Abstract
Objective
To examine the effect of external hip rotation on ischiofemoral (IF) and quadratus femoris (QF) spaces using real-time kinematic MRI, with the hypothesis that hips with IF and QF space narrowing have distinct motion patterns compared with control hips.
Materials and methods
This prospective study was IRB-approved and complied with HIPAA guidelines. We recruited women (≥ 18 years) with and without ischiofemoral impingement to undergo kinematic MRI of the hips. A kinematic imaging protocol using T2-HASTE was performed beginning at maximal internal rotation followed by active external hip rotation. The duration of each acquisition was 30 s, providing 8 images/3 s. IF and QF spaces, and femoral metaphyseal and lesser trochanter centroid coordinates were measured on sequential images. Hips were classified as controls or narrowed based on IF and QF space thresholds and compared statistically throughout motion stages.
Results
The cohort comprised 12 women (24 hips; 10 control and 14 narrowed hips) aged 58 ± 10 years. External rotation caused IF space reduction of 59% in narrowed hips versus 41% in control hips. QF space decreased 71% in narrowed hips versus 50% in control hips. IF and QF spaces differed significantly between groups only when external rotation exceeded the neutral position (P < 0.02 for both). The lesser trochanter terminated more posteriorly in narrowed hips compared with controls (P = 0.03).
Conclusions
Kinematic MRI during external hip rotation in women with narrowed and control hips reveals dynamic differences in IF and QF spaces and lesser trochanter terminal position.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ischiofemoral impingement (IFI) is characterized by hip pain and quadratus femoris muscle abnormalities due to narrowing between lesser trochanter in relation to ischial tuberosity or hamstring tendons [1, 2]. Ischiofemoral (IF) narrowing was initially described on radiographs of three patients after hip surgery presenting with chronic pain, which was relieved by lesser trochanter osteotomy [3]. Subsequently, IF space narrowing was shown in surgery-naïve patients using MRI [1, 4,5,6], which demonstrated additional soft tissue features and measurement thresholds establishing the IFI syndrome. The typical presentation of IFI comprises hip pain in middle-aged women, showing on MRI a combination of narrowed IF and quadratus femoris (QF) spaces, tears, edema, or atrophy of QF muscle [1, 2]. Hip pain is variable in presentation, but is more prominent at hip external rotation and extension, usually localized to the deep gluteal region [7].
The exact etiology that leads to IFI is unknown. Prior studies have shown pelvic morphologic features that predispose to IF space narrowing, such as increased ischial and femoral neck angles [4, 6]. However, these findings reflect static assessments and can be substantially influenced by hip position at imaging [8, 9]. In a recent case report, kinematic MRI in a 58-year-old female provided preliminary evidence of how the IF space was affected by external hip rotation, being mostly narrowed by rotation of lesser and greater trochanter towards the ischium [10]. Although this finding was described in a patient with QF muscle edema, IF and QF spaces were within previously reported normal ranges. Furthermore, no comparison with range-of-motion in control hips was performed.
Our goal was to prospectively compare the range-of-motion in IFI with control hips using real-time kinematic hip MRI. We hypothesized that hips with narrowed IF and QF spaces had distinct motion patterns during external rotation compared with that of normal controls.
Materials and methods
Patients
This prospective study was approved by the Institutional Review Board and followed Health Insurance Portability and Accountability Act (HIPAA) guidelines, with individual informed consent being performed prior to imaging procedures. Women with imaging findings of IFI were identified from our institutional database of MRI examinations (pelvis and/or hip) obtained between April 2009 and April 2018. Diagnostic reports containing the term “ischiofemoral impingement,” “IFI,” or “IF impingement” were confirmed by narrowed IF and QF spaces below published thresholds [11]. These prospective participants were contacted and invited to join the study. Additional age- and sex-matched individuals were recruited using announcements posted on an approved internet platform. These additional participants were screened to have no current hip pain, history of fracture, or prior hip surgery with the intention of creating a control group. Exclusion criteria for all participants were presence of prosthesis or hardware, metal artifact that would adversely affect measures, bone or soft tissue neoplasms, fractures, and infection. A total of 12 women were recruited, yielding 24 hips that underwent real-time kinematic MRI between March 2017 and May 2018. We sought to recruit only women for this study given the preponderance of IFI in females and to avoid confounding factors that could be introduced by features of male pelvic morphology.
