Abstract
Objective
To describe femoroacetabular posterior translation (FAPT) using dynamic hip ultrasonography (DHUS), and to determine the inter- and intra-rater reliability of hip ultrasound measurements of FAPT.
Materials and methods
The study design was a feasibility study of 13 healthy young adults (26 hips) using test–retest analysis. The data was collected prospectively over a 2-week time period. Three DHUS measurements (posterior neutral (PN), flexion, adduction, and internal rotation (PFADIR), and stand and load (PStand) were measured by four independent raters (2 senior who divided the cohort, 1 intermediate, 1 junior) at two time points for bilateral hips of each participant. Reliability was assessed by calculating the intraclass correlation coefficient (ICC) along with 95% confidence intervals (CIs) for each rater and across all raters.
Results
A total of 468 US scans were completed. The mean age of the cohort was 25.7 years (SD 5.1 years) and 54% were female. The inter-rater reliability was excellent for PFADIR (ICC 0.85 95% CI 0.76–0.91), good for PN (ICC 0.69 95% CI 0.5–0.81), and good for PStand (ICC 0.72 95% CI 0.55–0.83). The intra-rater reliability for all raters was good for PFADIR (ICC 0.60 95% CI 0.44–0.73), fair for PN (ICC 0.42 95% CI 0.21–0.59), and fair for PStand (ICC 0.42 95% CI 0.22–0.59).
Conclusion
This is the first study to present a protocol using dynamic ultrasonography to measure FAPT. DHUS measure for FAPT was shown to be reliable across raters with varying levels of ultrasound experience.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hip microinstability (HMI), defined as supra-physiologic hip motion, has gained acceptance as a unique clinical entity that may cause or contribute to hip pain [1]. HMI is thought to be due to subtle bone deficiency, peripelvic soft tissue weakness, and/or ligamentous laxity [2]. The clinical presentation may be subtle. Many patients will not report hip joint unsteadiness. Rather, they may describe a C sign. The “C” sign is a common sign seen in patients presenting with pain from the intra-articular hip joint. The patient holds his/her hand in a C shape over the superior lateral aspect of the hip with the thumb positioned posterior to the trochanter and the fingers extending into the groin. The patient may also report groin pain. Both the “C” sign and groin pain are non-specific findings for hip joint pathology [3]. Certain populations may be at risk such as athletes. Specifically, dancers have been documented to have high prevalence of hip dysplasia, hip pain (prevalence as high as 27%), as well as being described to be more hypermobile than controls [4]–[6].
Objective findings characterizing HMI with various imaging modalities are limited, though certain radiographic and MRI findings associated with hip instability have been reported. For example, Akiyama described femoroacetabular translation in 2 positions (neutral and Patrick position) comparing a cohort of normal female hips to dysplastic hips. They reported an average posterior-infero-medial femoral head translation of 1.12 mm in normal hips v. 1.97 mm in hips with dysplasia [7]. However, these findings have been thought to be suggestive but not diagnostic [8]–[10]. As hip motion is dynamic, studies have assessed hip translation at various positions and extreme range of motion using plain radiographs in dancers [11], MRI [12], and 3D CT [13]. In addition, dual fluoroscopy is another potential dynamic diagnostic tool as it has been utilized to study the biomechanics of the walk gait cycle pertaining to patients with cam-type femoroacetabular impingement [14]. Nevertheless, the only imaging modality that has been shown to reliably assess the degree of femoral head translation is ultrasound (US) [15, 16]. The ability to assess for anterior femoroacetabular translation using dynamic US has been shown to have excellent intra-rater and good to excellent inter-rater reliability [15].
Characterizing posterior hip translation through US has yet to be described. The ability to objectively quantify femoroacetabular posterior translation (FAPT) may lead to better understanding of clinical implications of common hip structural abnormalities such as the cam deformity (femoroacetabular impingement (FAI)) and acetabular dysplasia. For example, Philippon et al. and Krych et al. found that 75% and 82% of athletes with posterior hip instability episodes were found to have FAI [17, 18]. In addition, posterior hip instability has been associated with acetabular morphology such as acetabular retroversion and a decrease in posterior acetabular coverage [19]. With this, we aim to present a protocol for measuring FAPT using dynamic hip ultrasonography (DHUS) and to determine the inter- and intra-rater reliability of hip ultrasound measurements of FAPT.
