Abstract
Objective
Slipped capital femoral epiphysis (SCFE) is a hip disorder where the femoral head slips relative to the neck at the physis. Appropriate treatment of SCFE depends on the severity of the slip, commonly categorised using the Southwick (SW) angle. The SW angle is measured in the frog-lateral leg position, which can be painful and potentially unattainable for patients. The purpose of this study is to determine how errors in frog-lateral radiograph positioning affect measured SW angles and slip classifications.
Methods
Models of SCFE hips were produced from one CT scan of a normal hip; 360 deformities were created. SW angles were measured from a simulated frog-lateral position. Femoral lateral head-neck angles (LHNA; equivalent to SW in incorrect frog-lateral plane) were measured over a range of 837 incorrect frog-lateral leg positions with positioning errors in flexion and/or internal/external rotation.
Results
Seventy-six per cent of all imaging position-deformity combinations had error in the reported angle (>1° difference between LHNA and SW). Of those, 70% had <5°, 24% had 5° to 10°, and 6% had >10° of error from the actual SW angle. Three per cent of LHNAs that had >10° error resulted from <10° of positioning error.
Conclusions
If the patient is limited in flexion or external rotation, more diagnostic testing should be considered if error in the reported slip measurement would affect treatment decisions or if accurate severity classification is needed for research. Small positioning errors in moderate and severe slips can cause a > 10° LHNA error; additional three-dimensional imaging should be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Slipped capital femoral epiphysis (SCFE) is a disorder of the adolescent hip where the femoral head slips relative to the femoral neck at the physis (growth plate) [1]. SCFE has an incidence of about 1 case per 10,000 children [2]. Although the aetiology of SCFE remains unclear, it is associated with obesity [3, 4]. SCFE can result in premature hip osteoarthritis (OA), pain associated with loss of flexion and internal rotation [5], and disability [6].
Treatment for SCFE is controversial and may depend on the severity of the slip, the stability of the slip, and whether the condition is acute or chronic. In particular, knowing the severity of a slip may be important for selecting surgical treatment, in addition to classifying slips for registry-based studies. The severity of the slip is often determined using the Southwick (SW) angle, measured as the angle between the neck and head axes on a frog-leg lateral radiograph, which is determined by subtracting the angle between the head axis and the femoral shaft axis in the unaffected side from the affected side [7]. The frog-lateral position can be quite painful for SCFE patients, especially those with an unstable slip. SCFE patients may not be able to achieve the frog-lateral position because of a limited range of motion believed to be caused by impingement of the slipped femur. It is not uncommon for severe slips to limit flexion and exhibit forced external rotation [8]; one particular case study described a patient with severe SCFE who displayed a forced external rotation of 45° and was limited to 60° of flexion [5]. There is also a potential to worsen acute slips by forcing the leg into the proper frog-lateral position [9]. If a patient is unable to achieve the frog-lateral position, the hip is generally imaged in the closest achievable position.
It is not clear how positioning errors in the frog-leg radiograph impact the SW measurement. The purpose of this study is to determine how errors in frog-lateral radiograph positioning affect measured SW angles and slip classifications (mild, moderate or severe) based on those angles.
Materials and methods
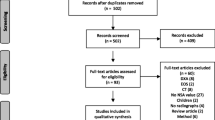
Ethics board approval was obtained from our institution for this study.
Models of hips with SCFE were developed by first creating a model of a normal adolescent hip and then simulating slips in two planes. We used one computed tomographic (CT) scan of a normal right hip (16 years old, female, resolution 0.6 × 0.6 × 0.4 mm3) obtained from clinical records. The geometry of the femur and epiphysis was obtained by segmenting the scans semi-automatically using image analysis software (Mimics, Leuven, Belgium). Models of hips with SCFE were then created by combining simulated posterior and inferior slips of the femoral head relative to the physis in the axial and coronal planes respectively. We simulated axial and coronal slips from 0° (no deformity) to 90° in 5° steps (19 increments per plane), which, when combined, yielded 360 simulated deformed hips and one normal hip (192 = 361 total models) [10].
