Abstract
Objectives
To develop and evaluate a deep learning (DL)–based system for measuring leg length on full leg radiographs of diverse patients, including those with orthopedic hardware implanted for surgical treatment.
Methods
This study retrospectively assessed 2767 X-ray scanograms of 2767 patients who did or did not have orthopedic hardware implanted between January 2016 and December 2019. A cascaded DL model was developed to localize the relevant landmarks on the pelvis, knees, and ankles required for measuring leg length. Statistical analysis was performed using the correlation coefficient analysis and Bland–Altman plots to assess the agreement between the reference standard and DL-calculated lengths.
Results
Testing data comprised 400 radiographs from 400 patients. Of these radiographs, 100 were from patients with orthopedic hardware implanted in their pelvis, knees, or ankles. For all testing data, leg lengths derived from the DL-based measurement system, with or without internal fixation devices, showed excellent agreement with the reference standard (femoral length, r = 0.99 (P < .001); root mean square error (RMSE) = 0.17 cm; mean difference, − 0.01 ± 0.17 cm; 95% limit of agreement (LoA), − 0.35 to 0.34; tibial length, r = 0.99 (P < .001); RMSE = 0.17 cm; mean difference, − 0.02 ± 0.17 cm, 95% LoA, − 0.34 to 0.31; and full leg length, r = 1.0 (P < .001); RMSE = 0.19 cm; mean difference, 0.05 ± 0.18 cm; 95% LoA, − 0.31 to 0.40). The mean time for leg length measurement for each patient using the DL-based system was 8.68 ± 0.18 s.
Conclusion
The DL-based leg length measurement system could provide similar performance to radiologists in terms of accuracy and reliability for a diverse group of patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Leg length discrepancies (LLDs), in which the lengths of the paired lower extremity limbs are unequal, are considered orthopedic deformities [1]. LLDs are relatively common and found in as many as 40–70% of adult and pediatric populations [1,2,3]. The causes of LLDs include idiopathic developmental abnormalities, scoliosis, fixed pelvic tilt, orthopedic degenerative disorders, and surgical disorders, such as joint replacements [1,2,3,4,5]. In particular, studies have suggested that LLD is associated with several lower limb and lumbar biomechanical conditions and musculoskeletal disorders, such as foot pronation, low back pain, osteoarthritis of the knee and hip joints, and stress fractures [1, 6,7,8,9,10]. Therefore, it is crucial that the leg length be accurately and reliably measured to allow for proper diagnosis and treatment planning.
Direct and indirect clinical measurement of leg length relies on the palpation of bony landmarks, which is prone to errors [7]. Therefore, due to their accuracy and reliability, radiographs are considered the gold standard for measuring leg length [1, 7,8,9,10]. However, manual leg length measurements using radiographs, while cognitively simple for a radiologist, are time-consuming tasks [10]. Computer-assisted quantification programs may allow for automatic leg length measurements without these limitations. The recent development of a deep learning–based (DL-based) approach showed promising results for LLD measurement on limited datasets [10].
This study aimed to evaluate the accuracy and reliability of DL-based leg length measurements using full leg radiographs of a diverse group of patients, including those with internal fixation devices that were implanted for surgical treatment, by comparing the performance of a DL-based system to that of trained radiologists.
Materials and methods
Study population and dataset
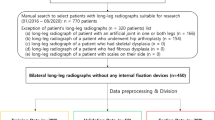
The appropriate institutional review board approved this retrospective study, and the requirement for informed consent was waived due to the retrospective design of the study. We identified 2791 X-ray scanograms that were taken between January 2016 and December 2019 (Innovision; DongKang Medical Systems Co. Ltd., Seoul, South Korea), and a total of 2767 X-ray scanograms from 2767 patients were manually selected for this study. Of these scanograms, there are approximately twice as many female patients as male patients, and 328 were from patients with internal fixation devices implanted in the pelvis, knees, or ankles. Patient’s radiographic studies were excluded from the study if they (a) overlapped (n = 0); (b) had segmental views of the hips, knees, and ankles (n = 21); (c) had skeletal dysplasia (n = 0); (d) had external orthopedic hardware (n = 0); or (e) had undergone radiography with a scale at their side (n = 3). Full leg, standing, anteroposterior view radiographs that included both lower extremities from the hips to the ankles were obtained through an image acquisition system (HPACS software; HealthHub Co. Ltd., Seoul, South Korea). The image resolution was approximately 3000 × 8000 pixels in a 24-bit gray scale JPEG format. All images were de-identified before use. The patient demographic statistics are summarized in Table 1.
