Abstract
Objectives
To give a systematic overview of current diagnostic imaging options for assessment of the distal tibio-fibular syndesmosis.
Materials and methods
A systematic literature search across the following sources was performed: PubMed, ScienceDirect, Google Scholar, and SpringerLink. Forty-two articles were included and subdivided into three groups: group one consists of studies using conventional radiographs (22 articles), group two includes studies using computed tomography (CT) scans (15 articles), and group three comprises studies using magnet resonance imaging (MRI, 9 articles).The following data were extracted: imaging modality, measurement method, number of participants and ankles included, average age of participants, sensitivity, specificity, and accuracy of the measurement technique. The Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) tool was used to assess the methodological quality.
Results
The three most common techniques used for assessment of the syndesmosis in conventional radiographs are the tibio-fibular clear space (TFCS), the tibio-fibular overlap (TFO), and the medial clear space (MCS). Regarding CT scans, the tibio-fibular width (axial images) was most commonly used. Most of the MRI studies used direct assessment of syndesmotic integrity. Overall, the included studies show low probability of bias and are applicable in daily practice.
Conclusions
Conventional radiographs cannot predict syndesmotic injuries reliably. CT scans outperform plain radiographs in detecting syndesmotic mal-reduction. Additionally, the syndesmotic interval can be assessed in greater detail by CT. MRI measurements achieve a sensitivity and specificity of nearly 100%; however, correlating MRI findings with patients’ complaints is difficult, and utility with subtle syndesmotic instability needs further investigation. Overall, the methodological quality of these studies was satisfactory.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Syndesmotic injuries of the ankle are common and often present with nonspecific clinical and radiographic findings [1,2,3,4]. Approximately up to 18% of all ankle sprains and up to 23% of all ankle fractures show an additional injury of the distal tibio-fibular syndesmosis [3, 5,6,7]. Undiagnosed injuries of the syndesmosis may lead to chronic instability of the ankle joint and degenerative changes over time [4, 5, 8,9,10,11,12,13,14]. Injury can occur to any of the four ligaments that comprise the syndesmosis: the anterior inferior tibio-fibular ligament (AITFL), the interosseous membrane (IOM), the posterior inferior tibio-fibular ligament (PITFL), and the transverse tibio-fibular ligament (TTFL) [5, 15,16,17,18,19,20,21]. Additionally, the deltoid ligament stabilizes the distal syndesmosis [8]. The deltoid ligament, which consists of four superficial and two deep components, anchors the tibia medially and restrains a lateral shift of the talus in the ankle joint [22,23,24,25,26]. Deltoid injuries are commonly seen in patients with acute syndesmotic injury [9, 27,28,29,30].
Conventional (weight-bearing) radiographs (antero-posterior and mortise view), computed tomography (CT) scans and/or magnetic resonance imaging (MRI) are widely used for assessment of the distal tibio-fibular syndesmosis [9]. Due to the insufficient accuracy of conventional radiographs for detecting syndesmotic injuries, CT scans and MRI have gained popularity over the last few years [31]. However, there is heterogeneous evidence regarding the accuracy of the various measurement techniques, especially in chronic syndesmotic injuries. The objective of this article is to give a systematic overview of the current imaging options for assessment of the distal tibio-fibular syndesmosis.
Materials and methods
Search strategy
Four major medical databases were searched from inception through July 10, 2017: PubMed, ScienceDirect, Google Scholar, and SpringerLink. The bibliographies of articles of interest were additionally reviewed. There were no limitations on type of journal or publication date of the article. Articles in English, German, French and Russian were included. Following keywords were used: syndesmosis/-otic AND instability, syndesmosis/-otic AND injury, syndesmosis/-otic AND imaging, syndesmosis/-otic AND augmentation. The systematic literature search was performed by three reviewers (N.K., M.W.W., and A.B.).
Data extraction
The following data were extracted from each study: Imaging modality, measurement method, number of participants and ankles included, average age of participants, sensitivity (if mentioned), specificity (if mentioned), and accuracy of the technique (if mentioned). If a study used multiple radiographic modalities (i.e. MRI and CT scans), data for each cohort were extracted separately. For studies with multiple readers for each imaging examination, the data were averaged. Data extraction was performed by three reviewers (N.K., M.W.W., and A.B.).
Study selection
Studies were included if they were original research studies (incl. cadaver studies) that assessed the distal tibio-fibular syndesmosis using conventional radiographs/ fluoroscopy, CT scans, or MRI. Exclusion criteria consisted of studies that used incomplete data (i.e. intraoperative assessment without preoperative evaluation), studies that were published as either case reports or review articles, finite-element modeling studies, studies including less than five participants and studies written in another language than English, German, French, or Russian. Furthermore, studies that did not have their full text available on the aforementioned sources were excluded. The study selection process was conducted independently by three reviewers (N.K., M.W.W., and A.B.). The decision to include or exclude the study was made based on a group consensus agreement. Disagreements were discussed and a group consensus was reached.
