Abstract
Osteoid osteoma and osteoblastoma are rare benign bone-forming tumors with very similar histological features. They are nowadays considered as two distinct entities. Progression of an osteoid osteoma to osteoblastoma is considered very rare with only a few cases reported in the literature. Herein we describe a case of an osteoid osteoma of the thoracic spine in a 29-year-old woman that was initially treated conservatively and progressed to osteoblastoma 5 years following the initial diagnosis. Imaging revealed an increase in the size of the spinal lesion that was surrounded by extensive paraspinal abnormal soft tissue that raised suspicion for sarcomatous transformation. The final diagnosis was established by CT-guided biopsy of both the bone lesion and the paraspinal soft tissue, which excluded malignancy and revealed an osteoblastoma surrounded by plasma cell-rich chronic inflammation. The patient then underwent wide surgical excision of the lesion and paraspinal soft tissue component that confirmed the diagnosis. Follow-up with MRI over the next 12 months was unremarkable, with no signs of recurrence or spinal instability. This unique presentation of an osteoblastoma has not been previously described. This case also demonstrates the importance of follow-up of osteoid osteomas that are treated conservatively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoid osteoma and osteoblastoma are rare benign bone-forming tumors with very similar histological features that are nowadays considered as two distinct entities. Transformation of an osteoid osteoma into osteoblastoma is very rare and only a few cases have been reported in the literature [1–6]. Herein, we describe the unique imaging findings of a spinal osteoid osteoma that progressed into osteoblastoma over a 5-year period in a 29-year-old woman. The bone lesion was surrounded by extensive paraspinal soft tissue, which raised suspicion for sarcomatous transformation. CT-guided biopsy excluded malignancy and revealed an osteoblastoma surrounded by plasma cell-rich chronic inflammation. This unique presentation of an osteoblastoma has not been previously described.
Case report
A 29-year-old woman with a known osteoid osteoma of the spine was imaged in our institution as part of work-up for worsening symptoms. The patient had presented 5 years previously with back pain worsening during the night that resolved with anti-inflammatory medication. An initial computerized tomography (CT) scan revealed a 5-mm lesion on the right posterolateral aspect of T4 vertebral body with typical features of osteoid osteoma (Fig. 1). Four months later, follow-up revealed mild enlargement of the nidus of the lesion (Fig. 2). The patient was offered percutaneous treatment with radiofrequency (RF) ablation or surgical excision but chose conservatory management. Within the next 5 years, there were periods of remission followed by periods of exacerbation of the pain that responded well to aspirin and non-steroidal anti-inflammatory drugs. No further follow-up imaging studies were performed in this period until the patient represented 5 years later for reassessment.
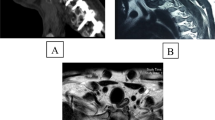
A CT scan was then performed that demonstrated progression of the initial lesion to a 23-mm, well-defined, lytic lesion on the right posterolateral aspect of T4 vertebral body with sclerotic margins and an associated paraspinal soft tissue mass adjacent to the lesion as well as sclerosis of the T4 and T5 vertebral bodies (Fig. 3a). Further imaging with magnetic resonance imaging (MRI) demonstrated both the bone lesion and the extension into the paraspinal soft tissues (Fig. 3b-d).
There is a well-defined expansive lytic lesion with sclerotic margins on the right posterolateral aspect of T4 vertebral body extending to the right pedicle (large arrow). The lesion occupies the ipsilateral foramen, compresses the exiting nerve root and causes minimal distortion of the cord. The lesion exhibits inhomogeneous low signal intensity on T2W (b) and T2W/FS (c) (arrows). There is a further paraspinal soft tissue mass exhibiting high signal intensity on T2W (b) and T2W/FS (c) and intermediate signal intensity on T1W (d). Note the low T1 signal intensity of T4 and T5 vertebral bodies due to sclerosis
A spinal osteoblastoma with reactive paraspinal soft tissue was considered to be the more likely diagnosis with less likely diagnoses including sarcomatous transformation or even lymphoma. A CT-guided biopsy of the soft-tissue component of the lesion (Fig. 4a) was initially performed and the histopathology showed reactive fibrofatty tissue with benign plasma cell and lymphoid infiltrates with no evidence of malignancy (Fig. 4b). This was followed by a second CT-guided biopsy of the osseous lesion (Fig. 4c), which was performed under sedation and histopathology revealed a benign osseous lesion with findings consistent with an osteoblastoma (Fig. 4d).
CT-guided biopsy of the paraspinal soft tissue lesion (a) showing fibrofatty tissue with focal inflammatory infiltrates composed of plasma cells and small lymphocytes with a mixed B and T populations and no evidence of malignancy (b). CT-guided biopsy of the spinal lesion (c) showing fragments of a bone tumor composed of interlacing spicules of osteoid and irregular and mineralized bone lined with osteoblasts. Osteoclasts like giant cells are also present. The stroma is composed of fibrovascular connective tissue (d)
Some weeks later, the patient underwent wide surgical excision of the spinal lesion and paraspinal soft tissue mass. The surgical procedure included resection of the right 5th rib followed by right hemilaminectomy and partial somatectomy of T4 and T5 vertebrae en block with the lesion. Then the soft tissue component was separately dissected away. Biopsy of the bony component of the excision specimen confirmed the diagnosis of osteoblastoma with no signs of cytological atypia or mitotic activity of the osteoblasts. Biopsy of the paraspinal soft tissue showed fibro-adipose tissue with predominantly plasma cell-rich inflammation and multiple small lymphoid follicles, with focal collagen accumulation and myofibroblastic proliferation and moderate obliterative phlebitis in keeping with plasma cell-rich chronic inflammation with no evidence of atypical tumor cells.