MRI protocol
Detailed MRI parameters are outlined in Table 1. MRI was prospectively performed on a 3.0T scanner (Siemens Trio, Erlangen, Germany), employing a phased array body-matrix coil. Briefly, our protocol had the following features:
-
subject supine, with knees extended, hips in neutral position in regard to flexion/extension, and no constraints to internal or external rotation of lower extremities;
-
static tri-plane localizer for prescription of kinematic imaging;
-
real-time kinematic axial imaging during active external hip rotation: each hip was scanned separately, using a T2-weighted Half-Fourier-Acquired Single-shot Turbo spin Echo (HASTE) pulse sequence. Participants initially positioned the hip in maximal internal rotation. Then, they actively externally rotated the hip to their personal maximum.
Prior to scanning, participants were coached on how to perform the motion inside the scanner, assessing for potential discomfort and space limitations. Participants were also encouraged to move within their level of comfort and practiced how to perform the motion, ensuring uniform speed and synchronized begin/end with the audible begin/end of HASTE pulse sequence (30-s duration). During acquisitions, one investigator remained next to the subject inside the MR suite, monitoring if motion was performed as prescribed, and repeat imaging was performed if needed. We provided an audible countdown prior to launching kinematic scanning, which once initiated, lasted 30 s and generated a stack of 8 contiguous axial images every 3 s. Therefore, 10 stacks were output from beginning to end of external hip rotation, documenting 10 unique timeframes (t1—t10) along the motion (total of 80 axial images per external rotation). No subjects underwent intravenous or intra-articular contrast injection.
Image analysis
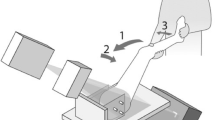
At each timeframe, we identified the axial image that best demonstrated the ischium and lesser trochanter. We used the length tool in the ImageJ software version 1.52 (http://imagej.nih.gov) to obtain the following parameters (Figs. 1 and 2) [1]:
-
IF space (length in mm): the shortest distance between lateral cortex of ischial tuberosity and medial cortex of lesser trochanter;
-
QF space (length in mm): the narrowest space for passage of quadratus femoris muscle between the lateral surface of hamstring tendons and medial surface of iliopsoas tendon or medial cortex of lesser trochanter;
-
Femoral centroid (x-y coordinates in mm): center of best-fit ellipse in medullary cavity of femoral metadiaphysis, excluding lesser trochanter;
-
Lesser trochanter centroid (x-y coordinates in mm): center of best-fit ellipse in medullary cavity of lesser trochanter.
44-year-old female, right hip (control). Sequential timeframes from kinematic MRI during external rotation. t1 represents initial state at maximal internal rotation, t5 neutral position, and t10 maximal external rotation. Solid and dotted lines show measures of IF and QF spaces, respectively. Measures were performed on all timeframes and are indicated at beginning (t1) and end (t10) of external rotation. At terminal external rotation, no significant compression of quadratus femoris muscle (arrow) is noted
52-year-old female, right hip (narrowed). Sequential timeframes from kinematic MRI during external rotation. t1 represents initial state at maximal internal rotation, t5 neutral position and t10 maximal external rotation. Best-fit ellipses (red) and solid centroids (black) were measured on all timeframes and are indicated on this figure at beginning (t1) and end (t10) of external rotation. At terminal stages of external rotation, substantial compression of quadratus femoris muscle (arrow) is noted
Two fellowship-trained musculoskeletal radiologists with 7 (FJS) and 22 (MT) years of experience performed all measurements independently, blinded to recruitment source.
Hip classification criteria
Using previously described IF and QF space thresholds from a published meta-analysis [11], we classified hips as narrowed or control using measurements from our kinematic series. We adopted this stringent methodology as it provided an objective classification parameter and to increase sensitivity to detect space narrowing throughout the range-of-motion, which can be underestimated in static imaging at a single position. Clinical symptoms, and semi-quantitative, or qualitative measures of QF muscle abnormality were not used as a criterion for hip classification, due to our focus on osseous biomechanics. Therefore, we classified hips as follows:
-
narrowed hips, with IF space ≤ 15 mm and QF space ≤ 10 mm on one or more timeframes of kinematic series;
-
control hips, with IF space > 15 mm on all timeframes of kinematic series.
