Abstract
Performing and optimizing MRI of the chest, abdomen and pelvis in neonates and young infants can be challenging. This is a result of several factors, including patient size, desire to avoid or minimize sedation/general anesthesia, and the relative rarity of these examinations. However, with proper preparation and protocol optimization, high-quality diagnostic images can be acquired that can aid in diagnosis and patient management. In addition, numerous special considerations arise when performing body MRI in neonates compared to older pediatric patients. This review article provides an update on the performance and optimization of MRI of the body in neonates and infants. Furthermore, the authors present common indications for neonatal body MRI and discuss the use of intravenous gadolinium-based contrast agents in this vulnerable patient population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Performing and optimizing MRI of the chest, abdomen and pelvis in neonates and young infants can be challenging. This is the result of a variety of factors, including patient size and the fact that MRI scanners and associated ancillary equipment are generally designed for much larger adult patients as well as the relative rarity of these examinations. When using optimized state-of-the-art pulse sequences and appropriate surface coils, however, high-quality diagnostic images can be acquired that can help in diagnosis and patient management. In addition, numerous special considerations arise when performing body MRI in neonates compared to older pediatric patients, such as how to safely transport the infant to and from the MRI scanner and keep the infant safe in the MRI environment, whether to image during natural sleep (so-called feed and swaddle) versus with sedation or general anesthesia, how to immobilize the infant, which surface coil to use, and how to manage power (heat) deposited into the infant during the imaging examination.
This review article provides an update on the performance and optimization of MRI of the body in neonates and young infants. Furthermore, we review common indications for neonatal body MRI and discuss the use of intravenous gadolinium-based contrast materials, including gadoxetate disodium (Eovist; Bayer HealthCare, Whippany, NJ), in this vulnerable patient population.
Special considerations when performing neonatal body magnetic resonance imaging
Patient transport
Neonates, and especially premature babies, are a vulnerable population that is particularly susceptible to physiological stress and instability. Thus, transportation to and from the MRI scanner likely places these infants at some risk outside the carefully controlled, vigilant and caring environment of the neonatal intensive care unit (NICU) [1, 2]. Transportation generally requires special equipment to monitor and support the baby (e.g., transport incubator) as well as dedicated personnel, such as a specialized transport team, nursing staff or physician staff. When performing neonatal body MRI, one goal should be to minimize the time and distance that infants are away from the NICU. In a study of 641 NICU patients and 1,197 intra-hospital transports, the majority of which were for imaging procedures, clinical complications occurred in 27.3% [1].
Feed and swaddle vs. sedation/general anesthesia and patient immobilization
There have been increasing efforts to decrease exposure to sedation and general anesthesia in very young children, including neonates. The feed-and-swaddle (or feed-and-wrap) method of imaging is increasingly described in the literature, with relatively high rates of success [3, 4]. With this method, the child is fed, immobilized and imaged during natural sleep. Thus, pulse sequences requiring breath-holding cannot be performed or must be modified to minimize motion artifacts. The feed-and-swaddle method avoids sedation/general anesthesia exposure and its potential adverse health effects and it lowers resource use and associated health care costs. However, if the infant does not soundly sleep, this method can result in a longer examination (potentially disrupting the MRI schedule) or even non-diagnostic imaging from patient motion. Kurugol et al. [4], using motion-robust (radial) and fast (compressed sensing acceleration) MRI techniques, were successful in performing dynamic contrast-enhanced MR urography in 17 of 18 infants without sedation or general anesthesia using a feed-and-wrap protocol.
Sedation and general anesthesia are still commonly used at dedicated pediatric institutions when performing body MRI in neonates and infants (although this is likely decreasing as use of the feed-and-swaddle method increases). Imaging under sedation or general anesthesia has advantages, including potentially improved image quality, faster imaging (especially if a feed-and-swaddle patient has difficulties sleeping), and improved diagnostic accuracy. Sedation/general anesthesia consumes more resources, however, with a resulting increase in health care costs. In a prospective investigation, Vanderby et al. [5] concluded that encounter costs for sedated and anesthetized patients were 3.2 and 9.6 higher, respectively, than costs for awake patients. Multiple or lengthy exposures to sedation and anesthetic medications in children younger than 3 years might also negatively impact the developing brain, based on recent United States Food and Drug Administration communications [6].