Study quality assessment
The Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) tool was used to assess the methodological quality (Table 1) [32]. Studies which solely characterize the distal tibio-fibular syndesmosis in healthy ankles were excluded from assessment. In total, 16 studies underwent quality assessment: seven studies using X-rays or fluoroscopy, three studies using CT scans, and six studies using MRI. Two studies investigated both the diagnostic accuracy of X-ray and MRI. Each of the studies were evaluated for risk of bias regarding patient selection, index test, reference standard, and flow and timing (e.g. time between index test and reference standard) [32]. Additionally, each study was evaluated for concerns of applicability regarding patient selection, index test, and reference standard.
Statistics
Sensitivity and specificity were calculated if they were not mentioned in the study using a fourfold table. The quality of the studies included in our analysis was assessed by using both internal and external validity measures within the framework provided by the QUADAS-2 tool [32].
Results
Included studies
The initial screening showed 9,862 studies which potentially could be included (Fig. 1). After removing all duplicates and reviewing the title and abstract of each study, 8900 studies were excluded. Another 920 studies were excluded if they met any of the following exclusion criteria: review article, case report, <5 patients included, incomplete data set or not available as a full-text article. Data screening was done according to the guidelines of “Preferred Reporting Items for Systematic Review and Meta-Analyses” (PRISMA). The remaining 42 articles were subdivided into three groups: group one consists of studies using conventional radiographs (22 articles), group two includes studies using CT scans (15 articles), and group three comprises studies using MRI (9 articles). If one study included more than one imaging modality (e.g. conventional radiographs and CT scans), it was included in more than one group (four articles).
Study characteristics
With the exception of four studies using conventional radiographs, one study using CT scans, and one study using MRI, every included study reported the average patient age. Overall, the average patient age was 42.4 years in group one, 42.7 in group two, and 32.9 in group three. A total of 3,246 patients (3,441 ankles) were assessed. Conventional radiography or fluoroscopy was the most popular diagnostic tool (1,587 ankles), followed by CT scans (1,250 ankles), and lastly by MRI (604 ankles). Assessment of the syndesmosis using conventional radiographs was most frequently done on weight-bearing antero-posterior (AP) radiographs in combination with mortise view, while axial images were preferred for assessments done using CT scans. Assessments using MRI often included coronal, sagittal, and axial images and allowed direct visualization of the syndesmosis.
Using conventional radiographs or fluoroscopy, data were available for healthy ankles, patients suffering from isolated syndesmotic injuries (e.g. high ankle sprains), and patients with an ankle fracture in combination with a syndesmotic injury. Two studies investigated chronic syndesmotic injuries in patients with history of an ankle fracture, nine studies investigated acute syndesmotic injuries (isolated and in combination with an ankle fracture), eight studies assessed the syndesmosis in healthy ankles, and three studies included cadavers. Studies using CT scans included data from healthy ankles (nine studies), ankle fractures in combination with a syndesmotic injury (three studies investigated acute and one study investigated chronic syndesmotic injuries in patients with history of an ankle fracture) but not from isolated syndesmotic injuries. Two additional studies used cadavers for assessment of the syndesmosis. Studies using MRI included results from healthy ankles (two studies), isolated syndesmotic injuries (two studies, whereas both included a mixed cohort of patients suffering from isolated syndesmotic injuries and patients suffering from syndesmotic injuries in combination with an ankle fracture), and ankle fractures (one study and two studies including the above mentioned mixed cohort).
Measurement methods
Conventional radiographs or fluoroscopy (AP, mortise, and lateral view) used 13 different measurement techniques, while CT scans and MRI used 29 and 10, respectively (direct visualization of the ligaments excluded). Summaries of commonly used measurement techniques using conventional radiographs are shown in Figs. 2 and 3. The three most common techniques used for assessment of the syndesmosis in conventional radiographs or fluoroscopy are the tibio-fibular clear space (TFCS), tibio-fibular overlap (TFO), and medial clear space (MCS). Two cadaver studies used stress views (one study using plain radiographs, one study using fluoroscopy), while none of the studies using healthy volunteers or patients performed stress radiographs. In case of an ankle fracture, sensitivity and specificity (when additionally using the Weber and Orthopedic Trauma Association classification for decision-making) were 47.0 and 100%, respectively [33]. Using the Lauge-Hansen Classification instead of the Weber or Orthopedic Trauma Association (OTA) classification, sensitivity and specificity were each 92.0% [33]. In acute isolated syndesmotic injuries, sensitivity/ specificity was 82.0%/ 75.0% for TFCS, 36.0%/ 78.0% for TFO, and 73.0%/ 59.0% for MCL [34]. MRI was used as a reference standard in both studies. Using arthroscopy as a reference standard, sensitivity/ specificity was found to be 48.8%/ 100% for TFCS and TFO (AP view) and 63.6%/ 100% for MCS, talo-crural angle and talar tilt (mortise view, study included patients with ankle fractures) [28]. Two more studies assessed the sensitivity and specificity but had mixed cohorts (ankle fracture in combination with a syndesmotic injury and isolated syndesmotic injury) [35, 36]. Included studies are summarized in Table 2.
