentiated (high-grade) extrapulmonary neuroendocrine carcinomas. Pancreas. 2010;39:799–800. https://doi.org/10.1097/MPA.0b013e3181ebb56f.
Welin S, Sorbye H, Sebjornsen S, Knappskog S, Busch C, Oberg K. Clinical effect of temozolomide-based chemotherapy in poorly differentiated endocrine carcinoma after progression on first-line chemotherapy. Cancer 2011; 11: 4617–4622. doi: https://doi.org/10.1002/cncr.26124.
Panzuto F, Rinzivillo M, Spada F, Antonuzzo L, Ibrahim T, Campana D, et al. Everolimus in pancreatic Neuroendocrine carcinomas G3. Pancreas. 2017;46(3):302–5. https://doi.org/10.1097/MPA.0000000000000762.
Kesavan M, Claringbold PG, Turner JH. Hematological toxicity of combined 177Lu-octreotate radiopeptide chemotherapy of gastroenteropancreatic neuroendocrine tumors in long-term follow-up. Neuroendocrinology. 2014;99(2):108–17. https://doi.org/10.1159/000362558.
Acknowledgements
Professor Hicks’ research is supported by a National Health and Medical Research Council of Australia Program grant and practitioner fellowship. We thank our radiopharmacists and radiochemists for their excellent support of our theranostics program and our dedicated nuclear medicine technologists and nursing staff for the care of our patients. Finally, we are grateful for the trust invested in us by our patients, their families and their managing clinicians.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest. No funding was received. All procedures performed were in accordance with the ethical standards of the institutional research committee and all patients provided informed consent for treatment.
Additional information
Sue Ping Thang and Mei Sim Lung are co-first authors.
A correction to this article is available online at https://doi.org/10.1007/s00259-017-3886-y.
Rights and permissions
About this article
Cite this article
Thang, S.P., Lung, M.S., Kong, G. et al. Peptide receptor radionuclide therapy (PRRT) in European Neuroendocrine Tumour Society (ENETS) grade 3 (G3) neuroendocrine neoplasia (NEN) - a single-institution retrospective analysis. Eur J Nucl Med Mol Imaging 45, 262–277 (2018). https://doi.org/10.1007/s00259-017-3821-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-017-3821-2