Patient immobilization is particularly critical for babies imaged using the feed-and-swaddle method. Immobilization decreases physical motion and associated image artifacts and can aid sleep. Several devices exist for neonate and infant immobilization in the MRI environment (e.g., MedVac Vacuum Immobilization Splints by Newmatic Medical, Caledonia, MI; Hugger by MRIequip, Nisswa, MN; Universal Octopaque octagon board by Octostop, Laval, Québec, Canada; BabyFix Cocoon by Pearl Technology AG, Schlieren, Switzerland) (Fig. 1). Importantly, any immobilization device must be confirmed as MRI safe. It also is possible to successfully immobilize neonates and infants in a surface coil (e.g., blanket-like coil) in combination with blankets, padding and tape, an approach that is commonly employed at our institution. Such devices have been shown to preserve image quality, minimize motion artifacts and shorten imaging times in premature neonates compared to a cohort imaged using sedation [7].
Clinical images of patient immobilization devices described as MRI safe. a MedVac Vacuum Immobilization System (Newmatic Medical, Caledonia, MI). b Hugger (MRIequip, Nisswa, MN). c Octagon board (Universal Octopaque; Octostop, Laval, Québec, Canada). d BabyFix Cocoon (Pearl Technology AG, Schlieren, Switzerland)
Patient monitoring and temperature maintenance
The neonatal population is susceptible to vital sign instability, particularly in response to stress. Thus, monitoring these babies is essential both during transportation to and from the MRI scanner and during the examination. Vital signs commonly monitored include heart rate, blood oxygen saturation, temperature and blood pressure. Monitors and leads must not only be MRI safe but also lack white noise emissions that can adversely impact MR image quality by producing artifacts.
It is important to recognize that neonates, and in particular premature babies, are less capable of maintaining their body temperature [2, 8]. This is likely caused by immaturity of the brain’s temperature regulatory system as well as neonates’ relatively larger body surface area compared to older children and adults. Decreases in body temperature can lead to vital sign instability. Thus, in the MRI environment, care should be taken to monitor and maintain a neonate’s body temperature. This can be accomplished through swaddling and the use of blankets, placement of a hat (cap) on the infant’s head and employing an MRI-compatible isolette (incubator) to provide a more hospitable environment during imaging. A study of brain and body MRI in 530 neonates using a dedicated MR-compatible incubator concluded that the incubator significantly increased the availability of MRI to newborns, particularly in premature and unstable newborns [9]. In a study by Don Paul et al. [2], only 43% of infants were normothermic upon return to the NICU following MRI, suggesting that MRI-related unintentional hypothermia is common unless proactively managed. Predictors of a post-MRI decrease in body temperature in neonates and infants include younger age, lower weight, lower pre-MRI temperature, use of propofol as the primary anesthetic, use of an advanced airway device, and being outside the NICU [8].
Magnetic field strength and specific absorption rate
Neonatal body MRI can be performed at both 1.5 tesla (T) and 3 T, each having advantages and disadvantages. Advantages of imaging at 3 T include increased signal versus noise, which can be used to improve image quality or shorten the examination. Faster imaging at 3 T has also been demonstrated to decrease the doses of medications used for sedation and general anesthesia [10]. Imaging at 3 T also has disadvantages, however, including increased artifacts from magnetic susceptibility, or local inhomogeneities in the magnetic field [11]. Imaging at 3 T can also increase the amount of energy deposited into a patient compared to 1.5 T (increased specific absorption rate, or SAR), although this is rarely clinically relevant in babies, who dissipate heat approximately 3–4 times faster than adults because of babies’ relatively greater body surface areas [12]. Malik et al. [12] modeled SAR in neonates and adults at 1.5 T and 3 T, concluding that SAR is lower in neonates than in adults under equivalent radiofrequency (RF) conditions and that MRI scanner SAR calculators designed for adults might overestimate power deposition, thus creating an additional safety margin.
