Abstract
We report on a 40-year-old male with a 9-month-long history of snapping of his right hip caused by a previously undescribed etiology of internal extra-articular snapping hip, namely due to a localized tenosynovial giant cell tumor. Both dynamic ultrasound evaluation and MRI proved to be crucial in the diagnosis of this rare entity. Auto-provocation of the snapping showed an anterior hip mass moving posteriorly to the psoas tendon which elucidated the pain and clicking sensation. Subsequent MRI demonstrated a peripheral low-intensity rim due to hemosiderin deposition around the synovial mass which is indicative for pigmented villonodular tenosynovitis. Treatment consisted of arthroscopic shaver burr resection. Immediately postoperatively, the snapping sensation could not be provoked anymore by the patient. The purpose of reporting on this case report is to emphasize several successive learning points. First, dynamic ultrasound aids in diagnosis and differentiation of the types of snapping hip. Second, specific MRI features are suggestive of tenosynovial giant cell tumor, recognizing these traits may prevent delayed diagnosis and subsequent aggravated clinical course. Third, localized pigmented villonodular tenosynovitis around the hip may present as an internal extra-articular snapping hip and is of consideration in the differential diagnosis of recurrent snapping hip.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tenosynovial giant cell tumors (TGCT), formerly known as pigmented villonodular tenosynovitis (PVNS), form a group of benign but proliferative and potentially locally aggressive diseases [1]. They originate from synovia of joints, bursa, or tendon sheaths and are classified into two categories: a localized form (giant cell tumor of tendon sheath (GTS-TS) or localized TGCT) and a diffuse form (diffuse pigmented villonodular tenosynovitis (PVNS) or diffuse type giant cell tumor (D-TGCT)) [2]. Both manifestations have distinct characteristics. The former mostly presents as a single slow-growing mass adjacent to tendons or small joints such as the hands but is also seen around larger joints. A common presenting complaint is a painless swollen joint or a lump, but the mass effect of the lesion can cause pain and discomfort if left untreated [2]. The latter is more aggressive; the multiple nodules most often affect the knee, hip, or ankle joint, and may cause a more concerning clinical presentation [2]. Swift diagnosis is important since the natural history of the disorder may lead to ongoing pain, affect daily functioning, or cause joint destruction and subsequent osteoarthritis [3]. Preoperative imaging is crucial to localize and characterize the lesion and to map possible multiplicity in order to prevent recurrence.
Here, we report on a 40-year-old male with a 9-month-long history of snapping of his right hip caused by a previously undescribed etiology of internal extra-articular snapping hip, namely due to localized TGCT. A snapping hip (SH) or “coxa saltans” is a condition characterized by a palpable or audible snapping sensation during hip joint movement [4]. While the etiology may be diverse, the disorder is typically caused by the slipping of a tendon over a bony protrusion. SH is divided into three main categories: external extra-articular (external SH), internal extra-articular (internal SH), and intra-articular. External extra-articular snapping comprises the most frequently encountered form and is provoked by the iliotibial band or gluteus maximus tendon slipping over the greater trochanter [4]. The internal extra-articular manifestation emerges from the iliopsoas tendon sliding over structures located posteriorly to the tendon itself such as the iliopectineal eminence, the femoral head, or the ridge of the lesser trochanter. Additionally described mechanisms include subluxation of the long head of the biceps femoris over the ischial tuberosity or slippage of the iliofemoral ligament across the femoral head [5]. Intra-articular snapping may be caused by loose bodies or (osteo)chondral fragments, labral tears, or synovial chondromatosis [4]. While the hip joint is a relatively commonly affected large joint by diffuse type PVNS, a localized TGCT originating from the psoas bursa leading to a snapping hip presentation has not yet been described [6, 7]. Both dynamic ultrasound evaluation and MRI proved to be crucial in the diagnosis of this rare entity. Auto-provocation of the snapping showed an anterior hip mass moving posteriorly to the psoas tendon which elucidated the pain and clicking sensation, thus confirming the diagnosis of an internal extra-articular cause of snapping hip. Subsequent MRI demonstrated a peripheral low-intensity rim due to hemosiderin deposition around the synovial mass which is suggestive for PVNS [8].