Methods
The study protocol was approved by the institutional review board. The study was conducted at a tertiary pediatric hospital, which has a high-volume hip preservation program. This study utilized a test–retest analysis to analyze intra- and inter-rater reliability of DHUS in assessing FAPT.
“A total of 4 attending-level board-certified primary sports medicine physicians were utilized as ultrasound scanners. Each physician had varying levels of musculoskeletal (MSK) US experience: > 10 years (two senior level), 5–10 years (one intermediate), and one provider that was 1 year out of sports medicine fellowship training (Junior). Two physicians, both with > 10 years of MSK US experience, were each assigned a group to scan due to schedule availability of the scanning provider. Specifically, the cohorts were divided into two groups: group 1 consisted of participants #1–7 and group 2 consisted of participants #8–14. The intermediate and junior scanners performed the US scan for both cohorts. The ultrasound scans were obtained over a 2-week time period, each week comprised of 2 days of scanning. In total, there were 4 days of scanning. On week 1, participants #1–7 attended day 1 and participants #8–14 attended day 2. The group was asked to return 2 weeks later to complete the scans in a similar fashion.”
The DHUS assessments were performed, and data was collected at a total of 4 days over a 2-week period as described above. Thirteen participants were included in the study—1 participant was excluded, and the reason for exclusion is described below. Each participant had both hips scanned by 3 providers. Each hip was considered a unique ultrasound examination, and in turn, 26 hips were assessed. Three scans were obtained for each hip. This was repeated twice, 2 weeks apart. A total of 468 scans were obtained for the study.
Study participants
Fourteen participants, who were employees at the pediatric hospital, were recruited for the study using an internal advertisement. None of the participants were involved with the study design, data collection, data analysis, or manuscript preparation. All were in good health with no known underlying history of hip pathology. Demographics were collected on each participant including age, sex, height, weight, BMI, and 9-point Beighton score. Hypermobility was defined as Beighton ≥ 5/9 [20, 21]. Participants with hip pain and a history of prior hip surgery were excluded. One participant was only able to attend 1 visit and therefore was not included in the data analysis. The final cohort consisted of 13 participants. Both hips of each participant were used as an independent data point resulting in a total of 26 hips. Each participant was provided with an incentive of a $50 Amazon gift card per visit.
FAPT US protocol
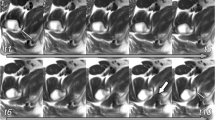
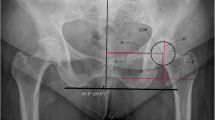
The measurements of FAPT were collected for 3 patient positions. The first position is the neutral (PN) or baseline position (Fig. 1A and B). The patient is in the lateral decubitus position with the hip being scanned facing up. The side being scanned has both the hip and knee in neutral. The contralateral hip is flexed to 90° to neutralize the pelvis and lumbar spine. The second position (PFADIR) simulates the posterior apprehension test. The position begins with the PN position as described above. The scanned hip is then passively flexed to 110°, adducted, and internally rotated (Fig. 2A and B). The third position is weight bearing and loading of the posterior hip (PStand). The individual is standing with their feet facing forward and shoulder width apart. They then flex their spine and reach over to the contralateral foot with their hands (Fig. 3A). Ultrasound measurements of FAPT were obtained using an internal software, which is a ruler tool included in the ultrasound machine. Measurements were obtained by determining the position of the femoral head in relation to the acetabulum (Figs. 1C, 2C, and 3B). A negative reading indicates the femoral head is below the acetabulum.
