Abstract
Objective
To describe a lateral fluoroscopically guided retrocalcaneal bursa injection technique, report patient outcomes at 1–4 weeks after steroid/anesthetic retrocalcaneal bursal therapeutic injection, and correlate pre-injection diagnostic heel ultrasound variables with improvement in patient pain scores.
Materials and methods
After IRB approval, fluoroscopically guided therapeutic retrocalcaneal bursa injections performed using a lateral approach were retrospectively reviewed. Pre-injection heel ultrasound results and pre- and post-injection patient VAS pain scores (scale 0–10) were recorded. The Wilcox matched-pair test compared pain scores, and Spearman’s rho assessed for correlation between pain score changes and heel ultrasound results.
Results
Thirty-two injections were performed in 30 patients (25 females, 5 males; mean 56.5 ± 9.3 years, range 39–75 years; 21 left heel, 11 right heel) with technical success in 32 of 32 cases (100 %). Insertional Achilles tendon pathology and retrocalcaneal bursitis were present in 31 of 32 cases (97 %) and 16 of 32 cases (50 %), respectively. Median pre- and post-procedure pain scores were 8 (IQR 7, 10) and 1.75 (IQR 0, 6). A statistically significant decrease in pain score was observed following injection, with a median change of 4.75 (IQR 3, 8; p < 0.001). Clinically significant response (>50 % reduction in pain score) was present in 69 % (95 % CI, 0.52–0.86; p < 0.001). No significant correlation was identified between a decrease in pain score and a sonographically abnormal Achilles tendon or retrocalcaneal bursa.
Conclusion
Fluoroscopically guided retrocalcaneal bursal steroid/anesthetic using a lateral approach is an effective technique. This technique yielded 100 % technical success and a clinically significant decrease in patient pain scores (p < 0.001).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The retrocalcaneal (RC) bursa is located between the posterior superior calcaneus and the Achilles tendon attachment onto the calcaneus. Retrocalcaneal bursitis is due to inflammation of the RC bursa. This inflammation may be associated with degenerative changes within the insertional Achilles tendon [1]. While Achilles insertional tendinopathy and retrocalcaneal bursitis are two different entities in the range of Achilles tendon pathology, they may co-exist, and patients with RC bursitis often present similarly to those with insertional Achilles tendinopathy and/or tear. The hallmark of retrocalcaneal bursitis is pain anterior to the Achilles tendon, often accompanied by a positive two-finger “squeeze test,” in which pain is elicited by applying pressure medially and laterally, immediately anterior to the Achilles tendon [1–3].
We describe a fluoroscopically guided injection technique into the retrocalcaneal (RC) bursa using a lateral approach in patients presenting with posterior heel pain and clinically suspected retrocalcaneal bursitis and/or insertional Achilles pathology. To our knowledge, this technique has not been previously reported in the literature. Additionally, we report on post-injection short-term patient outcomes and correlate these outcomes with pre-injection diagnostic heel ultrasound findings of retrocalcaneal bursitis and/or insertional Achilles pathology.
Materials and methods
Patient selection
Institutional review board approval was obtained for this retrospective study. Informed consent was waved. All procedures performed were in accordance with the ethical standards of the institution. Consecutive patients referred for fluoroscopically guided RC bursa steroid/aesthetic injection over 10 months were studied (September 2013–July 2014). All patients were referred for RC bursal injection following a clinical diagnosis of suspected retrocalcaneal bursitis and/or Achilles insertional tendinopathy.
Pre-injection workup
Diagnostic ultrasound
All patients at our institution undergo a diagnostic heel ultrasound (US) examination immediately prior to the fluoroscopically guided RC bursa injection. All pre-injection diagnostic heel ultrasound examinations were performed by one of two fellowship-trained musculoskeletal radiologists or a single musculoskeletal radiology fellow under direct supervision. Gray-scale and color Doppler ultrasound long- and short-axis images were obtained using an ACUSON Sequoia 512 US machine and a 12–15-MHz linear probe to assess for distal Achilles pathology and the presence of RC bursitis. Dynamic sonographic evaluation was performed to evaluate for Achilles tendon tear with passive movement of the foot.
Pain scores
A visual analog scale (VAS) pain score (scale 0–10) was obtained from the patient prior to the procedure by the performing radiologist, and the score was recorded in the patient's medical record.
