Abstract
Objective
Suspected soft-tissue sarcomas are typically investigated using magnetic resonance imaging (MRI), with a view to planning image-guided core needle biopsy for confirmation of the histological diagnosis. Indeterminate superficial lesions may be small and therefore potentially difficult to biopsy safely, such lesions possibly being more amenable to primary excision biopsy. The aim of this study is to determine the suitability of this practice in the setting of a specialist sarcoma service.
Materials and methods
All patients referred over a 12-month period to the sarcoma service with a small (<3-cm), indeterminate, superficial soft-tissue mass according to MRI criteria, or a small lesion of the hand or foot deemed unsafe for percutaneous biopsy, and who underwent primary excision biopsy were included. The histology results were categorized into neoplastic and non-neoplastic lesions, and assessed for resection completeness.
Results
Fifty-eight patients fulfilled the inclusion criteria from all patients referred to the sarcoma service in a 12-month period. Of these, 42 out of 58 (72.4%) had benign neoplasms, 4 out of 58 (6.9%) had malignant tumours, 2 out of 58 (3.4%) an intermediate grade lesion, while 10 out of 58 (17.2%) were non-neoplastic. All 4 malignant lesions were completely excised at the time of excision biopsy.
Conclusions
Primary excision biopsy of small, indeterminate soft-tissue masses within the setting of a specialist sarcoma service is a suitable management option. Only a small proportion of small superficial soft-tissue lesions with indeterminate MRI features are malignant tumours.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Soft-tissue masses have a wide differential diagnosis, including benign neoplasms, malignant tumours that may be primary (sarcoma, lymphoma) or metastatic, and non-neoplastic lesions. They may also arise superficially or deep to the superficial fascia and vary considerably in size and imaging characteristics.
Optimal management requires accurate diagnosis, usually followed by surgical excision when appropriate. Diagnosis may be achieved by imaging alone, particularly for many benign [1, 2] and non-neoplastic lesions [3], but more frequently requires pre-operative biopsy. The latter is best performed in the setting of a multidisciplinary team (MDT) in a specialist centre [4–6] using percutaneous core needle biopsy (PCNB) with image guidance [7–9]. A potential complication of PCNB is the contamination of surrounding uninvolved tissue, which, although having a very low incidence of larger and deeper soft-tissue lesions [10, 11], could potentially be relatively more likely in the case of smaller lesions since maintaining the needle purely within the lesion at the time of biopsy could be more difficult.
It has been suggested that lesions measuring less than 3 cm in the maximal dimension and located superficial to the fascia can be treated with a primary surgical excision [12], but we are unaware of any study that has determined the suitability of such a protocol in a specialist setting, while the inadvertent or inadequate excision of unsuspected small sarcomas in non-specialist centres is a well-recognised phenomenon [13].
The purpose of this study is to determine the suitability of primary surgical excision biopsy of small, indeterminate superficial soft-tissue lesions referred as suspected sarcomas to a specialist sarcoma service.
Materials and methods
Because of the retrospective nature of the study, the local Research and Development Board has in a written consent declared that they did not require formal ethics approval. All patients referred to a specialist musculoskeletal sarcoma service during a 12-month period (beginning of January to end of December 2014) were identified from the new patient multidisciplinary team (MDT) meeting decision sheets and retrospectively analysed. The imaging investigations for all cases had been reviewed at a weekly sarcoma MDT meeting by an experienced (>20 years) musculoskeletal radiologist with a special interest in bone and soft-tissue tumour imaging. The decision to undertake a primary surgical excision biopsy for small (≤30 mm) superficial soft-tissue lesions that were considered indeterminate in nature by magnetic resonance imaging (MRI) criteria was made in collaboration with the attending orthopaedic oncology surgeon, and these patients formed the final study group. A lesion was considered indeterminate if an MRI diagnosis could not be suggested with confidence, such lesions typically being well-defined with intermediate T1-weighted (T1W), proton density-weighted (PDW) and T2-weighted (T2W) signal characteristics and intermediate-to-increased signal intensity (SI) on fat suppressed/short tau inversion recovery (STIR) sequences (Figs. 1, 2 and 3). In the hands and feet, lesions with typical imaging signal characteristics of a tenosynovial giant cell tumour and appropriate anatomical positions were excluded, but lesions within the size criteria that are centred away or not in contact with the joints and tendons or not of typical MRI signal intensity have been included. The histological diagnoses were categorized into benign neoplasms, intermediate neoplasms, malignant neoplasms and non-neoplastic lesions.