A–C A The first ultrasound position, termed posterior neutral or baseline position (PN), shows the subject lying in the lateral decubitus position. The scanned hip and knee on the ipsilateral side are both in the neutral position, while the contralateral hip is flexed to 90°. B Illustration showing the placement of the ultrasound probe, which is placed in parallel to the femur. C Example of the measurement of posterior femoroacetabular translation of the PN position. An internal software was used to calculate the position of the femoral head as it relates to the acetabulum. The vertical distance from the tip of the acetabulum to the sclerotic margin of the femoral head represents femoral head translation
A–C A The second ultrasound position, termed flexion, adduction, and internal rotation (PFADIR), is intended to simulate the posterior apprehension test. The position begins with the posterior neutral (PN) position (Fig. 1A). The scanned hip is then passively flexed to 110°, adducted, and internally rotated. B Illustration showing the placement of the ultrasound probe, which is placed in parallel to the femur. C Example of the measurement of posterior femoroacetabular translation of the PFADIR position
A–B A The third ultrasound position is termed the stand and load position (PStand). The individual is standing with their feet facing forward and shoulder width apart. The patient flexes their spine and reaches over to the contralateral foot with their hands. B Example of the measurement of posterior femoroacetabular translation of the PStand position
Statistical analysis
Demographic characteristics were summarized for the cohort by frequency and percent, mean and standard deviation (SD), or median and interquartile range (IQR), as appropriate. Each of the three DHUS measurements across all hips was summarized by mean and SD by rater level (junior, 0–5 years of experience; intermediate, 5–10 years of experience; and senior, 10 or more years of experience) and by first and second read. Intra-rater reliability was assessed by calculating the intraclass correlation coefficient (ICC) along with 95% confidence intervals (CIs) for each rater and across all raters. An ICC model was used, which is a two-way mixed effects model to assess consistency for a single rater. Inter-rater reliability was assessed by estimating ICCs across all three raters for the first read, the second read, and across all reads along with 95% CIs. An ICC model was used, which is a two-way random effects model to assess absolute agreement over the average of three random raters. Interpretations of reliability coefficients were based on the cutoffs by Fleiss and Cicchetti and Sparrow: < 0.40, poor; 0.40–0.59, fair; 0.60–0.74, good; and > 0.74, excellent [22]. Power analysis found that a sample of 26 measurements across three raters provided more than 80% power to test for ICC values of 0.4 to 0.8 against null hypotheses 0.30 units lower than the sample estimate with alpha set to 5%.
Results
Demographics
DHUS measurements for thirteen subjects (54% female), with a mean age of 26 years (range, 19–38), taken at two separate time points by three independent raters were reviewed. Over 1/3 of the cohort were hypermobile. The mean FAPT measurements for the three US positions of neutral, PFADIR, and PStand were 3.6 mm (SD 3.2 mm), 10.5 mm (SD 3.9 mm), and 8.2 mm (SD 4.1 mm), respectively (Table 1).
US measurements by rater experience
The US measurements of each rater are highlighted in Table 2. Due to the variability in measurements, no differences were statistically discernible across rater experience level (Table 2). For the junior rater, the absolute difference in measurement between read 1 and read 2 was 1.5 mm, 1.5 mm, and 0.7 mm for the neutral, PFADIR, and PStand, respectively. For the intermediate rater, the absolute difference in measurement between read 1 and read 2 was 0.7 mm, 0.8 mm, and 1.9 mm for the neutral, PFADIR, and PStand, respectively. For the senior raters, the absolute difference in measurement between read 1 and read 2 was 1.3 mm, 0.2 mm, and 0.8 mm for the neutral, PFADIR, and PStand, respectively (Table 2).
Inter- and intra-rater reliability
Inter-rater reliability ranged from good to excellent for read one and read two (Table 3).
Inter-rater reliability was lowest, although good, for the neutral measurement and was highest and excellent for the PFADIR measurement (Table 3).
Intra-rater reliability ranged from fair to good (Table 4). Intra-rater reliability was good and highest for the PFADIR measurement (Table 4). The intra-rater reliability was fair for the neutral and PStand positions (Table 4). Intra-rater reliability ranged from poor to fair for the junior rater, from poor to excellent for the intermediate rater, and from poor to fair for the senior rater (Table 4).
Discussion
This study is the first to propose an ultrasound protocol to assess femoroacetabular posterior translation (FAPT) using 3 measurements. These measurements and positions were designed with the intentions of understanding posterior femoroacetabular motion and the dynamic changes at various positions: baseline (posterior neutral), simulating the posterior hip apprehension test (posterior, flexion, adduction, and internal rotation), and to assess the hip in the weightbearing position (posterior standing).