Statistical analyses
Mean values between readers were used for data analyses. In order to compare kinematic changes in IF space and QF space, we sequentially plotted their averages for control versus narrowed hips. Tracking of femoral and lesser trochanter mean centroid coordinates during the kinematic series was plotted on a chart to compare the motion pattern between groups. The left hip x-coordinates were mirrored (i.e., multiplied by − 1) so trajectories from all hips could be combined into the same chart. All statistics were calculated using the JMP Pro (version 14, SAS Institute, Cary, NC) and MedCalc software (version 12.7, MedCalc, Ostend, Belgium). The intraclass correlation coefficient (ICC) measured agreement between readers regarding quantitative parameters (IF and QF space measures). Between-group IF space, QF space and IF centroid distance comparisons were performed using Wilcoxon/Kruskal-Wallis 2-sample tests, with multiple comparisons being corrected using the Bonferroni method (α/n hypotheses). Overall statistical difference between serial IF and QF space measurements was evaluated using the MANOVA repeated measures procedure in JMP. Significance level (α) was set as < 0.05. All measurements were expressed in millimeters ± standard deviation.
Results
A total of 12 women were recruited: 4 identified by previous MRI reports had bilateral IFI and 8 recruited by online advertisement–referred asymptomatic hips. Three of the asymptomatic women had bilateral IF and QF space narrowing based on published thresholds [11], and their hips were allocated to the narrowed hip group. The final study cohort comprised 24 hips of 12 women (10 control hips and 14 narrowed hips) (Fig. 3). The mean age was 58 ± 10 years (median 59, range 43–68). Ages in control and narrowed hip groups were not significantly different (p = 0.8). No subjects had history or imaging evidence of fracture, surgery, hardware, neoplasms, or infection. All subjects visited our institution for prospective kinematic MRI and were able to undergo the entire protocol.
Subject recruitment and hip classification workflow based on published thresholds [11]. IF, ischiofemoral; QF, quadratus femoris; IFI, ischiofemoral impingement
Mean measures for IF and QF spaces during external hip rotation for both groups are detailed in Table 2. ICC values were 0.96 (95% CI 0.95, 0.97) for IF space and 0.97 (95% CI 0.96, 0.98) for QF space measures, indicating a high level of inter-reader agreement. Between the initial (t1) and final (t10) timeframes, external rotation caused IF space reduction of 59% (16.3 mm) in narrowed hips versus 41% (14.1 mm) in control hips. QF space decreased 71% (12.2 mm) in narrowed hips versus 50% (10.7 mm) in control hips. During initial stages of external rotation (t1–t5), narrowed and control hips showed progressive IF space reduction without significant differences between groups (P > 0.1 after Bonferroni adjustment) (Fig. 4a). However, decrease of IF spaces diverged after t5, with lower IF spaces in narrowed hips from t6–t10 (P < 0.01 after Bonferroni adjustment). Similarly, the QF space showed progressive decrease during external rotation (Fig. 4b), with similar QF space from t1–t6 (P > 0.07 after Bonferroni adjustment). Beginning at t7, the QF space was smaller in narrowed hips (P < 0.006 after Bonferroni adjustment). The MANOVA repeated measures procedure revealed overall significant differences between controls and narrowed hips for serial measures of IF (P = 0.0005) and QF (P = 0.002) spaces.
Plotting of femoral metaphysis and lesser trochanter centroid trajectories during external rotation examined differences between control and narrowed hips. The femoral metaphysis in both groups had similar arc-shaped trajectories, with non-significant difference in position at terminal (t10) external rotation (3.4 mm, P = 0.3). However, the lesser trochanter had a markedly different trajectory between groups during external rotation. In narrowed hips, the lesser trochanter described a steep convex trajectory with significant posterior excursion, whereas in controls, it described a shallow convex trajectory on the axial plane. Accordingly, a significant difference in the posterior position of lesser trochanter at terminal (t10) external rotation was noted between narrowed and control hips (8.4 mm, P = 0.03) (Figs. 5, 6, 7, 8; Video 1).