The purpose of reporting this case report is to emphasize several successive learning points. First, dynamic ultrasound aids in diagnosis and differentiation of the types of SH. Second, specific MRI features are suggestive of TGCT; recognizing these traits may prevent delayed diagnosis. Third, localized PVNS around the hip may present as an internal extra-articular snapping hip and should be considered a possible cause of recurrent snapping hip.
Case report
A 40-year-old male high-level amateur cyclist was referred to our hospital due to a painful snapping sensation in his right hip during the past 9 months. Initially, the snapping occurred during cycling and later also while walking upstairs. No previous trauma was reported, and the patient presented with a blank medical history. Clinical examination revealed right groin tenderness on palpation, without palpable swelling, and an audible “click” and snapping sensation in deep hip flexion and internal rotation. Further clinical and neurovascular examination was unremarkable. The decision was made to obtain conventional radiographs of the right hip—which did not show any abnormalities—and a dynamic ultrasound. The latter revealed a mixed echogenic extra-articular mass (dimensions 4.8 × 2.4 × 1.7 cm) located anteriorly at the level of the hip joint and in close contact with the iliopsoas tendon. During dynamic evaluation and auto-provocation of the snapping, the mass shifted from the lateral to the posterior margin of the psoas tendon and this maneuver induced the pain (Fig. 1).
A, B Anteroposterior and lateral standard radiographs of the right hip. No clear joint effusion, focal soft-tissue mass, or bone erosions were noted on these images. C, D Dynamic ultrasound images taken before (C) and after (D) provocation of the snapping hip. C With the hip in extension, adduction, and neutral rotation, the mass is located lateral from the psoas tendon. D Mobilizing the hip into deep flexion, abduction, and external rotation made the mass shift posteriorly to the psoas tendon which induced the painful and clicking sensation. LAT lateral, ANT anterior, MED medial, ILIAC iliopsoas tendon, RIP localized mass
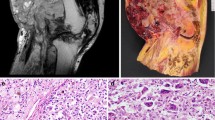
Subsequent MRI with intravenous gadolinium contrast (3 T, Ingenia, Philips Healthcare) confirmed the size and localization of the mass (Fig. 2). A significant amount of hemosiderin was present in the lesion without notable edge enhancement after IV contrast. Based upon clinical examination and imaging, the diagnosis of internal extra-articular snapping hip due to localized PVNS of the psoas bursa was made and a subsequent hip arthroscopy was performed. Over the course of the procedure, no intra-articular lesions were visualized. During inspection of the peripheral compartment, the mass only became visible after resection of the synovium located between the medial synovial fold and the zona orbicularis. Several biopsy samples were collected for histopathological analysis and afterwards the lesion was completely resected using an arthroscopic shaver burr (Fig. 3). Immediately postoperatively, the snapping sensation could not be provoked by the patient and his rehabilitation occurred uneventfully with a return to progressive cycling at 2 weeks postoperatively. Histopathological analysis confirmed the diagnosis of a localized TGCT (Fig. 4). Informed consent was given by the patient to present anonymized data and images.