Patient studies were split into training, validation, and testing data without overlaps (Fig. 1). Images with internal fixation devices in the pelvis, knee, or ankle only accounted for 9.7% (183/1,895) and 9.5% (45/472) of the total number of training and validation data, respectively. To address the class imbalance, we applied a simple data augmentation scheme based on image cropping and horizontal flip. A given radiograph was manually cropped at all four corners, while ensuring that no body parts were lost. Training data were used to train DL models for detecting regions of interest (ROI) containing relevant landmarks for leg length measurement as well as segmenting bones, including implanted prostheses, from ROI images. ROIs in the individual radiographs and the femoral area and knee and ankle joint masks that were within corresponding ROIs were manually annotated by a board-certified radiologist. These annotations were used as the ground truth for ROI detection and segmentation. Details of the training and validation datasets for deep learning models are summarized in Table E1 and E2.
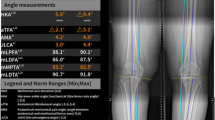
Reference standard for leg length measurements
A board-certified radiologist performed the leg length measurements on full leg, standing, anteroposterior radiographs in the testing data. Here, femoral, tibial, and full leg lengths were measured based on the mechanical axis [11]. The point of interest (POI) for measurements in the femoral area was the top of the femoral head or prosthetic femoral head. The POI for the knee joint was the most distal end of the medial femoral condyle or the prosthesis that replaced it. The POI for the ankle joint was the center of the tibial plafond or the prosthesis that replaced it. Leg length measurements on the full leg, standing radiograph are presented in Fig. 2.
An illustration of the leg length measurement process. A The deep learning–based system had a cascade architecture. The ROI detection network first detected six ROIs that contained the relevant landmarks that were needed to perform the measurements. The ROI segmentation networks then segmented the bones, including prostheses, within ROIs. The segmentation masks were processed using image processing algorithms to identify the POIs that corresponded to the relevant landmarks in the pelvis, knees, and ankles. Finally, the leg length was measured by calculating the distance between the extracted pixels; B POIs for the leg length measurement based on mechanical axes. Best viewed in color. ROI, region of interest, POI, point of interest
Development of the DL-based, fully automated, leg length measurement system
The system had a cascade architecture that comprised three stages (Fig. 2). The first stage involved locating six ROIs and identifying their classes. Based on the ROI’s location (e.g., femoral area, knee joint and ankle joint on the left and right sides) and the presence of internal fixation devices in the ROI, the ROIs were classified into 12 different classes. We customized the single shot multibox detector [12] architecture for ROI detection. The second stage comprised 12 segmentation DL models, each of which was responsible for segmenting bones in the designated ROIs. All segmentation DL models shared the same model architecture; however, they were trained with different training data. For the segmentation DL model, we customized the standard U-Net [13] model. In the third stage, the bone contours in the segmentation masks were traversed using conventional image processing algorithms to find the accurate POI locations. Once all six POIs were identified, the final leg lengths on both sides were calculated. For training and testing, we used a single NVIDIA Titan-XP GPU (NVIDIA, Santa Clara, CA, USA). The code is accessible at https://github.com/RTOSChansu/llm/. See Appendix E1 for additional details of the model development.