Coil selection
The choice of surface coil when performing neonatal body MRI can substantially impact image quality, particularly signal versus noise [13]. Ideally, the size of the coil should match the size of the area of interest, and the coil should be located close to the infant to maximize sensitivity [13]. Smaller coils, in general, are associated with less image noise and might allow smaller fields of view. Furthermore, increasing the number of coil elements can increase sensitivity to RF signal while shortening examination time because of the increased image acquisition acceleration. Dedicated surface coils for neonatal body MRI can be original manufacturer equipment sold by the MRI scanner manufacturer, although aftermarket dedicated neonatal coils are also available for purchase. Multi-element “flex” and blanket-like coils can also be useful for imaging neonates and infants (Fig. 2). The torso of neonates and infants can be imaged in a variety of adult coils as well, such as extremity and head and neck coils, assuming SAR safety limits are appropriately calculated and not exceeded [14].
Clinical images of surface coils for neonatal body MRI. a Dedicated neonatal 8-channel coil designed for torso imaging (Philips Healthcare, Best, the Netherlands). b Lightweight blanket-like 24-channel coil (Siemens Medical Solutions USA, Malvern, PA). c Lightweight blanket-like 20-channel coil (GE Healthcare, Waukesha, WI). d Aftermarket Infant Cocoon coil, which allows body imaging in neonates and young infants using various manufacturers’ scanners (SREE Medical Systems, Cleveland, OH)
Performance of neonatal body magnetic resonance imaging protocols
When constructing neonatal body MRI protocols, there are several guiding principles to consider. First, the group of assembled pulse sequences should be capable of answering the clinical question at hand. Second, the protocol length should be as short as reasonably possible to minimize the amount of time the infant is in the MRI environment and away from the NICU. Third, the chosen pulse sequences ideally should be motion-robust and avoid the need for breath-holding, thus eliminating the need for general anesthesia and advanced airway devices. Fortunately, while most state-of-the-art pulse sequences are created for and initially investigated in adults, they can generally be translated to the pediatric population with appropriate parameter optimization.
T2-weighted imaging
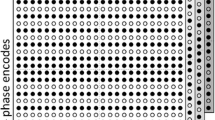
Three primary T2-weighted pulse sequences are used for body MRI in the neonate: (1) single-shot fast spin echo (SSFSE) or half-Fourier acquisition single-shot turbo spin echo (HASTE), (2) two-dimensional (2-D) multi-shot fast spin echo (FSE) and (3) three-dimensional (3-D) FSE (Fig. 3). All of these sequences can be used in conjunction with respiratory triggering or navigator pulse gating to minimize breathing-related artifacts, although respiratory detection using a bellows or belt can be difficult because of the inability to detect the slight excursions associated with breathing in the neonate. Two-dimensional FSE imaging can also be performed by acquiring numerous rotating blades made of multiple Cartesian phase-encoded lines, so-called periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER; GE Healthcare, Waukesha, WI), also known as BLADE (Siemens Medical Solutions USA, Malvern, PA) or MultiVane (Philips Healthcare, Best, the Netherlands) [15]. This variation of k-space filling oversamples the center of k-space, resulting in high signal-to-noise and contrast-to-noise ratios as well as a considerable reduction in motion sensitivity/artifact. All three of these T2-weighted techniques are generally time-consuming and can be accelerated using conventional parallel imaging techniques or more recently using pseudorandom undersampling of k-space (i.e. compressed sensing) [16, 17]. T2-weighted or fluid-sensitive images are generally used to detect a wide variety of pathological abnormalities as well as to characterize tissue. At least one T2-weighted sequence should also be obtained with fat suppression, commonly by employing frequency-selective chemical saturation, inversion recovery pulse or Dixon-based technique [18, 19].
T2-W sequences in a 10-day-old boy with an unusual form of cystic biliary atresia. a–c Coronal single-shot fast spin-echo (a), axial fat-suppressed T2-weighted MultiVane (b) and three-dimensional fast spin-echo maximum-intensity projection (c) images show a large, complex cystic structure centered in the region of the porta hepatis
T1-weighted imaging
Multiple T1-weighted pulse sequences can also be used for neonatal body MRI (Fig. 4). T1-weighted FSE sequences are free-breathing and hence susceptible to respiratory motion artifacts that can be mitigated either by obtaining multiple signal averages or by using PROPELLER technique [15]. T1-weighted gradient recalled echo (GRE) images can be obtained using either 2-D or 3-D filling of k-space. Three-dimensional GRE sequences are highly susceptible to motion artifacts, including those from breathing, however, and generally require the use of multiple signal averages or general anesthesia with breath-holding.
