Abstract
Vascular injury as a consequence of dislocated bone fragments after hip fractures is a rare complication. We report a case of a 78-year-old male who developed a pseudoaneurysm of the profunda femoris artery during rehabilitation after intramedullary fixation for a pertrochanteric hip fracture. As this procedure was minimally invasive, open reposition and fixation of the dislocated lesser trochanter were not performed. The pseudoaneurysm was diagnosed through duplex ultrasound and CT angiography and treated with thrombin injections and an endovascular Wallgraft covered stent. The imaging features are described in the article. Although a pseudoaneurysm is a rare complication after hip fractures, the development should be considered, in particular when symptoms such as pulsatile swelling or venous engorgement are presented.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Around 90 % of hip fractures occur in the elderly (age >65 years) because of secondary causes such as a reduction in bone mineral density, poor balance and environmental hazards [1]. It is estimated that the lifetime risk for hip fractures is 18 % for females and 6 % for males [2]. Fractures of the trochanteric complex are classified as simple pertrochanteric fractures (A1), multifragmentary pertrochanteric fractures (A2) and intertrochanteric fractures (A3). Depending on the fracture type, management of these fractures involves fixation with an intramedullary fixation device or dynamic hip screw. As these procedures are minimally invasive, open repositioning and fixation of a dislocated lesser trochanter are often not performed. Postoperative complications may affect around 20 % of patients with hip fractures [3]. However, vascular injury, which might be caused by the trauma itself, during surgery or during the postoperative course, rarely occurs. Only several of these cases have been published as a consequence of the latter cause [4–8].
In this article we describe the case of a 78-year-old male who developed a pseudoaneurysm of the profunda femoris artery during rehabilitation after intramedullary fixation for a multifragmentary pertrochanteric hip fracture (A2). Although a pseudoaneurysm is a rare complication after hip fractures, the development should be considered, in particular when symptoms such as pulsatile swelling or venous engorgement are presented. Early recognition could prevent an increase of the pseudoaneurysm diameter and therefore provide a higher therapy success rate.
Case report
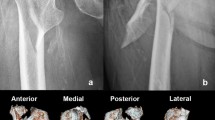
A 78-year-old male with an extensive history of cardiac problems, type II diabetes and renal dysfunction visited our emergency department after falling on his left hip. He was unable to bear any weight on it directly. During physical examination, his left leg was shorter and in external rotation. No swelling was objectified. A radiograph of his hips and pelvis showed a pertrochanteric femoral fracture on the left side with a dislocated lesser trochanter. It therefore includes a multifragmentary pertrochanteric hip fracture (A2 fracture). An intramedullary Gamma nail was placed the next day (Fig. 1). No complications occurred during the postoperative course, after which the patient was transferred to a rehabilitation clinic on the 10th postoperative day. At the time of discharge, the patient was feeling well, and although the wound was leaking exudate, it had no signs of infection. However, 4 weeks after the operation, the wound was still leaking exudate, and the wound culture showed an infection, which was successfully treated with antibiotics. The following months were without pain or complications.
Five months after surgery, however, the patients returned to our hospital with nonspecific pain in his left leg and the inability to stretch and walk. Although a swollen leg was seen for the first time since the operation, there was no erythema. Differential diagnoses were infection, deep venous thrombosis, arthrosis or dislocation of the Gamma nail. A radiograph of the patient’s left hip showed an unaltered position. Deep venous thrombosis was ruled out with duplex ultrasound; however, a large pseudoaneurysm of the profunda femoris artery (10 × 4 cm), pressing on the femoral vein (upper part of the profunda femoris artery), was seen. There was active flow in the pseudoaneurysm, including a partial thrombus (Fig. 2). Additionally, CT angiography was performed (Fig. 3).
The patient underwent thrombin treatment (2 ml), after which no circulation was seen in the pseudoaneurysm. However, after 4 days, the patient again underwent thrombin treatment (4 ml) as the pseudoaneurysm appeared not fully clotted. However, persistent flow was again presented in the aneurysm during duplex ultrasound. Therefore, an endovascular Wallgraft covered stent was placed through a 12-French sheath. The procedure was completed with technical success (Fig. 4). Due to preexistent kidney dysfunction, the patient was pre- and post-hydrated. Several hours after stent placement, the patient suddenly became dyspnoeic and was transferred to the coronary care unit under the suspicion of acute congestive heart failure. However, the patient ended up in the cardiopulmonary resuscitation setting, which eventually was discontinued. Unfortunately, an autopsy was not obtained.