The use of DHUS has been proposed as a point-of-care tool in diagnosing hip microinstability (HMI)—a condition that remains challenging to diagnose, especially in the athlete population whereby the hip joint demands are often much greater than for the non-athlete. Moreover, posterior femoroacetabular instability and impingement in the athletes and performing artist athletes is thought to contribute to posterior acetabular chondral damage population seen uniquely in some groups. By gaining a better understanding of posterior hip micro instability measured on dynamic US, we can correlate this finding to pain profile and articular and femoral cartilage damage patterns seen on MR imaging and bony changes seen on radiographs. Together, this information will serve to guide hip preservation efforts when treating complex hip pain.
The main finding of our study was that DHUS of FAPT demonstrated good to excellent inter-rater reliability and fair to good intra-rater reliability. Another notable finding was that US measurements did not vary across physician rater experience. The findings of our study offer a strategy to objectively quantify hip translation. Furthermore, our study will support clinical integration of DHUS for FAPT when evaluating complex hip pain.
The use of DHUS in evaluating joint motion is not novel. d’Hemecourt et al. introduced an US protocol to evaluate anterior femoral head translation, demonstrating excellent inter- and intra-rater reliability for neutral and anterior apprehension patient positions [15]. The use of US in quantifying joint mobility has been described in shoulders. Krarup et al. reported a significant difference in anterior shoulder translation when comparing affected shoulders to individuals without shoulder instability; 4.9 mm v. 1.9 mm (P < 0.01) [23]. In addition, Henderson et al. characterized the end range glenohumeral translation with application of an accessory passive force and ultrasound imaging [24].
Outside of ultrasonography, other imaging modalities have been investigated on its ability to provide objective findings for the diagnosis of HMI. The utilization of x-rays was illustrated by Mitchell et al., who was able to measure hip subluxation in elite ballet dancers using anteroposterior radiographic views by calculating the difference in the distance of the hip center position at the neutral position v. split position. They identified a 1.41 mm subluxation distance difference between the 2 positions [11]. Other imaging modalities such as 3D CT and MRI have also described in vivo hip translation. Cvetanovich et al. used a 3D CT software to quantify hip translation in adults with symptomatic FAI. The 3D software quantified the femoral head translation between the neutral and FABER positions to be 0.84 ± 0.37 mm. Moreover, they reported a posterior translation of 0.10 ± 0.54 mm in their cohort [13]. This amount of translation is much less than our findings of 3.6 mm (SD 3.2 mm) in the neutral and 10. 5 mm (SD 3.9 mm) in the posterior apprehension position. This difference may be from the patient position used to obtain each measurement. The use of the FABER position by Cvetanoovich et al. may underestimate FAPT as this position has been described to cause the femoral head to translate anteriorly and thus stressing the anterior hip joint and labrum [25, 26]. The cohort of Cvetanovich et al. were primarily participants with CAM femoroacetabular impingement. The exact location of the impingement, however, was not characterized—this may have contributed to the underestimation of FAPT in situations where posterior impingement is present. In addition, 3D MRI has characterized hip translation in patients with hip dysplasia. Akiyama et al. reported a mean translation of 4.10 ± 1.41 mm between the neutral and FABER position in patients with hip dysplasia [27]. Similarly using 3D MRI, Gilles et al. and Charbonnier et al. reported a mean translation of 2.12 ± 0.79 mm and 5.14 ± 1.28 mm at extreme range of motion when performed by professional dancers, respectively [12, 28]. The direction of the translation, however, was no specified. Although x-rays, 3D CT, and 3D MRI have demonstrated its ability to assess for in vivo hip translation, the use of ultrasound allows for a dynamic assessment that permits for real-time patient feedback and symptom localization to imaging findings. Ultrasound also eliminates radiation exposure and is more cost-effective than CT and MRI [29, 30].
There are (a few) limitations to this study to consider. We assumed that each hip (used) was an independent data point, even though we scanned both hips of each participant. As this was a study aimed at evaluating the reliability of a novel protocol, we felt this assumption would not affect our findings. In addition, we used 2 senior-level physician scanners who divided the cohort with each scanning half of the participants. Although having an additional senior scanner may theoretically improve the reliability results, it strengthens our data as more scanners—and therefore more chances for variability—were included in the data collection. Lastly, ultrasonography is operator-dependent, and findings may be difficult to replicate. To address this limitation, the study utilized 4 US scanners with a range of MSK US experience.