The three most frequently used measurement methods to assess the distal tibio-fibular syndesmosis using plain radiographs. a Measurement of the tibio-fibular clear space (TFCS). b 65-year old patient with a chronic syndesmotic instability following a malleolar fracture. c Measurement of the TFCS. d Measurement of the tibio-fibular overlap (TFO). e 29-year old patient with an acute syndesmotic injury following a high fibular and posterior malleolar fracture. The syndesmotic injury was not addressed on the primary surgery. f Measurement of the TFO. g Measurement of the medial clear space (MCS). h 55-year old patient with an acute syndesmotic injury and injury of the deltoid ligament following a malleolar fracture. i Measurement of the MCS
Investigators assessing the use of CT scans most common assessed the tibio-fibular width on axial images (anterior, middle, and posterior); however, only one study investigated sensitivity and specificity for syndesmotic injury using this technique in patients with ankle fractures [50]. Sensitivity/ specificity of 56.5%/ 91.7% was evident for the anterior (cut-off 4.0 mm), 74.4%/ 75.0% (cut-off 4.0 mm) for the middle, and 74.4%/ 78.8% for the maximum (cut-off 5.7 mm) tibio-fibular width [50]. The posterior tibio-fibular width was not a reliable predictor (Table 3 and Fig. 4) [50].
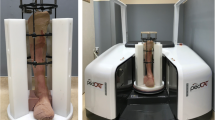
Frequently used measurement methods to assess the distal tibio-fibular syndesmosis using computed tomography (CT) scans. Measurements were performed 1 cm above the distal tibial plafond. a Measurement of the tibio-fibular width anterior (A), middle (C) and posterior (B). b 35-year old patient with an acute syndesmotic instability following a high fibular and posterior malleolar fracture. The syndesmotic injury was not addressed on the primary surgery. c Measurement of the tibio-fibular width. d Measurement of the antero-posterior translation (D, E, F) and the rotation (angle A1) of the distal fibula. e 47-year old patient with an acute syndesmotic injury following a high fibular fracture and small posterior malleolar avulsion. f Measurement of the antero-posterior translation and rotation of the distal fibula. g Measurement of the tibio-fibular clear space (TFCS) and tibio-fibular overlap (TFO). h 37-year old patient with an acute syndesmotic injury following a high fibular fracture. i Measurement of the TFCS and TFO. Radiologists and orthopedic surgeons should be aware that a distal fracture of the fibula and/or an additional tibia fracture influence the measurements. It is important to mention that the rotation of the ankle also influences the measurements
Most of the MRI studies used direct assessment of syndesmotic integrity. Only three studies (from the same author) used indirect assessment techniques [62,62,64]. Of the studies that assessed the syndesmosis directly, two studies included a mixed cohort (ankle fracture in combination with a syndesmotic injury and isolated syndesmotic injury), while three studies included patients with isolated syndesmotic injuries [35, 36, 65,65,67]. One study included patients with an ankle fracture in combination with a syndesmotic injury [68]. Ankle arthroscopy was used as a reference standard in all studies. Two studies used contrast media for MRI. Better sensitivity and specificity were reported when using a 3-Tesla (T) rather than a 1.5 T MRI (Table 4) [65, 67].
Methodological quality
Low probability of bias regarding patient selection, index test, reference standard, and flow and timing was found in 37.5% of the included studies [28, 33, 34, 55, 65]. Lack of clarity regarding flow and timing was found in 50.0% [29, 35, 36, 66,66,68]. Most of these studies used MRI for assessment of the syndesmosis. In 12.5% of the studies, lack of clarity regarding the index test was present (e.g. not specified if the investigator had knowledge of the reference standard while assessing the index test) [43, 58]. No relevant bias was found regarding the reference standard or patient selection. Ankle arthroscopy or MRI (the latter in group 1 and 2) was most commonly used as the reference standard. Studies were overall applicable to daily practice. One study did not clearly provide information about patient characteristics; therefore, the selection was unclear [55]. Another study did not provide sufficient information about the MRI used for assessment of the index test [68]. The methodological quality is summarized in Fig. 5.