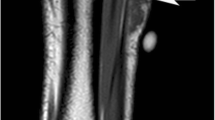
a, b Axial fat-suppressed proton density-weighted (PDW) fast spin echo (FSE) and sagittal T2-weighted (T2W) FSE magnetic resonance imaging (MRI) demonstrating a superficial dorsal upper arm lesion (white arrows) of intermediate signal intensity on both sequences. The maximal lesion dimension was 20 mm. Histology demonstrated this to be a low-grade spindle cell sarcoma (malignant neoplasm category lesion)
a, b Axial short tau inversion recovery (STIR) and coronal T1-weighted (T1W) spin echo (SE) MRI demonstrating a small superficial lesion close to the skin surface of the knee (white arrows) and of intermediate to mildly increased signal intensity. The maximal lesion dimension was 6 mm. Histology demonstrated this to be a benign fibrous histiocytoma (benign neoplasm category lesion)
a, b Axial PDW FSE and sagittal T2W FSE MRI demonstrating a small superficial lesion abutting the anterior margin of the superior patellar pole and quadriceps tendon (white arrows), which is of intermediate signal intensity on both sequences. Maximal lesion dimension was 14 mm. Histology demonstrated this to be an angioleiomyoma (benign neoplasm category lesion)
Excision was considered to be satisfactory if the lesion was histologically described as a complete resection with the narrowest clear margin of ≥3 mm, most specimens being reported two or three times by dedicated musculoskeletal histopathologists. If a subsequent further surgical resection was required, this histology result was also assessed for completeness of resection and potential complications from the initial excision biopsy.
Results
Fifty-eight patients met the inclusion criteria from all patients referred to the sarcoma service in a 12-month period. There were 29 male and 29 female patients with a mean age of 41 years (range 4–71 years).
The mean maximal lesion dimension was 14.2 mm (range 6–26 mm). Seventeen lesions measured ≤10 mm, 35 between 11 and 20 mm and 6 between 21 and 30 mm. With regard to location, 34 lesions arose in the upper limbs, 16 in the lower limbs and 8 on the trunk. Table 1 further subdivides the number of lesions in each anatomical location.
All excision biopsies yielded a definitive histological diagnosis. Forty-two lesions (72.4%) were benign neoplasms with a wide variety of histological diagnoses (Table 2), the most frequently encountered being pilomatrixoma (n = 6), tenosynovial giant cell tumour (n = 4) and schwannoma (n = 4). Four lesions (6.9%) were malignant, including a metastasis of unknown gastrointestinal origin, a malignant peripheral nerve sheath tumour (MPNST), a malignant melanoma and a spindle cell sarcoma (Table 2). Two patients (3.4%) had intermediate grade neoplasms, a soft-tissue giant cell tumour and a myxoinflammatory fibroblastic tumour, because of their rare potential for metastasis (Table 2). Ten lesions (17.2%) were non-neoplastic. The various histological diagnoses are displayed in Table 3.
All 4 malignant tumours occurred in adults. All four lesions were fully excised at the time of excision biopsy, with no further resection required owing to the clear margins at histological analysis. The patient with a spindle cell sarcoma (low-grade) underwent further wider local excision in view of the sarcoma diagnosis rather than an inadequate margin at primary excision, but the re-resection specimen confirmed complete resection at the time of initial excision biopsy.
The two sarcoma patients have been followed up in our service and, to date, at 2 years post-excision, no local recurrence or distant metastatic disease has been demonstrated. The remaining 2 patients with aggressive but non-sarcoma lesions were transferred to the relevant oncology services and managed elsewhere. Of the 2 patients with intermediate-grade lesions, the myxoinflammatory fibroblastic tumour patient had follow-up imaging at 1 year post-excision, which did not show any local recurrence, whereas the other patient chose to have follow-up elsewhere.
Discussion
Classical teaching is that a soft-tissue mass should be suspected of being a sarcoma if it is greater than 5 cm in dimension, located deep to the fascia and growing [14]. Older age at presentation is also a significant differentiating factor suggestive of malignancy [15]. However, it has also been well documented that soft-tissue sarcomas not uncommonly arise superficial to the fascia [15], and MRI features suggest that a superficial lesion might be more likely to be malignant have been described, including size greater than 5 cm, a lobular contour, fascial oedema and skin involvement [16]. It should be noted that superficial sarcomas are not uncommonly smaller than 5 cm, presumably because their superficial location results in earlier presentation.