To our knowledge, this is the first study to describe an ultrasound protocol to evaluate FAPT. HMI can be difficult to diagnose, but dynamic hip ultrasound may be a tool to provide a clinical objective measurement in quantifying hip motion for the athlete with complex hip pain. Future studies are needed to establish normative values of hip translation for athletes within various sports including, for example, ice hockey athletes, swimmers, gymnasts, and figure skaters. In addition, variables such as sex, hip morphology, and ligamentous laxity will be considered.
Data availability
The data that support the findings of this study are available from the corresponding author, [HL], upon reasonable request.
References
Kalisvaart MM, Safran MR. Microinstability of the hip–it does exist: etiology, diagnosis and treatment. J Hip Preserv Surg. 2015. https://doi.org/10.1093/jhps/hnv017.
Safran MR. Microinstability of the hip - gaining acceptance. J Am Acad Orthop Surg. 2019. https://doi.org/10.5435/JAAOS-D-17-00664.
Shu B, Safran MR. Hip instability: anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011. https://doi.org/10.1016/j.csm.2010.12.008.
Harris JD, Gerrie BJ, Varner KE, Lintner DM, McCulloch PC. Radiographic prevalence of dysplasia, cam, and pincer deformities in elite ballet. Am J Sports Med. 2016;44(1):20–7. https://doi.org/10.1177/0363546515601996.
Trentacosta N, Sugimoto D, Micheli LJ. Hip and groin injuries in dancers: a systematic review. Sports Health. 2017;9(5):422–7. https://doi.org/10.1177/1941738117724159.
Skwiot M, Śliwiński G, Milanese S, Śliwiński Z. Hypermobility of joints in dancers. PLoS One. 2019;14(2):0212188. https://doi.org/10.1371/journal.pone.0212188.
Akiyama K, Sakai T, Koyanagi J, Yoshikawa H, Sugamoto K. Evaluation of translation in the normal and dysplastic hip using three-dimensional magnetic resonance imaging and voxel-based registration. Osteoarthr Cartil. 2011;19:6. https://doi.org/10.1016/j.joca.2011.01.017.
Packer JD, et al. Capsular thinning on magnetic resonance arthrography is associated with intra-operative hip joint laxity in women. J Hip Preserv Surg. 2020. https://doi.org/10.1093/jhps/hnaa018.
Packer JD, et al. The cliff sign: a new radiographic sign of hip instability. Orthop J Sport Med. 2018. https://doi.org/10.1177/2325967118807176.
Woodward RM, Vesey RM, Bacon CJ, White SG, Brick MJ, Blankenbaker DG. Microinstability of the hip: a systematic review of the imaging findings. Skeletal Radiol. 2020. https://doi.org/10.1007/s00256-020-03516-7.
Mitchell RJ, et al. Radiographic evidence of hip microinstability in elite ballet. Arthrosc - J Arthrosc Relat Surg. 2016. https://doi.org/10.1016/j.arthro.2015.12.049.
Gilles B, et al. MRI-based assessment of hip joint translations. J Biomech. 2009. https://doi.org/10.1016/j.jbiomech.2009.03.033.
Cvetanovich GL, et al. Assessment of hip translation in vivo in patients with femoracetabular impingement syndrome using 3-dimensional computed tomography. Arthrosc Sport Med Rehabil. 2020. https://doi.org/10.1016/j.asmr.2019.12.002.
Lewis CL, Uemura K, Atkins PR, Lenz AL, Fiorentino NM, Aoki SK, Anderson AE. Patients with cam-type femoroacetabular impingement demonstrate increased change in bone-to-bone distance during walking: a dual fluoroscopy study. J Orthop Res. 2023;41(1):161–9. https://doi.org/10.1002/jor.25332.
D’Hemecourt PA et al. Can dynamic ultrasonography of the hip reliably assess anterior femoral head translation?. 2019. https://doi.org/10.1097/CORR.0000000000000457.