T1-W sequences in a 14-day-old boy with pathology-proven inflammatory myofibroblastic tumor of the liver. a–c Axial two-dimensional T1-weighted fast spin-echo (a), breath-held axial post-contrast three-dimensional (3-D) T1-weighted modified Dixon (mDixon) (water image) (b) and free-breathing axial post-contrast 3-D T1-weighted mDixon stack-of-stars (3-D VANE) (water image) (c) images show a solid infiltrative liver mass located just to the right of the porta hepatis. The axial fast spin-echo image (a) shows respiratory motion artifacts despite the use of multiple signal averages. The mass demonstrated a centripetal enhancement pattern over time, likely because of its fibrous nature
Recently, free-breathing motion-robust T1-W GRE sequences have become clinically available that fill k-space using a stack-of-stars or radial trajectory (e.g., StarVIBE, or radial volumetric interpolated breath-hold examination, Siemens Medical Solutions USA; 3-D VANE, Philips Healthcare; and LAVA Star, or radial liver acquisition with volume acceleration, GE Healthcare) [20,21,22]. These radial 3-D GRE sequences also might allow for the collection of data from multiple echo times, enabling the creation of multiple image contrasts through Dixon methodology (e.g., in-phase, opposed-phase, water-only and fat-only images). Like T2-weighted imaging, all T1-weighted images can be acquired without or with fat suppression. However, compared to T2-weighted images, unenhanced T1-weighted images are generally less helpful for detecting pathological abnormalities, but instead aid in tissue characterization. Furthermore, these sequences are ubiquitously used as the foundation for contrast-enhanced MRI, which aids in lesion detection and characterization as well as in the assessment of tissue perfusion and vasculature.
Dynamic post-contrast imaging
Dynamic post-contrast imaging of the body, such as multiphase post-contrast imaging used to characterize liver masses, has commonly employed a 3-D GRE pulse sequence (e.g., VIBE, THRIVE [T1-weighted high-resolution isotropic volume examination] or LAVA) and multiple breath-holds. However, again, very recently, free-breathing T1-weighted sequences have become clinically available that allow for dynamic post-contrast imaging without breath-holds (e.g., GRASP, or golden-angle radial sparse parallel MRI, Siemens Medical Solutions USA; 4-D FreeBreathing, Philips Healthcare; DISCO star, or differential subsampling with Cartesian ordering, and Star, GE Healthcare) [22, 23]. These sequences employ a radial trajectory for filling k-space as well as combinations of view sharing, parallel imaging and compressed sensing with advanced iterative image reconstruction. Dynamic contrast-enhanced imaging of the vasculature can also be performed in neonates using free-breathing time-resolved MR angiography methods, such as TWIST (time-resolved angiography with interleaved stochastic trajectories; Siemens Medical Solutions USA), TRICKS (time-resolved imaging of contrast kinetics; GE Healthcare) and 4-D TRAK (time-resolved MR angiography with keyhole; Philips Healthcare) [24]. These sequences use parallel imaging and view-sharing and are particularly useful for evaluating vascular malformations and vascular congenital anomalies because they allow for evaluation of both anatomy and hemodynamics.
Other important pulse sequences
A few additional pulse sequences can be particularly helpful when imaging neonates. First, a multi-echo GRE sequence should be available to assess for the presence of iron overload. MRI detection of iron in the liver, pancreas and thyroid is critical to the diagnosis of neonatal hemochromatosis [25]. Second, diffusion-weighted imaging, while not necessarily essential, can be useful for lesion detection and characterization (Fig. 5) [26]. Finally, non-contrast MRI methods for evaluating the vasculature are becoming increasingly available. For example, a recently described 3-D Dixon-based GRE sequence with inversion recovery and a T2 preparation pulse provides extremely detailed imaging of the arterial and venous vasculature of the chest, abdomen and pelvis while also allowing for high-quality multi-planar reformations and 3-D reconstructions (Fig. 6) [27, 28].