CT and MRI follow-up after 6 and 12 months demonstrated complete excision of the lesion with no signs of recurrence and complete resolution of the paraspinal chronic inflammatory reactive soft tissue with mild fibrosis and pleural thickening at the area of the operation. No spinal instability or other abnormalities were seen (Fig. 5).
Discussion
Osteoblastoma and osteoid osteoma are rare benign bone-forming tumors with very similar histological features that usually arise in the 2nd decade of life and are currently considered as two distinct entities [2]. The size of the lesion is considered as the most reliable criterion with tumors larger than 15 mm considered as osteoblastomas and smaller then 15 mm considered as osteoid osteomas [3]. Apart from the size, these two entities differ in their topographic distribution, clinical presentation, and potential for progression [2].
In our daily clinical practice, the diagnosis of an osteoid osteoma is usually straightforward and is based on clinical and imaging findings. Lesions are usually smaller than 10 mm. Most patients present with typical pain that worsens during the night and resolves with non-steroidal anti-inflammatory drugs. In most cases, the patients are referred for CT-guided RF ablation and only a few patients undergo surgical excision. In exceptional cases, patients refuse any kind of intervention and prefer chronic use of non-steroidal anti-inflammatory drugs. In the latter group, ossification of the nidus and disappearance of the lucent zone indicate radiological regression of an osteoid osteoma [3].
In our case, the patient refused any kind of intervention. There were periods of remission followed by periods of exacerbation of the pain responded well to aspirin and non-steroidal anti-inflammatory drugs. Unfortunately, the patient did not have any follow-up studies within the subsequent 5-year period.
The imaging characteristics of the lesion and the preexistence of an osteoid osteoma at the same anatomic location that was not treated by an interventional procedure raised the suspicion of progression to a spinal osteoblastoma. However, the presence of a significant amount of paraspinal soft tissue surrounding the lesion was an atypical finding, which prompted the need for biopsy. Although we considered that this tissue may represent reactive soft tissue due to chronic hyperemia/inflammation, we could not exclude the possibility of sarcomatous transformation or even the possibility of a coexistence lymphoma. The biopsy from the soft tissue and the osseous lesion revealed a typical osteoblastoma surrounded by reactive fibrofatty tissue with benign lymphoid infiltrates.
Very few cases of osteoid osteomas progressing to osteoblastoma are reported in the literature [1–6]. To our knowledge, this is the first case of an osteoblastoma surrounded by inflammatory reactive soft tissue. There is no clear explanation for that, though chronic hyperemia/inflammation may stimulate the accumulation of lymphocytes and plasma cells adjacent to the lesion.
Osteoblastomas usually behave more aggressively in the bone than osteoid osteomas. In our case, although the lesion had significantly enlarged and involved a significant portion of the vertebral body and the right pedicle, it was well demarcated from adjacent tissues. The adjacent bone was intact and sclerosis of T4 and T5 vertebral bodies was attributed to osteoblastic response due chronic hyperemia/inflammation. These findings were against an aggressive bone lesion. Otherwise, vertebral body sparing surgical procedure would be more difficult with increased risk of incomplete excision of the lesion and vertebral body replacement would be a preferable option.
The natural history of osteoid osteomas treated conservatively is unknown, since current practice for almost all patients is RF ablation or surgical treatment for pain relief and no follow-up cross-sectional imaging studies are performed. In addition, there is no sufficient evidence in the literature concerning imaging follow-up of osteoid osteomas that are treated conservatively. Thus, we propose regular follow-up with limited CT at the area of the lesion in cases of osteoid osteomas that are treated conservatively or even in cases where there are concerns for incomplete tumor ablation/resection. Complete radiological regression should only be deducted if there is sclerosis and complete disappearance of the lucent zone of the nidus. In cases that demonstrate enlargement of the lesion or other suspicious features like surrounding inflammation, then a CT-guided biopsy or surgical excision of the lesion should be considered.
References
Cappuccio M, De Iure F, Amendola L, Corghi A, Gasbarrini A. Cervical osteoid osteoma progression to osteoblastoma. 1. Spine J. 2014;14(6):1070–1.
Chotel F, Franck F, Solla F, et al. Osteoid osteoma transformation into osteoblastoma: fact or fiction? Orthop Traumatol Surg Res. 2012;98(6 Suppl):S98–104.
Bruneau M, Polivka M, Cornelius JF, George B. Progression of an osteoid osteoma to an osteoblastoma. Case report J Neurosurg Spine. 2005;3(3):238–41.
Bettelli G, Tigani D, Picci P. Recurring osteoblastoma initially presenting as a typical osteoid osteoma. Report of two cases. Skelet Radiol. 1991;20(1):1–4.
Pieterse AS, Vernon-Roberts B, Paterson DC, Cornish BL, Lewis PR. Osteoid osteoma transforming to aggressive (low grade malignant) osteoblastoma: a case report and literature review. Histopathology. 1983;7(5):789–800.
Sung HW, Liu CC. Can osteoid osteoma become osteoblastoma? A case report. Arch Orthop Trauma Surg. 1979;95(3):217–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Michaelides, M., Pantziara, M., Petridou, E. et al. Spinal osteoid osteoma progressed to osteoblastoma with paraspinal soft tissue mass: a unique presentation. Skeletal Radiol 46, 379–383 (2017). https://doi.org/10.1007/s00256-016-2555-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-016-2555-8