The differential diagnosis of superficial soft-tissue lesions is wide and varies depending upon whether the lesion arises in the epidermis, dermis or subcutaneous fat [17]. Differential diagnosis also depends upon age at presentation and location in the body. A correct diagnosis can often be suggested by ultrasound in the case of lipomas, vascular malformations, epidermoid cysts and nerve sheath tumours, which were the commonest lesions in a large ultrasound study of patients presenting with superficial soft-tissue masses [18]. MRI is also of value in lesion characterization [1–3, 19], often precluding the need for pre-operative biopsy, but it is also recognized that many lesions, in particular, non-fat-containing sarcomas have indeterminate imaging features [20]. In such cases, as with tumours arising deep to the fascia, a pre-operative image-guided core needle biopsy should be performed by a radiologist working in the setting of a specialist sarcoma service, with the biopsy planned in conjunction with the operating surgeon [4–6]. The use of ultrasound or CT guidance for palpable lesions is associated with greater diagnostic accuracy than non-image-guided biopsy performed in the outpatient clinic [21], and MRI is also of value in planning needle biopsy [22]. Following diagnosis, wide surgical excision is the mainstay of treatment, with either neo-adjuvant or adjuvant radiotherapy utilized in selected cases [4–6].
The assumption that small, superficial soft-tissue tumours are unlikely to be malignant may be true, and is supported by the fact that only 11 out of 247 superficial soft-tissue masses diagnosed by ultrasound were malignant [18], but the inadvertent and/or inadequate excision of unsuspected sarcomas is also not uncommon. Such lesions are often not imaged before excision and are commonly incompletely excised, the most frequent diagnosis being leiomyosarcoma [13]. In such cases, re-excision of the tumour bed is required, often resulting in a greater resection of tissue than would have been necessary had the tumour been adequately treated initially. If radiotherapy is subsequently required, then this also necessitates wider field coverage [23–25]. Therefore, any indeterminate soft-tissue mass should be considered to represent a sarcoma until proven otherwise, and referred to a specialist sarcoma service for biopsy [6], irrespective of size or site in relation to the fascia.
A potential risk of needle biopsy is the contamination of healthy surrounding tissue; although this risk is potentially very low in larger and deeper lesions [10, 11], to the authors’ knowledge, there is little published literature regarding the frequency of tumour seeding following percutaneous biopsy in small superficial sarcomas and it may be that this risk is greater with tumours that are <2 cm in maximal dimension, as maintaining the needle purely within the lesion at the time of biopsy may be more difficult. This could potentially result in incomplete excision and a higher risk of local recurrence, although we are unaware of any study that has shown this to be the case.
Because of the indeterminate nature of the lesions, we assume them to be malignant. Although the ultrasound study by Hung et al. [18] indicated that less than 5% of pathologically proven superficial soft-tissue masses were malignant, the commonest lesions in their study were lipomas, vascular malformations, epidermoid cysts and benign neural tumours, accounting for approximately 65% of the cases. Such lesions can usually be well characterized by ultrasound and MRI and would not fit into our criteria of being indeterminate. This would suggest that the percentage of lesions with indeterminate imaging features that are malignant might be higher. Lesion size was not taken into consideration, but Calleja et al. in their study [16] did suggest that size greater than 5 cm might increase the likelihood of malignancy in superficial soft-tissue tumours. However, a study looking at the characteristics of inadvertently resected sarcomas found 50% of them to be small and superficial to the fascia [13]. This may be due to misinterpretation of the current guidelines on the management of soft-tissue tumours, which state that a sarcoma should be suspected when a lesion is greater than 5 cm in dimension, deep to the fascia and growing [14]. However, the guidelines do not state the opposite to be the case, and small superficial lesions may well be malignant, although the likelihood of this is unknown.
Some limitations of the study include its retrospective nature, and also the small number of sarcomas within the study group relative to the benign and non-neoplastic lesions, but this reflects the rarity of such lesions. The relative lack of long-term follow-up of the patients with sarcoma is also a potential limitation, but it is known that no local recurrence has been demonstrated for these patients at 2 years post-resection.
Recent European Guidelines have suggested that superficial lesions less than 3 cm in dimension might safely be treated using primary excision biopsy [10]. The current study suggests that primary excision of small, superficial soft-tissue masses that are indeterminate according to MRI criteria might be a safe practice, but only in the setting of a specialist sarcoma service, with none of 58 lesions being incompletely excised. It also identifies that superficial indeterminate lesions with a maximal dimension less than 3 cm are very unlikely to be malignant, with only 4 out of 58 cases (6.9%) being malignant.
References
Goodwin RW, O’Donnell P, Saifuddin A. MRI appearances of common benign soft-tissue tumours. Clin Radiol. 2007;62:843–53.
Walker EA, Fenton ME, Salesky JS, Murphey MD. Magnetic resonance imaging of benign soft tissue neoplasms in adults. Radiol Clin N Am. 2011;49:1197–217. vi.
Crundwell N, O’Donnell P, Saifuddin A. Non-neoplastic conditions presenting as soft-tissue tumours. Clin Radiol. 2007;62:18–27.