The ROI detection performance was evaluated using the mean average precision that was the mean of the average precision scores [14] for the 12 different ROI classes. The ROI segmentation performance was evaluated using the Dice score that was calculated using the following formula: (2 × TP)/((TP + FP) + (TP + FN)), where TP, FP, and FN indicated the number of true positive, false positive, and false negative pixels, respectively.
Statistical analysis
The accuracy and reliability of the DL-based leg length measurements were evaluated using the concordance correlation coefficient (CCC) and Pearson correlation coefficient (r) in relation to a reference standard. A Bland–Altman plot was also used to assess the agreement between the reference leg lengths and the leg length that was calculated through DL. Additionally, the mean squared error (MSE), mean absolute error (MAE), and root mean square error (RMSE) were used to evaluate the accuracy of the leg length that was calculated through DL in relation to a reference standard. All statistical analyses were performed using Minitab software (Minitab 17.3.1; Minitab LLC, Sate College, PA, USA) and R-programming (version 3.1.2 [2014]; https://www.r-project.org/).
Besides analyzing all testing data, subgroup analysis was performed to determine if the implanted orthopedic hardware influenced the accuracy and reliability of the DL-based leg length measurement system. Testing data were grouped into two disjoint subgroups: subgroup 1, which included patients with any internal fixation devices implanted in the pelvis, knees, or ankles; and subgroup 2, which included patients who had no orthopedic hardware.
Results
Study participants
In total, 2767 patients (mean age ± standard deviation, 56 ± 16 years; age range, 8–91 years; 975 men and 1972 women) were included in our study. Among those patients, 328 had internal fixation devices implanted in their pelvis, knees, or ankles (Fig. 1). Patient studies were split into training, validation, and testing data (68%, 1895/2767; 17%, 472/2767; and 15%, 400/2767), each of which comprised patients who did or did not have implanted orthopedic hardware. The baseline characteristics of the study population are described in Table 1.
Performance of the DL models for ROI detection and segmentation
The DL models for ROI detection and segmentation performed excellently with the entire testing dataset. There were no cases of failure with the ROI detection and the resultant mean average precision was 0.98. The subsequent segmentation masks generated by the DL models overlapped significantly with the corresponding ground truth. The average Dice score of the 12 segmentation DL models was 0.98. The DL models’ performance in ROI detection and segmentation is summarized in Table 2.
Accuracy and reliability of DL-based leg length measurements
The mean time for leg length measurements by the DL-based system was 8.68 ± 0.18 s for each patient when using a single NVIDIA Titan-XP GPU (NVIDIA, Santa Clara, CA, USA). The leg length that was derived from the DL-based system showed excellent agreement with the reference standard (femoral length, CCC = 0.99, r = 0.99; tibial length, CCC = 0.99, r = 0.99; and full leg length, CCC = 1.0, r = 1.0; P < 0.001 for all correlations) (Table 3).
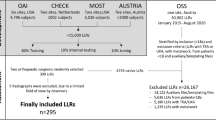
According to the Bland–Altman agreement analysis, there was no systematic bias between the reference standard and lengths that were calculated through the DL-based system. The mean differences ± standard deviation between the two femoral, tibial, and full leg length measurements were – 0.01 ± 0.17 cm, – 0.02 ± 0.17 cm, and 0.05 ± 0.18 cm, respectively. The 95% limits of agreement (LoA) between the two femoral, tibial, and full leg length measurements ranged from – 0.35 to 0.34, – 0.34 to 0.31, and – 0.31 to 0.40, respectively (Fig. 3).
Bland–Altman plots of the reference leg lengths and leg lengths that were calculated using DL. The x-axis represents the mean of the reference and DL-calculated lengths (cm), whereas the y-axis represents the difference between the reference and DL-calculated lengths (cm). A All the testing data; B subgroup 1; C subgroup 2. DL deep learning, SD standard deviation
The DL-based system’s high measurement accuracy was also observed with the MSE, MAE, and RMSE (femoral length, MSE = 0.03 cm, MAE = 0.14 cm, RMSE = 0.17 cm; tibial length, MSE = 0.03 cm, MAE = 0.13 cm, RMSE = 0.17 cm; and full leg length, MSE = 0.04 cm, MAE = 0.15 cm, RMSE = 0.19 cm) (Table 3).