We measured Southwick (SW) angles (femoral head-neck angle measured in the correct frog-leg lateral position) for each of the 360 simulated deformed and one normal hip. For each simulated deformed hip, we generated a simulated frog-leg lateral radiograph using a planar projection of the model. We positioned each simulated 3D hip in a clinically relevant simulated frog-leg lateral position (lateral flexion of 54°and external rotation of 42°, as determined by three experienced paediatric orthopaedic surgeons [10]). The SW angle of each deformed hip was then measured automatically in this position from the simulated radiograph of the 3D computer model (Fig. 1). The 361 simulated deformed hips were divided into normal (<1°), mild (1°-30°), moderate (30-60°), and severe (≥60°) groups based on the SW angles.
We then assessed the effect of positioning error on femoral lateral head-neck angles by generating simulated radiographs for all the simulated deformed hips for a range of simulated incorrect positions. We deliberately refer to these measurements as “lateral head-neck angles (LHNAs)” rather than “Southwick angles” because of the incorrect positioning involved, but the measurement method remains the same in the non-ideal planes. We measured femoral LHNAs for 837 different incorrect imaging planes that simulated incorrect positions. Incorrect imaging planes simulated lateral flexion angles ranging from 24° to 68° and external rotation angles ranging from 12° to 56° for a relative range in positioning error of −30° to 14° in each of flexion and external rotation (Fig. 2). To obtain the range of positioning errors, we assumed that error in flexion or external rotation of 30° or more would be obvious, resulting in no measurement being made, and that patients with SCFE would be unlikely to over-flex by more than ~15°. We also used the normal physiological limit of external rotation (51°, SD ~5°), which gives an approximate upper bound on external rotation of 56° for adolescents [11].
Femur models in incorrect viewing planes overlaid on femur in SW viewing plane to show differences in measured lateral head-neck angle (LHNA). a SW flexion and external rotation (ideal position); b abnormal position, under-flexed by 41°, over externally rotated by 14° giving an error in the reported angle of −11.2°; c abnormal position, over-flexed by 14°, under externally rotated by 30° giving an error in the reported angle of 11°
Measurement of the femoral LHNAs for the 837 incorrect imaging planes was repeated for each of the 361 simulated deformed hips. An error in the reported angle is defined as a greater than 1° difference between the LHNA and SW angle, which is similar to the inter- and intra-rater reliability of SW angle measurements [12]. Each LHNA was also categorised as mild, moderate, or severe based on the same ranges used for the SW angle (above), and the resulting category was compared to that from the SW angle measurement for a particular deformity to determine whether the error in positioning resulted in an error in classification.
All simulations, shape fitting and analyses were performed using MATLAB (MathWorks, MA, USA). Summary statistics were calculated to characterise LHNAs over all imaging positions.
Results
Among all the simulated “incorrect” positions for all deformed hips, about 6% of all LHNAs (every deformity-position combination) were misclassified in severity when compared to actual SW angle severity (Table 1). LHNAs were more likely to be classified in a lower severity category than the SW angle (6% of mild LHNAs were actually moderate SW; 8% of moderate LHNAs were actually severe SW) than higher (3% of moderate LHNAs were actually mild SW; 4% of severe LHNAs were actually moderate SW). No mild LHNA deformities were actually classified as severe SW deformities and no severe LHNA deformities were actually classified as mild SW deformities. No LHNAs or SW angles were classified as normal (<1° slip) in the deformed hips.
Seventy-six per cent (76%) of the simulated “incorrect” position/deformity combinations had error in the reported angle (difference between LHNA and SW) of greater than 1°; 70% of those that had error in the reported angle had less than 5° error, 24% had 5° to 10° error, and 6% had more than 10° of error. In a small proportion of cases, small errors in positioning led to large errors in LHNA; 3% of LHNAs that had more than 10° of reported error from the actual SW angle had less than 10° of error in flexion and external rotation. Severity was more likely to be underestimated (59% of errors in the reported angle underestimated severity) than overestimated (41% of errors in the reported angle overestimated severity) (Table 2). Most deformities with more than 10° error were moderate or severe (Fig. 3c–f).