Evaluation of the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) tool to assess studies using conventional radiographs, computed tomography (CT) scans and magnet resonance imaging (MRI) for assessment of syndesmotic instability. a Proportion of studies with low, high or unclear risk of bias. b Proportion of studies with low, high, or unclear concerns regarding applicability
Discussion
Several different measurement techniques are described in the literature assessing the distal tibiofibular syndesmosis [37, 38, 40, 41, 42, 45, 48, 69]. Chaput first described the TFCS (“la ligne clair”) in 1908 [70]. Pettrone et al. introduced a measurement algorithm for assessment of the distal tibiofibular interval in 1983 [69]. In 1989, Harper et al. defined radiographic criteria for physiologic syndesmotic dimensioning on AP and mortise radiographs [38]. TFCS should be less than 6 mm in both the AP and mortise view [38]. Overlap of the fibula and anterior tibial tubercle should be greater than 42% of the width of the fibula on the AP view [38].
Evaluation starts with conventional radiographs, including weight-bearing lateral, AP, and mortise views of the ankle joint. Several studies have shown that radiographic measurements of the distal tibio-fibular alignment have limited use and are not always predictive of injury severity [27,28,29, 49]. In these cases, intraoperative stress radiography may help assess the distal tibiofibular syndesmosis [39, 71, 72]. Widening of the TFCL and the MCL by more than 2 mm during external rotation stress indicates injury of the syndesmosis [39]; however, the evidence for stress views as the principal assessment for syndesmotic injuries is weak, especially in the case of chronic injuries.
The diagnostic accuracy of conventional radiographs differs considerably between authors [28, 33,34,35,36]; however, accuracy also differs between isolated syndesmotic injuries (e.g. high ankle sprains) and additional ankle fractures [33, 34]. Considering the Weber and/or Orthopedic Trauma Association (OTA) classification in combination with assessment of the TFCS, TFO medial clear space (MCS), and superior clear space (SCS) achieved a sensitivity of 47% and a specificity of 100% [33]. The sensitivity can be increased to 92.0% if the Lauge-Hansen classification is used instead of the Weber or OTA classification [33]. Of note, Nielson et al. found better sensitivity for TFO (assessment using AP radiographs) than TFCS or MCS when predicting syndesmotic injury in presence of an ankle fracture, but specificity was low [29]. Interestingly, X-ray findings did not correlate with anterior or posterior tibiofibular injury detected by MRI. The authors concluded that traditional radiographic measurements should not solely be relied on for determining if the syndesmosis is intact (Fig. 6). Acute isolated syndesmotic injuries have a sensitivity of 82.0% and a specificity of 75.0% when using the TFCS for assessment (AP view) [34]. A higher sensitivity was found for TFCS than either TFO or MCL [34]. The cut-off value in this study has been shown to be 5.3 mm for TFCS, 2.8 mm for TFO, and 2.8 mm for MCS [34]. AP views were used in this study for assessment of TFCS, while TFO and MCS were evaluated on the mortise view. It is important to mention that there is a wide variance regarding the normal tibio-fibular interval in the literature. In addition, most measurement methods are highly dependent on how severely the ankle joint was mal-rotated when the X-ray was taken [27, 73]. Significant differences were also found between male and female patients; therefore, published cut-off values must be interpreted with care [44].
Example of a 37-year-old man with an acute isolated syndesmotic injury. The conventional radiographs (mortise view) cannot predict reliably the syndesmotic injury. a Normal tibio-fibular clear space (TFCS). b Normal tibio-fibular overlap (TFO). c Normal medial clear space (MCS). d Axial magnet resonance imaging (MRI) proton density with fat saturation demonstrates full thickness tear of both the anterior (white arrow) and posterior (gray arrow) tibio-fibular ligaments. e Coronal T2 fat saturated MRI image shows heterogeneity and increased signal of the syndesmotic ligaments (arrow), consistent with syndesmotic injury
CT scans have been investigated extensively in the recent years. Axial images 1 cm above the tibial plafond are frequently used to assess rotation of the distal fibula and tibio-fibular width [43, 47, 50, 52,52,53,54,55,56,57,58,59,61]. The tibio-fibular width measured at the level of maximal distance has a sensitivity of 74.4% and a specificity of 79.8% to detect acute syndesmotic injuries (study including patients with ankle fracture) [50]. The cut-off value was found to be 5.7 mm [50]. Recently, Nault et al. introduced a novel algorithm for syndesmotic assessment which considers mal-rotation, lateral displacement, and antero-posterior displacement of the distal fibula [56]. This algorithm was additionally used for assessment of the distal syndesmosis on MRIs [62,62,64].