A T1-weighted turbo spin echo axial image prior to contrast administration. The well-delineated mass (straight arrows, dimensions 4.8 × 2.4 × 1.7 cm) shows an overall very low signal intensity and is near the psoas tendon (90° arrows), anteriorly of the hip joint. B, C T2*-weighted sagittal and axial sequences. Note the spotty low signal intensities with bloom artifacts due to the hemosiderin deposition (yellow asterisks). D T1-weighted short tau inversion recovery sagittal image with edge enhancement
A Representative histological image showing CD68+ multinucleated osteoclast-like giant cells, × 20 magnification. B–D Representative histological images using × 20, × 10, and × 2.5 magnification for B, C, and D, respectively. Note the presence of hemosiderin (brown streaks), foamy histiocytes, and mononuclear component. On the low-power view (D), there is a typical nodular and lobular architecture with fibrous bands dividing the separate lobules
Operative arthroscopic images. A Unremarkable intra-articular findings in the central compartment. B Inspection of the peripheral compartment did not show any pathology at the level of the medial synovial fold (black arrow) and zona orbicularis (white arrow). C After resection of the synovium at the level of medial synovial fold and zona orbicularis, the lesion became visible. Note the macroscopic presentation with a typical yellow and red-brown color (black arrow). D The lesion was resected completely until the psoas muscle (white arrow) was visible
Discussion
Localized TGCTs are rare and have an incidence of 8.4 patients per million [6]. There is no real consensus on the etiology and pathogenesis of the disease [9]. The diffuse form affects the entire synovium of the affected joint whereas the localized form is characterized by a single or nodular mass and is surrounded by normal synovial tissue. While the former is more common around the hip than the latter, here an uncommon occurrence of localized TGCT of the psoas bursa caused a recurrent internal extra-articular snapping hip in a 40-year-old male patient without any accompanying intra-articular manifestations. Treatment consisted of arthroscopic debridement and resection of the nodular mass in the peripheral hip compartment and healing occurred uneventfully.
The use of dynamic ultrasound proved essential in differentiating the type of snapping hip in this patient. The main advantage consisted of the combined temporal and spatial resolution which allowed real-time visualization of the psoas tendon slipping over the anterior hip mass during auto-provocation testing [10]. Piechota et al. comprehensively described their ultrasound protocol when considering internal snapping hip pathology [11]. In short, they start with a static scan using a linear 9- to 12-MHz transducer comparing the anterior hip region of both hips in a supine position. Subsequently, using a sagittal oblique plane, the femoral head is identified as a landmark structure and the transducer is turned to the oblique axial plane which allows for a clear evaluation of the psoas tendon. The hip is then flexed and internally rotated to provoke the snapping sensation; however, the precipitating movement may differ between patients and should be considered on an individual basis [11].
Localized TGCT most often presents as a well-delineated nodular mass in close localization to the original tendon on MR imaging with a size ranging between 0.5 and 5 cm [3]. Further features reflect the histological composition of the lesion [12]. Microscopically, TGCTs are characterized by variable proportions of osteoclast-like giant cells, mononuclear cells, and hemosiderin. The latter is an iron-storage complex located within the synovial lining cells and exhibits ferromagnetic properties that alter the MRI signal [13]. Subsequently, low to intermediate spotty signal intensities are seen on both T1- and T2-weighted images within the proliferative masses due to local changes in susceptibility [2]. Collagenous proliferation further contributes to the typical low signal intensity [12]. Gradient echo sequences are more sensitive to the magnetic changes and may be best suited to show hemosiderin deposits and blooming artifacts [13]. The amount of hemosiderin is variable and in some cases even absent. On T1-weighted images, the signal intensity is markedly enhanced after gadolinium injection because of the proliferative capillaries present [14]. If there is doubt about the diagnosis, a tissue biopsy is necessary as sarcoma is a rare entity to consider in the differential diagnosis [3].
When TGCT affect the hip, it mostly concerns the diffuse type combined with an intra-articular origin [3, 7]. This case is the first to report the peripheral involvement of a localized form around the psoas tendon without any intra-articular connection. Kallas et al. have described a case of diffuse PVNS causing a large retroperitoneal mass in close continuity with the psoas muscle and tendon; however, the lesion originated from within the joint, causing associated cartilage destruction [15]. In our patient, the intra-articular evaluation was unremarkable, and the lesion only surfaced after resecting the medial synovium of the peripheral compartment. The gold standard of treatment for localized type lesions consists of surgical resection; however, some advocate for an open approach to reduce risk or recurrence [2]. Either way, histological tissue examination is mandatory [2].