Sahr ME, Endo Y, Sink EL, Miller TT. Dynamic ultrasound assessment of hip instability and anterior and posterior hip impingement. Skeletal Radiol. 2023. https://doi.org/10.1007/s00256-022-04264-6.
Philippon MJ, Kuppersmith DA, Wolff AB, Briggs KK. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthrosc - J Arthrosc Relat Surg. 2009. https://doi.org/10.1016/j.arthro.2008.09.013.
Krych AJ, Thompson M, Larson CM, Byrd JW, Kelly BT. Is posterior hip instability associated with cam and pincer deformity? Clin Orthop Relat Res. 2012;470(12):3390–7. https://doi.org/10.1007/s11999-012-2468-3.
Novais EN, Ferrer MG, Williams KA, Bixby SD. Acetabular retroversion and decreased posterior coverage are associated with sports-related posterior hip dislocation in adolescents. Clin Orthop Relat Res. 2019;477(5):1101–8. https://doi.org/10.1097/CORR.0000000000000514.
Juul-Kristensen B, Røgind H, Jensen DV, Remvig L. Inter-examiner reproducibility of tests and criteria for generalized joint hypermobility and benign joint hypermobility syndrome. Rheumatology. 2007;46:12. https://doi.org/10.1093/rheumatology/kem290.
Schlager A, et al. Inter- and intra-rater reliability for measurement of range of motion in joints included in three hypermobility assessment methods. BMC Musculoskelet Disord. 2018;19:1. https://doi.org/10.1186/s12891-018-2290-5.
Charter RA. A breakdown of reliability coefficients by test type and reliability method, and the clinical implications of low reliability. J Gen Psychol. 2003. https://doi.org/10.1080/00221300309601160.
Krarup AL, Court-Payen M, Skjoldbye B, Lausten GS. Ultrasonic measurement of the anterior translation in the shoulder joint. J Shoulder Elb Surg. 1999;8:2. https://doi.org/10.1016/s1058-2746(99)90006-x.
Henderson N, Worst H, Decarreau R, Davies G. Ultrasound measurements and objective forces of glenohumeral translations during shoulder accessory passive motion testing in healthy individuals. Int J Sports Phys Ther. 2016;11:5.
Crawford MJ, Dy CJ, Alexander JW, Thompson M, Schroder SJ, Vega CE, Patel RV, Miller AR, McCarthy JC, Lowe WR, Noble PC. The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res. 2007;465:16–22. https://doi.org/10.1097/BLO.0b013e31815b181f.
Dy CJ, Thompson MT, Crawford MJ, Alexander JW, McCarthy JC, Noble PC. Tensile strain in the anterior part of the acetabular labrum during provocative maneuvering of the normal hip. J Bone Jt Surg. 2008;90:7. https://doi.org/10.2106/JBJS.G.00467.
Akiyama K, Sakai T, Koyanagi J, Yoshikawa H, Sugamoto K. In vivo hip joint contact distribution and bony impingement in normal and dysplastic human hips. J Orthop Res. 2013;31:10. https://doi.org/10.1002/jor.22414.
Charbonnier C, et al. Assessment of congruence and impingement of the hip joint in professional ballet dancers: a motion capture study. Am J Sports Med. 2011. https://doi.org/10.1177/0363546510386002.
Bierig SM, Jones A. Accuracy and cost comparison of ultrasound versus alternative imaging modalities, including CT, MR, PET, and angiography. J Diagnostic Med Sonography. 2009;25:3. https://doi.org/10.1177/8756479309336240.
Lentz B, Fong T, Rhyne R, Risko N. A systematic review of the cost-effectiveness of ultrasound in emergency care settings. Ultrasound J. 2021;13:1. https://doi.org/10.1186/s13089-021-00216-8.
Acknowledgements
We would like to extend our appreciation and gratitude to Dr. Young-Jo Kim, Dr. Eduardo Novais, Dr. Travis Matheney, and Dr. Yi-Meng Yen for their contributions on the design of the ultrasound protocol.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Le, H.M., d’Hemecourt, P.A., Jackson, S.S. et al. Protocol and validity testing of femoroacetabular posterior translation with dynamic hip ultrasonography. Skeletal Radiol 53, 1287–1293 (2024). https://doi.org/10.1007/s00256-024-04560-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-024-04560-3