Injection technique: a lateral fluoroscopic approach
All patients referred for RC bursa injection without a high-grade or full-thickness Achilles tendon tear on pre-injection diagnostic US are offered the requested retrocalcaneal bursal injection, regardless of the Achilles and bursal imaging findings on pre-injection diagnostic ultrasound evaluation. The risks and benefits of the procedure are explained to the patient, and informed consent is obtained. Discussed risks include infection, bleeding, allergic reaction to contrast and/or medications, and risk of Achilles tendon tear. Diabetics are educated on the risk of temporary high glucose levels following cortisone injection and therefore instructed to monitor sugar levels regularly. Patient allegies and current medications are reviewed (including any blood thinners), and review of systems is performed to exclude active infection. A standardized “time out” is performed according to the institutional ptotocol.
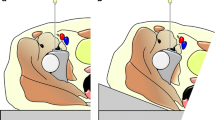
The patient is placed in a lateral decubitus position on the fluoroscopic table, with the affected side up. The patient's hindfoot is elevated on the table with a rolled towel, and an additional towel is often placed to ensure stability of the foot on the table. A radiodense marker is placed over the hindfoot. The image detector is then rotated to provide a true lateral view of the tibiotalar joint, serving as a scout image. The image is collimated to include only the posterior heel region in the imaged area. The radiodense marker is adjusted to overlie the posterior superior aspect of the calcaneus within a few millimeters of the posterior cortex.
The skin is marked, and the area is prepared and draped in the usual sterile fashion. Using a 27-gauge needle, 1 % lidocaine is injected for subcutaneous local anesthesia at the marked site. A 1.5-inch 25-gauge needle is then advanced in parallel with the image detector such that the needle tip overlies the hub. A fluoroscopic image demonstrates a target appearance of the needle at the posterior superior calcaneus. The target appearance is due to the needle tip directly overlapping the needle hub. If the hub has been prefilled with contrast, the image instead demonstrates the round density of the contrast-filled hub, without visualization of the needle shaft, indicating the needle tip directly overlaps the needle hub (Fig. 1a). Any required adjustments to accomplish this alignment are made within the very superficial soft tissues prior to further needle advancement. Often, stacked sterile guaze is used to stabilize the needle within the superficial soft tissues to allow for fine-tuning of the needle angulation before advancement. Once the needle angle has been optimized, the needle is advanced to the bone at the level of the posterior superior calcaneus.
a A true lateral fluoroscopic image of the hindfoot demonstrates a contrast-filled needle hub at the posterior superior calcaneus. This appearance is due to the needle tip directly overlapping the needle hub. b Fluoroscopic image demonstrates curvilinear c-shaped opacification of the retrocalcaneal bursa, closely abutting the posterior superior aspect of the calcaneus. c Fluoroscopic image after 0.2 ml contrast injection at the posterior calcaneus demonstrates linear vertical striations, indicating opacification of Achilles tendon fibers. The needle requires repositioning anterosuperiorly prior to steroid injection. d Flouroscopic image demonstrated diluted, decreased density of the previously injected contrast, having the appearance of contrast “washout.” The contrast pattern is consistent with the contour of the retrocalcaneal bursa
The needle is then retracted slightly, directed immediately posterior to the superior calcaneus, and advanced approximately 3–5 mm into the retrocalcaneal bursa. A syringe with connected tubing pre-filled with Isovue 200 is then attached to the hub of the needle, with care taken to fill the hub of the syringe with contrast. Approximately 0.1–0.2 ml of contrast is injected to confirm the needle position. The fluoroscopic image demonstrates curvilinear c-shaped opacification of the retrocalcaneal bursa, closely abutting the posterior superior aspect of the calcaneus (Fig. 1b). The contrast pattern should not demonstrate a linear vertical configuration, which would indicate opacification of the Achilles tendon insertional fibers or Achilles paratenon; this finding would prompt needle repositioning, typically anterosuperiorly (Fig. 1c).
Once contrast opacification confirms the needle tip is within the RC bursa, a mixture of 1 ml of 0.25 % bupivacaine and 1.5 ml of Depo-Medrol (40 mg/ml) is injected into the RC bursal space. It is a smooth, low-pressure injection. The volume of steroid/anesthetic that is injected is determined by resistance to the injection. Once resistance has been encountered, typically after 0.8–1.5 ml has been injected, the injection is complete. An additional fluoroscopic image is obtained demonstrating diluted, decreased density of the previously injected contrast, having the appearance of contrast “washout” (Fig. 1d). This final image further confirms that the steroid/anesthetic injection was within the retrocalcaneal bursa.