In summary, dynamic ultrasound evaluation offers a non-invasive and highly valuable diagnostic tool when dealing with patients that present with an unclear cause of snapping hip. Although rare, a localized tenosynovial giant cell tumor is of consideration in the differential diagnosis of psoas snapping. MR imaging of these lesions displays characteristic ferromagnetic features due to the presence of hemosiderin deposition.
References
Palmerini E, Staals EL, Maki RG, Pengo S, Cioffi A, Gambarotti M, et al. Tenosynovial giant cell tumour/pigmented villonodular synovitis: outcome of 294 patients before the era of kinase inhibitors. Eur J Cancer. 2015;51(2):210–7. https://doi.org/10.1016/j.ejca.2014.11.001
Van Der Heijden L, Gibbons CLMH, Dijkstra PDS, Kroep JR, Van Rijswijk CSP, Nout RA, et al. The management of diffuse-type giant cell tumour (pigmented villonodular synovitis) and giant cell tumour of tendon sheath (nodular tenosynovitis). J Bone Jt Surg Ser B. 2012;94(B):882–8.
Gouin F, Noailles T. Localized and diffuse forms of tenosynovial giant cell tumor (formerly giant cell tumor of the tendon sheath and pigmented villonodular synovitis). Orthop Traumatol Surg Res. 2017;103(1S):S91–7. https://doi.org/10.1016/j.otsr.2016.11.002
Yen YM, Lewis CL, Kim YJ. Understanding and treating the snapping hip. Sports Med Arthrosc. 2015;23:194–9.
Potalivo G, Bugiantella W. Snapping hip syndrome: systematic review of surgical treatment. HIP Int. 2017;27:111–21.
Ehrenstein V, Andersen SL, Qazi I, Sankar N, Pedersen AB, Sikorski R, et al. Tenosynovial giant cell tumor: incidence, prevalence, patient characteristics, and recurrence A registry-based cohort study in Denmark. J Rheumatol. 2017;44:1476–83.
Steinmetz S, Rougemont AL, Peter R. Pigmented villonodular synovitis of the hip. Efort Open Rev. 2016;1:260–6.
Lynskey SJ, Pianta MJ. MRI and thallium features of pigmented villonodular synovitis and giant cell tumours of tendon sheaths: a retrospective single centre study of imaging and literature review. Br J Radiol. 2015;88:1–7.
Stephan SR, Shallop B, Lackman R, Kim TWB, Mulcahey MK. Pigmented villonodular synovitis: a comprehensive review and proposed treatment algorithm. JBJS Rev. 2016;4:1–9.
Deslandes M, Guillin R, Cardinal É, Hobden R, Bureau NJ. The snapping iliopsoas tendon: new mechanisms using dynamic sonography. Am J Roentgenol. 2008;190:576–81.
Piechota M, Maczuch J, Skupiński J, Kukawska-Sysio K, Wawrzynek W. Internal snapping hip syndrome in dynamic ultrasonography. J Ultrason. 2016;16:296–303.
Wan JMC, Magarelli N, Peh WCG, Guglielmi G, Shek TWH. Imaging del tumore gigantocellulare delle guaine tendine. Radiol Medica. 2010;115:141–51.
Cheng XG, You YH, Liu W, Zhao T, Qu H. MRI features of pigmented vilonodular synovitis (PVNS). Clin Rheumatol. 2004;23:31–4.
De Beuckeleer L, De Schepper A, De Belder F, Van Goethem J, Marques MCB, Broeckx J, et al. Magnetic resonance imaging of localized giant cell tumour of the tendon sheath (MRI of localized GCTTS). Eur Radiol. 1997;7:198–201.
Kallas KM, Vaughan L, Haghighi P, Resnick D. Pigmented villonodular synovitis of the hip presenting as a retroperitoneal mass. Skeletal Radiol. 2001;30:469–74.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vervaecke, A.J., Declercq, H., Wetzels, K. et al. Localized tenosynovial giant cell tumor: a rare case of snapping hip. Skeletal Radiol 51, 2205–2210 (2022). https://doi.org/10.1007/s00256-022-04064-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-022-04064-y