Still images at terminal external rotation (t10) from 4 study subjects, showing centroid trajectories of femur and lesser trochanter. (a) 44-year-old and (b) 56-year-old female subjects from control group show U-shaped trajectory of lesser trochanter. (c) 52-year-old and (d) 66-year-old female subjects from narrowed hip group show posteromedial crescentic trajectory of lesser trochanter. Please view Supplementary material Video 1 for full kinematic sequences
Discussion
Our main findings are two-fold. First, we show significant IF and QF space narrowing occurs on external hip rotation only beyond the neutral position, which has important implications when considering IFI on static cross-sectional imaging. Second, we show the lesser trochanter in narrowed hips travels more posteriorly during external rotation, a feature contributing to IF and QF space narrowing. Taken together, our study describes previously unreported aspects of hip motion that provide novel insights into the biomechanics of IFI.
Narrowing of IF space was initially noted on radiographs by Johnson [3] on three patients with persistent post-surgical hip pain: two patients had prior total hip arthroplasty and one had a proximal femoral osteotomy. Hypertrophic changes of medial proximal femur and lesser trochanter suggested impaction against the ischium and represented a potential source of pain. In all cases, relief was achieved by lesser trochanter resection, which widened the IF space [3]. However, this phenomenon was seen as a potential surgical complication, and its existence in surgically naïve hips was unknown.
In a study using MRI, the IFI syndrome was defined by Torriani et al. [1] consisting of a combination of IF and QF space narrowing, secondary QF muscle abnormalities, and affecting middle-aged women with pain in the gluteal region. Notably, these cases had no prior surgery or metallic implants. Measurement thresholds have been proposed for osseous (IF) and soft-tissue (QF) spaces through which the QF muscle traverses [1, 11], and currently support the diagnosis of IFI. Subsequent studies examined morphologic features of proximal femur and pelvis, pointing towards a higher femoral inclination angle (i.e., hip valgus) and larger hamstring tendon cross-sectional area in IFI [4], as well as increased ischial and femoral neck angles [4, 6]. Although the etiology of IFI in native hips is still debated and potentially linked to congenital pelvic and/or femoral morphology, acquired changes in hip alignment such as from osteoarthritis and surgery may play a role [1, 4, 5]. Importantly, presence of QF muscle abnormalities (e.g., atrophy, edema, and tears) is variable and may coexist with seemingly normal spaces [12]. Furthermore, static cross-sectional imaging with flexed hips or prone positioning may artifactually widen IF and QF spaces, potentially confounding the diagnosis of IFI [13]. In such situations, QF muscle abnormalities may be visible with normal-appearing IF and QF spaces, requiring positional correction or range-of-motion imaging to confirm the presence of IFI.
In a case report, Singer et al. [10] provided the first MRI demonstration of femoral range-of-motion in a patient with presumed IFI. The authors noted that passive external hip rotation in a 58-year-old woman caused narrowing between trochanters relative to ischial tuberosity and hamstring tendons [10]. Although QF muscle edema was present, IF and QF spaces were normal. Serial measures throughout motion were unavailable, and hip range-of-motion was not compared with control hips. In an ultrasound study of normal volunteers, Finnoff et al. [9] showed the widest IF space occurred with hip abduction and internal rotation (52 mm), whereas hip adduction and external rotation resulted in the narrowest IF space (31 mm). Our study builds upon these studies, performing multiple measures on kinematic MRI during active external hip rotation, comparing cohorts of control with narrowed hips.
We found that significant IF and QF space narrowing occurred only during the latter stages of external rotation. Narrowed hips had higher amplitude of IF and QF space reduction during external rotation, which was significantly more prominent beyond t6 and t7, respectively. Taken together, these findings raise important considerations for imaging subjects with suspected IFI. Conventional positioning for hip and pelvis MRI usually comprises neutral knee position with feet strapped in internal rotation or perpendicular to table surface [13]. This common practice may lead to IF and QF space underestimation. In our study, hips were classified as narrowed when below-threshold IF and QF spaces [11] were detected at any point throughout the range-of-motion. We found no significant differences between narrowed and control hips on earlier timeframes between maximal internal rotation to neutral position (t1–t5). The significant difference in spaces between groups beyond neutral position (t6—t10) suggests external rotation is required to properly diagnose IFI. This also explains why some IFI patients undergoing static MRI with neutral/internal hip rotation may show QF muscle abnormalities with deceptively normal IF and QF spaces, creating a confusing picture. In a prior study on normal volunteers, Johnson et al. [13] found that supine hip flexion and prone neutral position overestimated IF space by 12 mm and 3 mm respectively, when compared with a supine neutral position. Imaging in maximal external rotation may help uncover pathologic IF or QF space narrowing, regardless of QF muscle abnormalities being present.