CT scans possess several advantages over conventional X-rays—first, no osseous overlaps are present, making the assessment more precise [46]; second, the tibiofibular joint can be visualized directly, which positively influences the accuracy [31]; third, the shape of the incisura fibularis and mal-rotation of the distal fibula can be assessed [51, 54, 74, 75]. As with conventional radiographs, the average measurements between male and female are significantly different [54]; however, bilateral CT scans of healthy ankles did not vary by more than 2.3 mm in tibiofibular interval and 6.5° in fibular rotation [54]. Recently, weight-bearing CT scans have gained in popularity with patients who have foot and ankle disorders; however, to our knowledge, no study has been published assessing this imaging technique to investigate syndesmotic instability.
High diagnostic accuracy is best achieved by utilizing MRI over conventional radiographs or CT scans, especially in chronic syndesmotic instability [35, 36, 66,66,68]; furthermore, contrast media and/or a 3 T MRI improve diagnostic accuracy of MRI [65, 67]. While direct assessment of the tibiofibular syndesmosis is possible by MRI, assessment of syndesmotic injury by X-ray or CT scans must rely on recognition of secondary signs. Sensitivity of up to 91.0% and specificity of 100% have been reported for syndesmotic injuries. Sensitivity of 84.0% and specificity of 93.5% have been reported for additional deltoid ligament tears using MRI [65]. Despite its high sensitivity and specificity, MRI has some notable disadvantages when compared to conventional X-rays or CT scans—first, MRI is both costly and not always readily available; second, interpretation errors may lead to over- or underestimation of the syndesmotic injury; third, MRI cannot be performed under weight-bearing condition. A reliable diagnostic protocol under weight-bearing condition would be desirable, especially for assessment of subtle chronic syndesmotic injuries. It is important to mention that ankle arthroscopy is likely the best definitive tool for assessing the degree of syndesmotic instability and mortise widening with up to 100% accuracy [36, 76].
Overall, the methodological quality of the included studies was satisfactory. Many studies using MRI failed to note how long had passed between when the MRI was obtained and when the surgery was performed. Too much time between the index test and the reference standard could cause bias. The included studies were generally applicable to daily practice.
In conclusion, conventional radiographs cannot predict syndesmotic injuries reliably. CT outperforms conventional X-rays in detecting syndesmotic mal-reduction. Additionally, the syndesmotic interval can be assessed in greater detail by CT. Using MRI, sensitivity and specificity of nearly 100% can be achieved. However, correlating MRI findings with patients’ complaints can be difficult, and utility with subtle syndesmotic instability needs further investigation. The methodological quality of the included studies is satisfactory.
References
van den Bekerom MP. Diagnosing syndesmotic instability in ankle fractures. World J Orthop. 2011;2(7):51–6.
Sman AD, Hiller CE, Rae K, Linklater J, Black DA, Nicholson LL, et al. Diagnostic accuracy of clinical tests for ankle syndesmosis injury. Br J Sports Med. 2015;49(5):323–9.
Hopkinson WJ, St Pierre P, Ryan JB, Wheeler JH. Syndesmosis sprains of the ankle. Foot Ankle. 1990;10(6):325–30.
Ryan PM, Rodriguez RM. Outcomes and return to activity after operative repair of chronic latent syndesmotic instability. Foot Ankle Int. 2016;37(2):192–7.
Rammelt S, Obruba P. An update on the evaluation and treatment of syndesmotic injuries. Eur J Trauma Emerg Surg. 2015;41(6):601–14.
Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653–60.
Zalavras C, Thordarson D. Ankle syndesmotic injury. J Am Acad Orthop Surg. 2007;15(6):330–9.
Miyamoto W, Takao M. Management of chronic disruption of the distal tibiofibular syndesmosis. World J Orthop. 2011;2(1):1–6.
van Dijk CN, Longo UG, Loppini M, Florio P, Maltese L, Ciuffreda M, et al. Classification and diagnosis of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1200–16.
Clanton TO, Williams BT, Backus JD, Dornan GJ, Liechti DJ, Whitlow SR, et al. Biomechanical analysis of the individual ligament contributions to syndesmotic stability. Foot Ankle Int. 2017;38(1):66–75.
Schuberth JM, Jennings MM, Lau AC. Arthroscopy-assisted repair of latent syndesmotic instability of the ankle. Arthroscopy. 2008;24(8):868–74.
Kim JH, Gwak HC, Lee CR, Choo HJ, Kim JG, Kim DY. A comparison of screw fixation and suture-button fixation in a syndesmosis injury in an ankle fracture. J Foot Ankle Surg. 2016;55(5):985–90.