Error in the reported angle with respect to errors in flexion (x-axis) and external rotation (y-axis). Dashed lines along the line of no flexion error (vertical) and the line of no external rotation error (horizontal). The origin of the plot is at 12° of external rotation and 24° of flexion. Points represent deformities where the LHNA was between 5° and 10° and more than 10° from the true SW. (a) Mild LHNAs that underestimated severity. (b) Mild LHNAs that overestimated severity. (c) Moderate LHNAs that underestimated severity. (d) Moderate LHNAs that overestimated severity. (e) Severe LHNAs that underestimated severity. (f) Severe LHNAs that overestimated severity
The direction of change seen in errors in the reported angle and misclassifications was clearly influenced by the type of malpositioning. For LHNAs that underestimated actual severity, hips were less flexed than ideal for a frog-leg lateral radiograph (Fig. 3, Table 3). For LHNAs that overestimated actual severity, hips were less externally rotated than ideal for a frog-leg lateral radiograph (Fig. 3, Table 3). For LHNAs that underestimated actual severity by more than 10°, hips were much less flexed and more externally rotated than ideal. For LHNAs that overestimated actual severity by more than 10°, hips were much less externally rotated and more flexed than ideal (Table 3).
Discussion
Using a 3D geometric bone model to predict the effects of improper frog-lateral leg positioning on Southwick angle measurements, we found that incorrect frog-lateral leg positioning resulted in about 22.6% of all tests having errors above 5° and approximately 6% of all LHNAs being misclassified. Our findings are consistent with results from a cadaveric model that was produced to quantify error in the femoral neck-shaft angle (NSA) taken in the anteroposterior view, where it was found that the NSA was susceptible to femur rotation [13]. That study’s finding that unwanted external rotation caused overestimated NSA is consistent with our finding that hips imaged in insufficient external rotation result in overestimated LHNAs, since both of these rotations caused the femur to be less oblique to the plane of imaging. The cadaveric study’s finding that most errors in measurement were less than or equal to 10° for a wide range of femoral positioning is consistent with our finding that 94% of LHNA measurements were within 10° of the correct SW angle and suggest the SW angle is a robust method for measuring SCFE slips.
Our result that errors in the reported angle caused some deformities to be placed in the wrong severity group suggests that correct frog-lateral leg positioning is important for proper SW angle classification. With a trend towards registry-based studies, it is important to correctly classify the severity of a slip.
We found that severe slips generally had over 10° of error in the reported LHNA in many of the incorrect imaging positions. While treatment approaches vary greatly for SCFE, for those surgeons who place a large weight on the degree of deformity in treatment decisions, this study highlights the need for 3D imaging to avoid inaccuracy in severity assessment.
We found that slips are more likely to be underestimated than overestimated if imaged in an incorrect frog-lateral position. If the slip angle is underestimated, the surgeon may only become aware of the severity of the deformity intra-operatively, meaning a shorter screw length is required, which may be more biomechanically unstable.
Our finding that LHNAs that underestimated severity had high positioning error in flexion and LHNAs that overestimated severity had high positioning error in external rotation suggests that not achieving a high enough flexion angle in the frog-leg imaging position could cause a slip to be measured as less severe than it is, and not achieving a high enough external rotation angle in the frog-leg imaging position could cause a slip to be measured as worse than it is. Underestimations of more than 10° had a mean flexion error of −20°, and overestimations of more than 10° had a mean external rotation error of −16°. While a clinician would likely recognise such a large error in position, a smaller positioning error (within 10° of the actual position) may go unnoticed and can still cause more than 10° of error in the reported slip angle (3% of >10° errors in the reported angle were within 10° of the actual position).
One strength of this work is that one normal bone model was used to create clinically relevant SCFE deformities, which allows direct comparisons of the degree of deformity without intersubject variability in other factors. A second strength is that femoral head-neck angles were calculated using an automated computerised method, eliminating reader variability. A further strength of this work is that it was a computer simulation study, which avoids subjecting patients to excessive radiation and pain.