Another observation from our study relates to the trajectory of femoral centroids during external rotation. Control hips externally rotated without significantly narrowing of IF space, with the lesser trochanter ending closer to midline but with minimal posterior translation. At terminal external rotation, the lesser trochanter described a U-shaped trajectory avoiding collision with the ischium. On the other hand, external rotation in narrowed hips caused the lesser trochanter centroid to move posteriorly while translating to the midline, describing a posteromedial crescentic trajectory. Taken together, these findings further support a multi-factorial etiology for IFI, likely including structural and dynamic components. As previously noted, IFI has been linked to structural features of pelvic [6] and femoral [4, 14] morphology that may contribute to space narrowing. Femoral and potentially acetabular morphology could play a role in affecting the rotation arc during hip motion, which combined with abnormal femoral and ischial morphology may lead to IFI. Although these morphologic features may be acquired, such as in osteoarthritis and valgus deformity, the preponderance of IFI in females across a wide age spectrum suggests superimposed congenital or developmental factors [1, 6, 11, 15]. Certain features of hip biomechanics such as hip abductor insufficiency may dynamically contribute to narrowing during hip motion [16]; however, the role of gluteal tendon tears, neurogenic weakness, or muscle inhibition remains uncertain. The combined effect of structural and dynamic factors may play a role in the distinct motion paths during external rotation seen in our study. However, since our study design was limited to documenting external rotation during real-time kinematic MRI, further investigations are needed to establish a link between such factors.
Our study should be interpreted considering certain limitations. First, hip motion was performed without weight-bearing, and physiologic loading may augment the abnormal relationship between osseous structures, especially during ambulation. Weight-bearing MR systems are commercially available and have the potential to further elucidate joint biomechanics [17]; however, it may have limitations in characterizing the mechanics of common hip motions such as sitting or walking. The magnet bore length and diameter of our MR system limited our study to external hip rotation, not allowing for proper hip extension that may be an important source of symptoms [18]. Again, this additional kinematic test could be addressed by future studies employing open-magnet designs. Of note, bidimensional fluoroscopy has a strong potential to provide insight regarding osseous relationships during specific hip motions, as shown in a prior study in which IF spaces in healthy female participants were reduced during standing and walking [8]. Standardization for specific hip rotational positions was not possible across our cohort, since patients had varied ranges-of-motion, body habitus, and level of comfort for maximal hip positions. However, our approach of allowing for external rotation within patient’s constraints may adequately reflect their expected motions and permitted demonstration of significant differences between groups. Finally, given the limited cohort size in our study, control hips were selected based on thresholds for osseous structures alone (IF space).
Strengths of our study include comparison of narrowed and control hips imaged using active hip motion and characterization of range-of-motion patterns in each group that were previously unrecognized.
In conclusion, our study furthers the understanding of IFI by demonstrating the effect of external hip rotation in narrowing of IF and QF spaces in women and showing distinct motion patterns in narrowed hips. Future studies employing kinematic imaging during usual activities are necessary to further elucidate the biomechanical abnormalities in IFI, which will greatly influence surgical and clinical management in this population.
References
Torriani M, Souto SCL, Thomas BJ, Ouellette H, Bredella MA. Ischiofemoral impingement syndrome: an entity with hip pain and abnormalities of the quadratus femoris muscle. AJR Am J Roentgenol. 2009;193:186–90.
Patti JW, Ouellette H, Bredella MA, Torriani M. Impingement of lesser trochanter on ischium as a potential cause for hip pain. Skelet Radiol. 2008;37:939–41.
Johnson KA. Impingement of the lesser trochanter on the ischial ramus after total hip arthroplasty. Report of three cases. J Bone Joint Surg Am. 1977 Mar;59(2):268–9.