Hunt KJ, Goeb Y, Behn AW, Criswell B, Chou L. Ankle joint contact loads and displacement with progressive syndesmotic injury. Foot Ankle Int. 2015;36(9):1095–103.
Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am. 1976;58(3):356–7.
Bartonicek J. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat. 2003;25(5–6):379–86.
Sora MC, Strobl B, Staykov D, Forster-Streffleur S. Evaluation of the ankle syndesmosis: a plastination slices study. Clin Anat. 2004;17(6):513–7.
Ebraheim NA, Taser F, Shafiq Q, Yeasting RA. Anatomical evaluation and clinical importance of the tibiofibular syndesmosis ligaments. Surg Radiol Anat. 2006;28(2):142–9.
Magan A, Golano P, Maffulli N, Khanduja V. Evaluation and management of injuries of the tibiofibular syndesmosis. Br Med Bull. 2014;111(1):101–15.
Lilyquist M, Shaw A, Latz K, Bogener J, Wentz B. Cadaveric analysis of the distal tibiofibular syndesmosis. Foot Ankle Int. 2016;37(8):882–90.
Hermans JJ, Beumer A, de Jong TA, Kleinrensink GJ. Anatomy of the distal tibiofibular syndesmosis in adults: a pictorial essay with a multimodality approach. J Anat. 2010;217(6):633–45.
Williams BT, Ahrberg AB, Goldsmith MT, Campbell KJ, Shirley L, Wijdicks CA, et al. Ankle syndesmosis: a qualitative and quantitative anatomic analysis. Am J Sports Med. 2015;43(1):88–97.
Mengiardi B, Pfirrmann CW, Vienne P, Hodler J, Zanetti M. Medial collateral ligament complex of the ankle: MR appearance in asymptomatic subjects. Radiology. 2007;242(3):817–24.
Boss AP, Hintermann B. Anatomical study of the medial ankle ligament complex. Foot Ankle Int. 2002;23(6):547–53.
Knupp M, Lang TH, Zwicky L, Lotscher P, Hintermann B. Chronic ankle instability (medial and lateral). Clin Sports Med. 2015;34(4):679–88.
Hintermann B, Golano P. The anatomy and function of the deltoid ligament. Tech Foot Ankle. 2014;13:67–72.
Milner CE, Soames RW. The medial collateral ligaments of the human ankle joint: anatomical variations. Foot Ankle Int. 1998;19(5):289–92.
Beumer A, van Hemert WL, Niesing R, Entius CA, Ginai AZ, Mulder PG, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004;423:227–34.
Takao M, Ochi M, Naito K, Iwata A, Kawasaki K, Tobita M, et al. Arthroscopic diagnosis of tibiofibular syndesmosis disruption. Arthroscopy. 2001;17(8):836–43.
Nielson JH, Gardner MJ, Peterson MG, Sallis JG, Potter HG, Helfet DL, et al. Radiographic measurements do not predict syndesmotic injury in ankle fractures: an MRI study. Clin Orthop Relat Res. 2005;436:216–21.
Jeong MS, Choi YS, Kim YJ, Kim JS, Young KW, Jung YY. Deltoid ligament in acute ankle injury: MR imaging analysis. Skelet Radiol. 2014;43(5):655–63.
Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int. 2006;27(10):788–92.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36.
Hermans JJ, Wentink N, Beumer A, Hop WC, Heijboer MP, Moonen AF, et al. Correlation between radiological assessment of acute ankle fractures and syndesmotic injury on MRI. Skelet Radiol. 2012;41(7):787–801.
Schoennagel BP, Karul M, Avanesov M, Bannas P, Gold G, Grossterlinden LG, et al. Isolated syndesmotic injury in acute ankle trauma: comparison of plain film radiography with 3T MRI. Eur J Radiol. 2014;83(10):1856–61.
Oae K, Takao M, Naito K, Uchio Y, Kono T, Ishida J, et al. Injury of the tibiofibular syndesmosis: value of MR imaging for diagnosis. Radiology. 2003;227(1):155–61.
Takao M, Ochi M, Oae K, Naito K, Uchio Y. Diagnosis of a tear of the tibiofibular syndesmosis: the role of arthroscopy of the ankle. J Bone Joint Surg. 2003;85(3):324–9.
Leeds HC, Ehrlich MG. Instability of the distal tibiofibular syndesmosis after bimalleolar and trimalleolar ankle fractures. J Bone Joint Surg Am. 1984;66(4):490–503.
Harper MC, Keller TS. A radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle. 1989;10(3):156–60.