A 78-year-old male during endovascular stent placement for his pseudoaneurysm. 1, Common femoral artery; 2, superficial femoral artery; 3, profunda femoris artery with pseudoaneurysm; 4, undilated stent in the profunda femoris artery with less flow in the pseudoaneurysm; 5, dilated stent in the profunda femoris artery without flow in the pseudoaneurysm
Discussion
With an incidence of 0.21 %, the formation of a pseudoaneurysm after a hip fracture is a rare complication [9]. While such vascular injury is mostly described because of trauma or during surgery, it is rarely reported as a consequence of dislocated bone fragments. The incidence of pseudoaneurysm due to the latter course is probably even lower after pertrochanteric fractures than hip fractures in general as these fractures often include a dislocated lesser trochanter and intertrochanteric fractures do not include this. Reconstruction images show that the lesser trochanter migrated cranially and lay against the pseudoaneurysm. Together with the clinical symptoms, these images suggest that pseudoaneurysm formation was a consequence of direct contact with a sharp part of the dislocated lesser trochanter. It could be hypothesized that the iliopsoas muscle dislocated this fragment cranially because of repeated hip flexion [4]. While this is the most likely cause, the possibility exists that the pseudoaneurysm was caused by the trauma or during surgery. Although we objectified the swelling for the first time, 5 months after surgery, the pain existed several weeks before presentation. It is therefore hypothesized that there was no sudden onset, but a gradually increasing swelling.
While a pseudoaneurysm is a rare complication of hip fractures, the complication is often not recognized on short notice because of nonspecific symptoms such as pain and edema, which show similarities with the general course after hip surgery. For this reason, the development of a pseudoaneurysm should always be considered, in particular when symptoms such as pulsatile swelling or venous engorgement are presented. The preferred diagnostics are arterial duplex ultrasound and CT angiography. There is no role for standard duplex ultrasound or CT angiography at the time of trauma in order to exclude a silent arterial injury due to the low incidence of vascular injury after hip fractures (0.21 %). In addition, considering the hypothesis that the swelling gradually increases, a pseudoaneurysm might not be found at the time of trauma. Performing these diagnostics is therefore always an individual choice. Depending on the location of the pseudoaneurysm, treatment is achieved through thrombin injections, open or endovascular repair. As the cause of the pseudoaneurysm is a dislocated lesser trochanter, resection of this fragment theoretically seems the definite therapy. However, this is an individual assessment, dependent on the location of the fragment and patient comorbidities.
References
Stevens JA, Olson S. Reducing falls and resulting hip fractures among older women. MMWR Recomm Rep. 2000;49:3–12.
Gillespie WJ. Extracts from "clinical evidence": hip fracture. BMJ. 2001;322(7292):968–75.
Carpintero P, Caeiro JR, Carpintero R, et al. Complications of hip fractures: A review. World J Orthop. 2014;5(4):402–11.
Helleman JN, Vos DI, Van der Laan L. Pseudoaneurysm of the deep femoral artery after pertrochanteric hip fracture: a case report. Vasc Dis Manag. 2011;2011:8E119–E120.
Singh S, Arora S, Thora A, Mohan R, Sural S, Dhal A. Pseudoaneurysm of profunda femoris artery following dynamic hip screw fixation for intertrochanteric femoral fracture. Chin J Traumatol. 2013;16(4):233–6.
Abraham E, Pankovich AM, Jansey F. False aneurysm of the profunda femoris artery resulting from intertrochanteric fracture. A case report. J Bone Joint Surg Am. 1975;57(6):871.
Lohmann H, Esenwein S, Geier B, Vogel T, Kleinert H. False aneurysm of the deep femoral artery due to pertrochanteric fracture of the hip with displaced fragment of the lesser trochanter. Z Orthop Unfall. 2009;147(1):23–5.
Sullivan MP, Schenker ML, Mehta S. Pertrochanteric hip fracture: a "routine" fracture with a potentially devastating vascular complication. Orthopedics. 2015;38(1):e75–9.
Karanikas I, Lazarides M, Arvanitis D, Papayanopoulos G, Exarchou E, Dayantas J. Iatrogenic arterial trauma associated with hip fracture surgery. Acta Chir Belg. 1993;93(6):284–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Authors’ disclosure
All authors declare that they have no conflict of interest. The corresponding author is not a recipient of a research scholarship.
Additional information
The article is not based on a previous communication to a society or meeting.
Rights and permissions
About this article
Cite this article
de Raaff, C.A.L., van Nieuwenhuizen, R.C. & van Dorp, T.A. Pseudoaneurysm after pertrochanteric femur fracture: a case report. Skeletal Radiol 45, 575–578 (2016). https://doi.org/10.1007/s00256-015-2315-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-015-2315-1