Subgroup analysis
The DL-based measurement system’s performance was not influenced by the presence of internal fixation devices in the pelvis, knees, or ankles. For both subgroups, it was observed that the two measurements correlated significantly (subgroup 1, CCC = 0.99, 0.99, and 1.0; r = 0.99, 0.99, and 1.0 for femoral, tibial, full leg lengths, respectively; subgroup 2, CCC = 0.99, 0.99, and 1.0; r = 0.99, 0.99, and 1.0 for femoral, tibial, and full leg lengths, respectively; P < 0.001 for all correlations) (Table 3).
The Bland–Altman plots also demonstrated that the accuracy and reliability of the DL-based leg length measurements were not affected by the internal fixation devices that were implanted in patients’ lower limbs (Fig. 3). For subgroup 1, the mean differences ± standard deviation between the two femoral, tibial, and full leg length measurements were – 0.01 ± 0.18 cm (95% LoA: − 0.37 to 0.35); 0.06 ± 0.14 cm (95% LoA: − 0.32 to 0.21); and − 0.05 ± 0.21 cm (95% LoA: − 0.47 to 0.36), respectively. For subgroup 2, the mean differences between the two femoral, tibial, and full leg length measurements were 0.00 ± 0.17 cm (95% LoA: − 0.34 to 0.33); − 0.01 ± 0.17 cm (95% LoA: − 0.34 to 0.33); and 0.05 ± 0.18 cm (95% LoA: − 0.31 to 0.40), respectively.
For subgroup 1, the RMSEs for the femoral, tibial, and full leg lengths were 0.18 cm, 0.15 cm, and 0.22 cm, respectively, whereas the corresponding errors of the femoral, tibial, and full leg lengths in subgroup 2 were 0.17 cm, 0.17 cm, and 0.18 cm, respectively. Both MAE and MSE also showed similar levels of errors as RMSE. The results from the performance evaluation are summarized in Fig. 3 and Table 3, and examples cases of leg lengths that are calculated using the DL-based system are presented in Fig. 4.
Radiographic images with the DL-calculated leg lengths. The lines were generated by a DL-based automatic leg length measurement system. The blue line represents the femoral length, and the red line represents the tibial line. The green line represents the full leg length. Images on the right side demonstrated that the DL-based system was able to accurately and reliably identify relevant landmarks that were required to measure the leg length. A A patient with no orthopedic hardware implanted; B A patient with internal fixation devices implanted in the pelvis and knees; C A patient with internal fixation devices implanted in the ankle. RLL right full leg length, RFL right femoral length, RTL right tibial length, LLL left full leg length, LFL left femoral length, LTL left tibial length, DL deep learning
Discussion
We developed and validated a deep learning–based fully automated leg length measurement system using full leg standing anteroposterior view radiographs that included both lower extremities from the hips to the ankles. For all the testing data that randomly included patients who did or did not have internal fixation devices in the pelvis, knees, or ankles, the ability of the DL-based system for detecting and segmenting regions of interest was excellent (mean average precision = 0.98, average Dice score = 0.98). Additionally, strong correlations were observed between the reference standard and separated femur, tibia, and full leg lengths that were calculated using deep learning (femoral length, r = 0.99 (P < 0.001), root mean square error (RMSE) = 0.17 cm, mean absolute error (MAE) = 0.14 cm, mean difference − 0.01 ± 0.17 cm, 95% limit of agreement (LoA) − 0.35 to 0.34; tibial length, r = 0.99 (P < 0.001), RMSE = 0.17 cm, MAE = 0.13 cm, mean difference − 0.02 ± 0.17 cm, 95% LoA − 0.34 to 0.31; and full leg length, r = 1.0 (P < 0.001), RMSE = 0.19 cm, MAE = 0.15 cm, mean difference 0.05 ± 0.18 cm, 95% LoA – 0.31 to 0.40). The average measurement time per radiograph for the deep learning–based system was 8.68 ± 0.18 s. There were no significant differences in performance when the subgroups were assessed according to the presence of internal fixation devices (subgroup 1, r = 0.99 (P < 0.001), 