Post-injection patient follow-up
One to 4 weeks after the injection, each patient is contacted by the performing radiologist as per routine for clinical follow-up. During this follow-up conversation, a short-term post-injection VAS pain score (scale 0-10) was obtained from the patient and recorded in the medical record.
Data collection
Patient data
Demographic information was recorded for each patient, including the age, gender, and side of heel pain. Pre- and post-injection VAS pain scores (scale 0–10) for all patients were recorded in a data file.
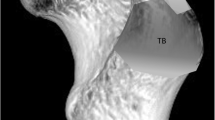
Ultrasound review
Two musculoskeletal radiologists reviewed the pre-injection diagnostic heel ultrasound images in consensus and recorded the presence or absence of sonographic distal Achilles tendon pathology and RC bursitis for each case. The reviewers were blinded with regard to the patient demographics, technical success of the procedure, and pre- and post-injection pain scores. Patients were categorized as having sonographic retrocalcaneal bursitis if there was bursal distension >3 mm (Fig. 2). Patients were categorized as not having sonographic retrocalcaneal bursitis if there was no bursal fluid or if bursal distension was <3 mm [4]. Patients were categorized as having sonographic distal Achilles tendon pathology if there was hypoechoic tendon enlargement >7 mm or Doppler flow within the Achilles tendon (Fig. 3). Patients were categorized as not having sonographic distal Achilles tendon pathology if the tendon was <7 mm and uniform in thickness and echogenicity in the longitudinal plane, had a flat or concave anterior margin in the transverse plane, and demonstrated no internal Doppler flow [5, 6].
Procedure review
The fluoroscopic case images from each patient were reviewed by two musculoskeletal radiologists in consensus to evaluate for technical success of the injection into the RC bursa using the described approach.
Statistical analysis
Median scores and interquartile range (IQR; 25th and 75th percentile) were calculated for pain scores pre- and post-injection as well as for the calculated change in pain score following injection. A clinically significant response was defined as a >50 % decrease in the pain score. Wilcox matched-pairs test was used to compare scores. One-sample test of proportions was used to determine whether there were a statistically significant number of clinically significant responses, with the assumption that 0 % would have a clinically significant response without treatment. Spearman’s rho was used to assess for correlation between a decrease in the pain score and other variables (including patient age, gender, side affected, and ultrasound findings). A P value < 0.05 was used to determine clinical significance.
Results
Thirty-two injections were performed in 30 patients (25 females, 5 males; mean age 56.5 ± 9.3 years, range 39–75 years). Twenty-one injections were performed on the left RC bursa and 11 on the right. Technical procedure success was achieved in 100 % of cases. Pre-injection diagnostic heel ultrasound identified 31 of 32 cases (97 %) cases with sonographic distal Achilles tendon pathology and 16 of 32 (50 %) cases with sonographic RC bursitis.
Pain scores before and after injection
Median pre- and post-injection pain scores were 8 (IQR 7, 10) and 1.75 (IQR 0, 6), respectively (Table 1). There was a statistically significant decrease in pain score following injection, with a median decrease of 4.75 (IQR 3, 8; p < 0.001). Clinically significant response, defined as a >50 % decrease in pain score, was present in 69 % (95 % confidence interval 0.52–0.86; p < 0.001). Fourteen patients (44 %) were pain-free (pain score of 0) at post-injection follow-up. There were no short-term complications reported during the post-injection patient follow-up calls.
Correlation between clinical and sonographic variables and response to injection
There was no significant correlation between a decrease in pain score and gender (ρ = 0.026, p = 0.887), age (ρ = -0.055, p = 0.765), or side injected (ρ = 0.143, p = 0.434). There was also no significant correlation between a decrease in pain score and the presence of abnormal sonographic distal Achilles tendon pathology (ρ = -0.162, p = 0.394) or RC bursitis (ρ = 0.181, p = 0.337) (Table 2).
Discussion
Corticosteroids have been used to treat multiple orthopedic conditions and may be administered blindly. Some clinicians advise against blind injection near the Achilles tendon because of the possibility of inadvertent intra-tendinous injection and fear of subsequent Achilles tendon rupture [7, 8]. Animal studies have demonstrated adverse biomechanical affects from intra-tendinous Achilles injection [9], and post-steroid Achilles tendon rupture has been reported in the literature, although the true level of risk is not known [2, 3, 7, 10].
The retrocalcaneal bursa is located between the calcaneus anteriorly, the Achilles tendon posteriorly, and Kagar’s fat pad superiorly [7, 8, 11]. Histological investigation of the retrocalcaneal bursa has revealed that a synovial membrane completely covers the entire bursal surface of the Achilles tendon [11]. A major benefit of image-guided injection into the retrocalcaneal bursa is confident injection into the synovial-lined bursal space and avoidance of an intra- or peri-tendon Achilles injection.