Tosun O, Algin O, Yalcin N, Cay N, Ocakoglu G, Karaoglanoglu M. Ischiofemoral impingement: evaluation with new MRI parameters and assessment of their reliability. Skelet Radiol. 2012;41:575–87.
Ali AM, Teh J, Whitwell D, Ostlere S. Ischiofemoral impingement: a retrospective analysis of cases in a specialist orthopaedic centre over a four-year period. Hip Int J Clin Exp Res Hip Pathol Ther. 2013;23(3):263–8.
Bredella MA, Azevedo DC, Oliveira AL, Simeone FJ, Chang CY, Stubbs AJ, et al. Pelvic morphology in ischiofemoral impingement. Skelet Radiol. 2014 Nov:249–53.
Carro LP, Hernando MF, Cerezal L, Navarro IS, Fernandez AA, Castillo AO. Deep gluteal space problems: piriformis syndrome, ischiofemoral impingement and sciatic nerve release. Muscles Ligaments Tendons J. 2016 Sep;6(3):384–96.
Atkins PR, Fiorentino NM, Aoki SK, Peters CL, Maak TG, Anderson AE. In vivo measurements of the ischiofemoral space in recreationally active participants during dynamic activities: a high-speed dual fluoroscopy study. Am J Sports Med. 2017 Oct;45(12):2901–10.
Finnoff JT, Bond JR, Collins MS, Sellon JL, Hollman JH, Wempe MK, et al. Variability of the ischiofemoral space relative to femur position: an ultrasound study. Am Acad Phys Med Rehabil. 2015;(April):1–8.
Singer A, Clifford P, Tresley J, Jose J, Subhawong T. Ischiofemoral impingement and the utility of full-range-of-motion magnetic resonance imaging in its detection. Am J Orthop Belle Mead NJ. 2014 Dec;43(12):548–51.
Singer AD, Subhawong TK, Jose J, Tresley J, Clifford PD. Ischiofemoral impingement syndrome: a meta-analysis. Skelet Radiol. 2015 Jun;44(6):831–7.
O’Brien SD, Bui-Mansfield LT. MRI of quadratus femoris muscle tear: another cause of hip pain. AJR Am J Roentgenol. 2007 Nov;189(5):1185–9.
Johnson AC, Hollman JH, Howe BM, Finnoff JT. Variability of ischiofemoral space dimensions with changes in hip flexion: an MRI study. Skelet Radiol. 2017 Jan;46(1):59–64.
Gómez-Hoyos J, Schröder R, Reddy M, Palmer IJ, Martin HD. Femoral neck anteversion and lesser trochanteric retroversion in patients with ischiofemoral impingement: a case-control magnetic resonance imaging study. Arthrosc J Arthrosc Relat Surg. 2016 Jan 1;32(1):13–8.
Goldberg-Stein S, Friedman A, Gao Q, Choi J, Schulz J, Fornari E, et al. Narrowing of ischiofemoral and quadratus femoris spaces in pediatric ischiofemoral impingement. Skelet Radiol. 2018 Nov;47(11):1505–10.
DiSciullo AA, Stelzer JW, Martin SD. Dynamic ischiofemoral impingement: case-based evidence of progressive pathophysiology from hip abductor insufficiency: a report of two cases. JBJS Case Connect. 2018 Dec;8(4):e107.
Shapiro LM, Gold GE. MRI of weight-bearing and movement. Osteoarthr Cartil. 2012 Feb;20(2):69–78.
Gómez-Hoyos J, Martin RL, Schröder R, Palmer IJ, Martin HD. Accuracy of 2 clinical tests for Ischiofemoral impingement in patients with posterior hip pain and endoscopically confirmed diagnosis. Arthrosc J Arthrosc Relat Surg. 2016 Jul 1;32(7):1279–84.
Funding
This study was funded by the MGH Department of Radiology Ralph Schlaeger Award (fund #230050).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was IRB-approved and HIPAA compliant. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vicentini, J.R.T., Martinez-Salazar, E.L., Simeone, F.J. et al. Kinematic MRI of ischiofemoral impingement. Skeletal Radiol 50, 97–106 (2021). https://doi.org/10.1007/s00256-020-03519-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-020-03519-4