Clarkson P, Ferguson PC. Primary multidisciplinary management of extremity soft tissue sarcomas. Curr Treat Options in Oncol. 2004;5:451–62.
Mendenhall WM, Indelicato DJ, Scarborough MT, et al. The management of adult soft tissue sarcomas. Am J Clin Oncol. 2009;32:436–42.
Grimer R, Judson I, Peake D, Seddon B. Guidelines for the management of soft tissue sarcomas. Sarcoma. 2010;2010:506182.
Hillen TJ, Baker JC, Jennings JW, Wessell DE. Image-guided biopsy and treatment of musculoskeletal tumors. Semin Musculoskelet Radiol. 2013;17:189–202.
Avedian RS. Principles of musculoskeletal biopsy. Cancer Treat Res. 2014;162:1–7.
Traina F, Errani C, Toscano A, et al. Current concepts in the biopsy of musculoskeletal tumors. J Bone Joint Surg Am. 2015;97.e7.
Berger-Richardson D, Swallow CJ. Needle tract seeding after percutaneous biopsy of sarcoma: risk/benefit considerations. Cancer. 2017;123:560–7.
UyBico SJ, Motamedi K, Omura MC, et al. Relevance of compartmental anatomic guidelines for biopsy of musculoskeletal tumors: retrospective review of 363 biopsies over a 6-year period. J Vasc Interv Radiol. 2012;23:511–8, 518.e1–2.
Noebauer-Huhmann IM, Weber M-A, Lalam RK, et al. Soft tissue tumors in adults: ESSR-approved guidelines for diagnostic imaging. Semin Musculoskelet Radiol. 2015;19:475–82.
Dyrop HB, Safwat A, Vedsted P, et al. Characteristics of 64 sarcoma patients referred to a sarcoma center after unplanned excision. J Surg Oncol. 2016;113:235–9.
National Institute for Health and Clinical Excellence. Referral guidelines for suspected cancer. NICE clinical guideline no.27. [Internet]. National Institute for Health and Clinical Excellence. 2005. Available from: www.nice.org.uk/CG027
Datir A, James SLJ, Ali K, Lee J, Ahmad M, Saifuddin A. MRI of soft-tissue masses: the relationship between lesion size, depth, and diagnosis. Clin Radiol. 2008;63:373–78, commentary 379–80.
Calleja M, Dimigen M, Saifuddin A. MRI of superficial soft tissue masses: analysis of features useful in distinguishing between benign and malignant lesions. Skeletal Radiol. 2012;41:1517–24.
Blacksin MF, Ha D-H, Hameed M, Aisner S. Superficial soft-tissue masses of the extremities. Radiographics. 2006;26:1289–304.
Hung EHY, Griffith JF, Ng AWH, Lee RKL, Lau DTY, Leung JCS. Ultrasound of musculoskeletal soft-tissue tumors superficial to the investing fascia. Am J Roentgenol. 2014;202:W532–40.
Zhuang KD, Tandon AA, Ho BCS, Chong BK. MRI features of soft-tissue lumps and bumps. Clin Radiol. 2014;69:e568–83.
Beaman FD, Kransdorf MJ, Andrews TR, Murphey MD, Arcara LK, Keeling JH. Superficial soft-tissue masses: analysis, diagnosis, and differential considerations. Radiographics. 2007;27:509–23.
Narvani AA, Tsiridis E, Saifuddin A, Briggs T, Cannon S. Does image guidance improve accuracy of core needle biopsy in diagnosis of soft tissue tumours? Acta Orthop Belg. 2009;75:239–44.
Khoo MMY, Saifuddin A. The role of MRI in image-guided needle biopsy of focal bone and soft tissue neoplasms. Skeletal Radiol. 2013;42:905–15.
Chandrasekar CR, Wafa H, Grimer RJ, Carter SR, Tillman RM, Abudu A. The effect of an unplanned excision of a soft-tissue sarcoma on prognosis. J Bone Joint Surg (Br). 2008;90:203–8.
Koulaxouzidis G, Schwarzkopf E, Bannasch H, Stark GB. Is revisional surgery mandatory when an unexpected sarcoma diagnosis is made following primary surgery? World J Surg Oncol. 2015;13:306.
Pretell-Mazzini J, Barton MD, Conway SA, Temple HT. Unplanned excision of soft-tissue sarcomas: current concepts for management and prognosis. J Bone Joint Surg Am. 2015;97:597–603.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Khoo, M., Pressney, I., Hargunani, R. et al. Small, superficial, indeterminate soft-tissue lesions as suspected sarcomas: is primary excision biopsy suitable?. Skeletal Radiol 46, 919–924 (2017). https://doi.org/10.1007/s00256-017-2635-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-017-2635-4