Fluoroscopically guided injection into the retrocalcaneal bursa is easily performed. At our institution, image-guided retrocalcaneal bursal injections are performed under fluoroscopic or sonographic guidance, depending on the availability of resources, which fluctuates with the clinical schedule. Knowledge of the fluoroscopic technique is useful in our environment and may also be useful for practice settings where outpatient musculoskeletal procedures typically occupy the fluoroscopic suite.
Significant short-term pain reduction was achieved with our technique, with a median pain score change of -4.75, clinically significant response in 69 % of patients (p < 0.001), and 44 % of patients pain-free (VAS pain score = 0) at short-term follow-up. Since patients with RC bursitis often clinically present similarly to those with insertional Achilles tendinopathy [1–3], we analyzed the sonographic presence or absence of insertional Achilles pathology and RC bursitis in our population of patients with posterior heel pain referred for retrocalcaneal bursa injection. Sonographic distal Achilles tendon tendinopathy or tendinopathy with partial tear was identified in 97 % of cases, and retrocalcaneal bursitis was present in 50 % of cases. We did not find a significant association between pain response to injection in our study and the presence of Achilles tendon pathology or retrocalcaneal bursitis. We conclude that patients with Achilles tendon pathology and without sonographic retrocalcaneal bursitis can nevertheless benefit from bursal injection, as they did in our study.
There were no short-term complications reported in our study. Although we did not formally study patient outcomes beyond 1–4 weeks, in follow-up with the referring physicians, Achilles tendon rupture occurred in one patient 2 months following a fluoroscopically guided bursal injection, preceded immediately by a fall. The causal relationship between the fall versus the recent steroid injection and the Achilles rupture is unknown.
The study is limited by its retrospective analysis. Clinical follow-up was limited to 4 weeks; therefore, only short-term affects were studied. Further research is required to determine the longer-term risks and benefits of this procedure. Lastly, the study relies on patient pain scores to measure short-term successful clinical outcome.
References
Uquillas CA, Guss MS, Ryan DJ, Jazrawi LM, Strauss EJ. Everything Achilles: knowledge update and current concepts in management. J Bone Joint Surg Am. 2015;97(14):1187–95.
Wijesekera NT, Chew NS, Lee JC, et al. Ultrasound-guided treatments for chronic Achilles tendinopathy: an update and current status. Skelet Radiol. 2010;39:425–34.
Schepsis AA, Jones H, Haas AL. Achilles tendon disorders in athletes. Am J Sports Med. 2002;30(2):287–305.
Nazarian LN, Rawool NM, Martin CE, Schweitzer ME. Synovial fluid in the hindfoot and ankle: detection of amount and distribution with US. Radiology. 1995;197(1):275–8.
Pang BS, Ying M. Sonographic measurement of achilles tendons in asymptomatic subjects: variation with age, body height, and dominance of ankle. J Ultrasound Med. 2006;25(10):1291–6.
Leung JL, Griffith JF. Sonography of chronic Achilles tendinopathy: a case-control study. J Clin Ultrasound. 2008;36(1):27–32.
Metcalfe D, Achten J, Costa M. Glucocotricosteroid injections in lesions of the Achilles tendon. Foot Ankle Int. 2009;30(7):661–5.
Asplund C, Best TM. Achilles tendon disorders. BMJ. 2013;346:f1262.
Hugate R, Pennypacker J, Saunders M, Juliano P. The effects of intratendinous and retrocalcaneal intrabursal injections of corticosteroid on the biomechanical properties of rabbit Achilles tendons. J Bone Joint Surg. 2004;86A:794–801.
Turmo-Garuz A, Rodas G, Balius R, et al. Can local corticosteroid injection in the retrocalcaneal bursa lead to rupture of the Achilles tendon and the medial head of the gastrocnemius muscle? Musculoskelet Surg. 2014;98:121–6.
Kachlik D, Baca V, Cepelik M, et al. Clinical anatomy of the retrocalcaneal bursa. Surg Radiol Anat. 2008;30:347–53.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Goldberg-Stein, S., Berko, N., Thornhill, B. et al. Fluoroscopically guided retrocalcaneal bursa steroid injection: description of the technique and pilot study of short-term patient outcomes. Skeletal Radiol 45, 1107–1112 (2016). https://doi.org/10.1007/s00256-016-2368-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-016-2368-9