Limitations of this work include that our correct frog-lateral plane is an estimation. However, there is no consensus on what exactly a frog-lateral plane is (specific flexion and external rotation angles). We did, however, obtain plane determinations from three surgeons and found high inter- and intra-rater ICC values [10]. The hip model we used was of a 16 year old, which is older than the typical SCFE age range. However, SW and LHNA measurements were made based on the simulated SCFE slip angles, so the actual bony geometry of the femur is only used to define the neck and epiphyseal axes. Another limitation of this work is that we had limited evidence from which to estimate our range of simulated positioning errors. There is a lack of research on the typical magnitude of positioning error, whether errors in external rotation or flexion are more common in SCFE patients, and how often SCFE patients are imaged in non-ideal planes. However, given that SCFE results in pain and reduced ROM, our clinical experience suggests the number of affected patients may be underestimated.
Accurate frog-leg lateral positioning is important for correctly measuring the SW angle of SCFE deformities and for placing them in the proper severity group for research purposes. Incorrect slip measurement is a concern because patient care decisions may be dependent on the severity of a slip. While the frog-leg radiograph remains an important diagnostic tool in SCFE, if it is suspected that the patient may be limited in flexion or external rotation, additional diagnostic testing should be considered if an erroneous measurement would affect treatment decisions. Adopting a lower threshold for three-dimensional imaging of moderate and severe deformities should be considered because a small error in positioning could cause a greater than 10° error in the reported Southwick angle.
References
Wu GS, Pollock AN. Slipped capital femoral epiphysis. Pediatr Emerg Care. 2011;27(11):1095–6.
Gholve PA, Cameron DB, Millis MB. Slipped capital femoral epiphysis update. Curr Opin Pediatr. 2009;21(1):39–45.
Novais EN, Millis MB. Slipped capital femoral epiphysis: prevalence, pathogenesis, and natural history. Clin Orthop Relat Res. 2012;470(12):3432–8.
Manoff EM, Banffy MB, Winell JJ. Relationship between body mass index and slipped capital femoral epiphysis. J Pediatr Orthop. 2005;25(6):744–6.
Abraham E, Gonzalez MH, Pratap S, Amirouche F, Atluri P, Simon P. Clinical implications of anatomical wear characteristics in slipped capital femoral epiphysis and primary osteoarthritis. J Pediatr Orthop. 2007;27(7):788–95.
Sonnega RJA, van der Sluijs JA, Wainwright AM, Roposch A, Hefti F. Management of slipped capital femoral epiphysis: results of a survey of the members of the European Paediatric Orthopaedic society. J Child Orthop. Dec. 2011;5(6):433–8.
Jarrett DY, Matheney T, Kleinman PK. Imaging SCFE: diagnosis, treatment and complications. Pediatr Radiol. 2013;43(Suppl 1):S71–82.
Westhoff B, Ruhe K, Weimann-Stahlschmidt K, Zilkens C, Willers R, Krauspe R. The gait function of slipped capital femoral epiphysis in patients after growth arrest and its correlation with the clinical outcome. Int Orthop. May 2012;36(5):1031–8.
Loder RT. Controversies in slipped capital femoral epiphysis. Orthopedic Clinics of North America. 2006;37:211–221.
Jones CE, Cooper AP, Doucette J, Buchan LL, Wilson DR, Mulpuri K, d’Entremont AG. Relationships Between Severity of Deformity and Impingement in Slipped Capital Femoral Epiphysis. J Pediatr Orthop. 2015;91(5):360–4.
Rao KN, Joseph B. Value of measurement of hip movements in childhood hip disorders. J Pediatr Orthop. 2001;21(4):495–501.
Lehmann TG, Vetti N, Laborie LB, Engesæter IØ, Engesæter LB, Rosendahl K. Intra- and inter-observer repeatability of radiographic measurements for previously slipped capital femoral epiphysis at skeletal maturity. Acta Radiologica. 2014;(5):587–591.
Kay RM, Jaki KA, Skaggs DL. The effect of femoral rotation on the projected femoral neck-shaft angle. J Pediatr Orthop. 2000;20(6):736–9.
Acknowledgements
This study was supported by a Microgrant from the Rare Disease Foundation and an Undergraduate Student Research Award from Engineers in Scrubs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics board approval was obtained from our institution for this study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Jones, C.E., Cooper, A.P., Doucette, J. et al. Southwick angle measurements and SCFE slip severity classifications are affected by frog-lateral positioning. Skeletal Radiol 47, 79–84 (2018). https://doi.org/10.1007/s00256-017-2761-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-017-2761-z