0.99 (P < 0.001), and 1.0 (P < 0.001); RMSE = 0.18 cm, 0.15 cm, and 0.22 cm; MAE = 0.14 cm, 0.11 cm, 0.16 cm for the femoral, tibial, and full leg lengths, respectively; subgroup 2, r = 0.99 (P < 0.001), 0.99 (P < 0.001), and 1.0 (P < 0.001); RMSE = 0.17 cm, 0.17 cm, and 0.18 cm; MAE = 0.14 cm, 0.14 cm, 0.15 cm for the femoral, tibial, full leg lengths, respectively). For subgroups 1 and 2, the mean differences between the two measurements were small with a 95% confidence interval in femoral, tibial, and full leg lengths (subgroup 1, − 0.01 ± 0.18 cm, − 0.06 ± 0.14 cm, and − 0.05 ± 0.21 cm; 95% LoA − 0.37 to 0.35, − 0.32 to 0.21, and − 0.47 to 0.36, respectively; subgroup 2, 0.00 ± 0.17 cm, − 0.01 ± 0.17 cm, and 0.08 ± 0.16 cm; 95% LoA − 0.34 to 0.33, − 0.34 to 0.33, and − 0.24 to 0.39, respectively). These findings indicated that there was no systematic bias between the two measurements.
Zheng et al. [10] demonstrated that the measurement of LLD in pediatric patients on radiographs could be automated and performed rapidly by deep learning algorithm (CCC = 0.99, r = 0.99 (P < 0.001), MAE = 0.45 cm for separated femur and tibia lengths; CCC = 0.99, r = 0.99 (P < 0.001), MAE = 0.45 cm for the full leg length). Our findings similarly suggest that automated and precise measuring of leg length on full leg standing radiographs of diverse patients, including those with orthopedic hardware implanted for surgical treatment, can be enabled by deep learning algorithms. As in our study, Zheng et al.’s approach employed a multi-step process for image segmentation, in which the DL model first roughly split radiographs into left and right leg images, then finely segmented femurs and tibias on the unilateral full-limb images. However, there were differences in our methodology. We believe that these differences were the key to our system’s improved generalization capability. First, to accurately recognize and localize relevant landmarks on the hips, knees, and ankles, we included the radiographs of both pre- and postoperative patients who had internal orthopedic hardware implanted for training DL models. To the best of our knowledge, this is the first study to assess the effectiveness of DL-based leg length measurements for patients with internal fixation devices. Second, instead of exploring the entire image to segment the femurs and tibias, our approach only allowed ROIs that enclosed relevant landmarks (e.g., POIs) to be considered; thus, it was more effective in capturing discriminative local features. Third, we adopted state-of-the-art attention mechanisms to enable the fine segmentation of ROIs where prostheses were present.
This study had some limitations. First, we did not evaluate the DL models by using external datasets that are completely independent from those used for model training. Utilizing additional data from multiple institutions for model training is needed to improve the DL models’ generalizability. Second, patients with skeletal dysplasia were not included in either training or testing. Third, we did not consider the angulation of the femoral and tibial axes. Fourth, we used only a single model of the equipment for X-ray scanogram acquisition.
In conclusion, we developed and evaluated a clinically relevant deep learning–based leg length measurement system that performed similar to radiologists in terms of accuracy and reliability. The performance of our system was not influenced by the orthopedic hardware implanted in lower extremity limbs of patients. This will be helpful in reducing repetitive and time-consuming task of leg length measurement required for surgical planning and for the diagnosis and prognosis of relevant disease. Further prospective studies should be performed to extend this deep learning–based system to provide comprehensive set of leg geometry measurements by increasing diversity of and numbers contained in the training data for deep learning models, as well as by enhancing feature learning capability of deep learning models.