Xenos JS, Hopkinson WJ, Mulligan ME, Olson EJ, Popovic NA. The tibiofibular syndesmosis: evaluation of the ligamentous structures, methods of fixation, and radiographic assessment. J Bone Joint Surg Am. 1995;77(6):847–56.
Brage ME, Bennett CR, Whitehurst JB, Getty PJ, Toledano A. Observer reliability in ankle radiographic measurements. Foot Ankle Int. 1997;18(6):324–9.
Grass R, Rammelt S, Biewener A, Zwipp H. Peroneus longus ligamentoplasty for chronic instability of the distal tibiofibular syndesmosis. Foot Ankle Int. 2003;24(5):392–7.
DeAngelis JP, Anderson R, DeAngelis NA. Understanding the superior clear space in the adult ankle. Foot Ankle Int. 2007;28(4):490–3.
Marmor M, Hansen E, Han HK, Buckley J, Matityahu A. Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot Ankle Int. 2011;32(6):616–22.
Shah AS, Kadakia AR, Tan GJ, Karadsheh MS, Wolter TD, Sabb B. Radiographic evaluation of the normal distal tibiofibular syndesmosis. Foot Ankle Int. 2012;33(10):870–6.
Grenier S, Benoit B, Rouleau DM, Leduc S, Laflamme GY, Liew A. APTF: anteroposterior tibiofibular ratio, a new reliable measure to assess syndesmotic reduction. J Orthop Trauma. 2013;27(4):207–11.
Choi Y, Kwon SS, Chung CY, Park MS, Lee SY, Lee KM. Preoperative radiographic and CT findings predicting syndesmotic injuries in supination-external rotation-type ankle fractures. J Bone Joint Surg Am. 2014;96(14):1161–7.
Chen Y, Qiang M, Zhang K, Li H, Dai H. A reliable radiographic measurement for evaluation of normal distal tibiofibular syndesmosis: a multi-detector computed tomography study in adults. J Foot Ankle Res. 2015;8:32.
Peterson KS, Chapman WD, Hyer CF, Berlet GC. Maintenance of reduction with suture button fixation devices for ankle syndesmosis repair. Foot Ankle Int. 2015;36(6):679–84.
Feller R, Borenstein T, Fantry AJ, Kellum RB, Machan JT, Nickisch F, et al. Arthroscopic quantification of syndesmotic instability in a cadaveric model. Arthroscopy. 2017;33(2):436–44.
Yeung TW, Chan CY, Chan WC, Yeung YN, Yuen MK. Can pre-operative axial CT imaging predict syndesmosis instability in patients sustaining ankle fractures? Seven years’ experience in a tertiary trauma center. Skelet Radiol. 2015;44(6):823–9.
Tang CW, Roidis N, Vaishnav S, Patel A, Thordarson DB. Position of the distal fibular fragment in pronation and supination ankle fractures: a CT evaluation. Foot Ankle Int. 2003;24(7):561–6.
Elgafy H, Semaan HB, Blessinger B, Wassef A, Ebraheim NA. Computed tomography of normal distal tibiofibular syndesmosis. Skelet Radiol. 2010;39(6):559–64.
Mukhopadhyay S, Metcalfe A, Guha AR, Mohanty K, Hemmadi S, Lyons K, et al. Malreduction of syndesmosis: are we considering the anatomical variation? Injury. 2011;42(10):1073–6.
Dikos GD, Heisler J, Choplin RH, Weber TG. Normal tibiofibular relationships at the syndesmosis on axial CT imaging. J Orthop Trauma. 2012;26(7):433–8.
Knops SP, Kohn MA, Hansen EN, Matityahu A, Marmor M. Rotational malreduction of the syndesmosis: reliability and accuracy of computed tomography measurement methods. Foot Ankle Int. 2013;34(10):1403–10.
Nault ML, Hebert-Davies J, Laflamme GY, Leduc S. CT scan assessment of the syndesmosis: a new reproducible method. J Orthop Trauma. 2013;27(11):638–41.
Lepojarvi S, Pakarinen H, Savola O, Haapea M, Sequeiros RB, Niinimaki J. Posterior translation of the fibula may indicate malreduction: CT study of normal variation in uninjured ankles. J Orthop Trauma. 2014;28(4):205–9.
Malhotra G, Cameron J, Toolan BC. Diagnosing chronic diastasis of the syndesmosis: a novel measurement using computed tomography. Foot Ankle Int. 2014;35(5):483–8.
Mendelsohn ES, Hoshino CM, Harris TG, Zinar DM. CT characterizing the anatomy of uninjured ankle syndesmosis. Orthopedics. 2014;37(2):e157–60.
Kotwal R, Rath N, Paringe V, Hemmadi S, Thomas R, Lyons K. Targeted computerised tomography scanning of the ankle syndesmosis with low dose radiation exposure. Skelet Radiol. 2016;45(3):333–8.
Kocadal O, Yucel M, Pepe M, Aksahin E, Aktekin CN. Evaluation of reduction accuracy of suture-button and screw fixation techniques for syndesmotic injuries. Foot Ankle Int. 2016;37(12):1317–25.
Nault ML, Gascon L, Hebert-Davies J, Leduc S, Laflamme GY, Kramer D. Modification of distal tibiofibular relationship after a mild syndesmotic injury. Foot Ankle Spec. 2017a;10(2):133–8.
Nault ML, Hebert-Davies J, Yen YM, Shore B, Jarrett DY, Kramer DE. Variation of syndesmosis anatomy with growth. J Pediatr Orthop. 2016;36(4):e41–4.
Nault ML, Marien M, Hebert-Davies J, Laflamme GY, Pelsser V, Rouleau DM, et al. MRI quantification of the impact of ankle position on syndesmosis anatomy. Foot Ankle Int. 2017b;38(2):215–9.
Chun KY, Choi YS, Lee SH, Kim JS, Young KW, Jeong MS, et al. Deltoid ligament and tibiofibular syndesmosis injury in chronic lateral ankle instability: magnetic resonance imaging evaluation at 3T and comparison with arthroscopy. Korean J Radiol. 2015;16(5):1096–103.
Han SH, Lee JW, Kim S, Suh JS, Choi YR. Chronic tibiofibular syndesmosis injury: the diagnostic efficiency of magnetic resonance imaging and comparative analysis of operative treatment. Foot Ankle Int. 2007;28(3):336–42.
Kim S, Huh YM, Song HT, Lee SA, Lee JW, Lee JE, et al. Chronic tibiofibular syndesmosis injury of ankle: evaluation with contrast-enhanced fat-suppressed 3D fast spoiled gradient-recalled acquisition in the steady state MR imaging. Radiology. 2007;242(1):225–35.
Warner SJ, Garner MR, Schottel PC, Hinds RM, Loftus ML, Lorich DG. Analysis of PITFL injuries in rotationally unstable ankle fractures. Foot Ankle Int. 2015;36(4):377–82.
Pettrone FA, Gail M, Pee D, Fitzpatrick T, Van Herpe LB. Quantitative criteria for prediction of the results after displaced fracture of the ankle. J Bone Joint Surg Am. 1983;65(5):667–77.
Chaput V. Les fractures malleolaires du cou-de-pieds et les accidents du travaill. Paris: Masson & Cie; 1907.
Pakarinen H, Flinkkila T, Ohtonen P, Hyvonen P, Lakovaara M, Leppilahti J, et al. Intraoperative assessment of the stability of the distal tibiofibular joint in supination-external rotation injuries of the ankle: sensitivity, specificity, and reliability of two clinical tests. J Bone Joint Surg Am. 2011;93(22):2057–61.
Stoffel K, Wysocki D, Baddour E, Nicholls R, Yates P. Comparison of two intraoperative assessment methods for injuries to the ankle syndesmosis: cadaveric study. J Bone Joint Surg Am. 2009;91(11):2646–52.
Pneumaticos SG, Noble PC, Chatziioannou SN, Trevino SG. The effects of rotation on radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle Int. 2002;23(2):107–11.
Cherney SM, Spraggs-Hughes AG, McAndrew CM, Ricci WM, Gardner MJ. Incisura morphology as a risk factor for syndesmotic malreduction. Foot Ankle Int. 2016;37(7):748–54.
Vasarhelyi A, Lubitz J, Gierer P, Gradl G, Rosler K, Hopfenmuller W, et al. Detection of fibular torsional deformities after surgery for ankle fractures with a novel CT method. Foot Ankle Int. 2006;27(12):1115–21.
Lucas DE, Watson BC, Simpson GA, Berlet GC, Hyer CF. Arthroscopic evaluation of syndesmotic instability and malreduction. Foot Ankle Spec. 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Nicola Krahenbuhl is supported by a grant from the Swiss National Science Foundation (SNF; grant number P2BSP3_174979).
Additional information
Investigation performed at the Department of Orthopaedics and Department of Radiology and Imaging Sciences, University of Utah, Salt Lake City, Utah, USA
Rights and permissions
About this article
Cite this article
Krähenbühl, N., Weinberg, M.W., Davidson, N.P. et al. Imaging in syndesmotic injury: a systematic literature review. Skeletal Radiol 47, 631–648 (2018). https://doi.org/10.1007/s00256-017-2823-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-017-2823-2