Abbreviations
- CCC:
-
Concordance correlation coefficient
- DL:
-
Deep learning
- LLD:
-
Leg length discrepancies
- LoA :
-
Limit of agreement
- MAE:
-
Mean absolute error
- MSE:
-
Mean squared error
- POI:
-
Point of interest
- r :
-
Pearson correlation coefficient
- RMSE:
-
Root mean square error
- ROI:
-
Region of interest
References
Gurney B. Leg length discrepancy. Gait Posture. 2002;15:195–206.
Yong M, Park S. Leg length discrepancy to influence on kinematic changes of the pelvis and the hip during gait. J Kor Phys Ther. 2019;31:368–71.
Khamis S, Carmeli E. A new concept for measuring leg length discrepancy. J Orthop. 2017;14:276.
Meermans G, Malik A, Witt J, Haddad F. Preoperative radiographic assessment of limb-length discrepancy in total hip arthroplasty. Clin Orthop Relat Res. 2011;469:1677–82.
Blake RL, Ferguson H. Limb length discrepancies. J Am Podiatr Med Assoc. 1992;82:33–8.
Rannisto S, Okuloff A, Uitti J, et al. Leg-length discrepancy is associated with low back pain among those who must stand while working. BMC Musculoskelet Disord. 2015;16:110.
Ahmed K. Leg length discrepancy: assessment and secondary effects. Ortho & Rheum Open Access. 2017;5:555678.
Sabharwal S, Kumar A. Methods for assessing leg length discrepancy. Clin Orthop Relat Res. 2008;466:2910–22.
Murray KJ, Azari MF. Leg length discrepancy and osteoarthritis in the knee and lumbar spine. J Can Chiropr Assoc. 2015;59:226–37.
Zheng Q, Shellikeri S, Huang H, Hwang M, Sze RW. Deep learning measurement of leg length discrepancy in children based on radiographs. Radiology. 2020;296:152–8.
Rungprai C, Goetz JE, Arunakul M, et al. Validation and reproducibility with a biplanar imaging system versus conventional radiography. Foot Ankle Int. 2014;35:1166–75.
Liu W, Anguelov D, Erhan D et al (2016) SSD: Single shot multibox dector. In: Leibe B., Matas J., Sebe N., Welling M. (eds) Computer Vision – ECCV 2016. ECCV 2016. Lecture Notes in Computer Science, Springer, Cham. 9905:21–37.
Ronneberger O, Fischer P, Brox T (2015) U-net: Convolutional networks for biomedical image segmentation. In: Navab N., Hornegger J., Wells W., Frangi A. (eds) Medical Image Computing and Computer-Assisted Intervention – MICCAI 2015. MICCAI 2015. Lecture Notes in Computer Science, Springer, Cham. 9351:234–241
Zhang P, Su W (2012) Statistical inference on recall, precision and average precision under random selection. Proceedings of 2012 9th International Conference on Fuzzy Systems and Knowledge Discovery (FSKD), Chongqing, China. 1348–1352
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points:
• Strong correlations (P<.001) were observed between the reference standard and lengths of the separated femurs, tibias, and full legs that were calculated through deep learning.
• The deep learning–based system measured each patient’s leg length in approximately 8.68 ± 0.18 s.
• There was no significant difference in performance noted when the radiographs of patients with internal fixation devices implanted in the pelvis, knees, or ankles were compared with those without implants.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, C.S., Lee, M.S., Byon, S.S. et al. Computer-aided automatic measurement of leg length on full leg radiographs. Skeletal Radiol 51, 1007–1016 (2022). https://doi.org/10.1007/s00256-021-03928-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-021-03928-z