The addition of diffusion-weighted sequences in a 27-day-old boy with known congenital hemangioma of the liver. a Axial fat-suppressed T2-weighted MultiVane image shows a large lobulated hyperintense mass replacing most of the liver. Large flow voids are present within the mass. b Axial diffusion-weighted image (b value = 800 s/mm2) shows that the liver mass has mildly increased peripheral signal intensity and mildly decreased central signal intensity. The spleen (long arrow) and left adrenal gland (short arrow) are highlighted. c Apparent diffusion coefficient parametric map shows only mild impeded diffusion of water involving the periphery of the mass, characterized as intermediate signal intensity. The spleen (long arrow) and left adrenal gland (short arrow) appear very dark, consistent with much greater restricted diffusion of water molecules
Non-contrast vascular MRI in a 29-day-old boy with ultrashort gut and cholestasis being considered for multivisceral transplant. Three-dimensional mDixon inversion recovery sequence with T2 preparation maximum-intensity projection image confirms that major vascular structures in the neck, chest, abdomen and pelvis are patent and available for vascular access
Common indications for neonatal body magnetic resonance imaging
The performance of body MRI in neonates is actually fairly uncommon, for several reasons. First, radiography and US can answer many imaging-related questions in very young children. Second, evaluation by MRI can often wait until the child is older and outside the neonatal period. Third, numerous neonatal (and often congenital) abnormalities are not clinically present until later in life. Finally, in some cases, although it subjects the neonate to ionizing radiation, CT is the more appropriate imaging test to provide fast, high-quality imaging without sedation or general anesthesia to facilitate immediate medical decision-making.
A review of neonatal imaging performed at Cincinnati Children’s Hospital Medical Center between January 2019 and December 2020 showed on average ~2–4 clinical neonatal body MRI examinations each month. Common indications for imaging the chest included assessment of vascular malformations and vascular malformation syndromes (e.g., CLOVES syndrome, or congenital lipomatous overgrowth, vascular malformations, epidermal nevi and scoliosis/skeletal/spinal anomalies), congenital vascular anomalies, masses and mass-like lesions, congenital lung lesions, and more recently, bronchopulmonary dysplasia. Common indications for imaging the abdomen and pelvis included assessment of congenital masses of the liver, adrenal glands and kidneys; vascular malformations and vascular malformation syndromes; congenital vascular anomalies; mass versus hematoma (e.g., adrenal gland, liver); pancreatobiliary anomalies; congenital cystic lesions; and complex renal and urinary tract anomalies.
Intravenous gadolinium chelate considerations
The decision to administer an intravenous gadolinium chelate, or a gadolinium-based contrast agent (GBCA), during a neonatal body MRI examination should be made on a patient-by-patient basis after considering the available medical and surgical history and the clinical indication for imaging. Both the risks and benefits of administering these contrast agents should be considered. Potential risks of exogenous GBCA exposure include allergic-like reactions, physiological adverse reactions, gadolinium retention in the body and nephrogenic systemic fibrosis (NSF). Based on the literature, allergic-like reactions to GBCAs are very rare in young children, including neonates [29, 30]. Fortunately, most neonatal body MRI examinations are performed under anesthesiologist or nurse supervision with uninterrupted monitoring, so that if they occur, treatment is timely and efficacious. While there is particular concern about gadolinium retention in the body in children, especially neonates and infants because of their longer life expectancies and hence increased potential for additional GBCA exposures, no adverse health effects from retained gadolinium in the body (e.g., brain, bone) have been proved to date. As of 2012, NSF was only very rarely reported in children, with no instances in children younger than 6 years [31]. The recent change to the American College of Radiology (ACR) Group II GBCAs (i.e. the increased use of macrocyclic GBCAs and gadobenate dimeglumine) has essentially eliminated NSF, including in adults with chronic kidney disease who had been considered high-risk for developing NSF [32].
Gadolinium-based contrast agent administration has many potential benefits in neonatal body MRI. First, GBCAs can highlight lesions that otherwise go undetected on non-contrast MRI acquisitions. Second, it is likely that these contrast agents improve both the diagnostic performance of MRI and reader confidence. Finally, while much more difficult to prove (particularly in the neonatal population), it is conceivable that GBCAs improve patient outcomes.
It is generally advisable to take a cautious approach to the administration of GBCAs in neonates and young children. This is in part because only a very tiny fraction of the hundreds of millions of doses of GBCAs administered throughout the world to date have been injected in neonates, so the data in this population are limited. However, based on the available evidence, these agents can be safely used when clinically indicated. In fact, all three currently available macrocyclic GBCAs are approved for use in infants and term neonates based on their package inserts. When performing neonatal body MRI, an ACR Group II GBCA should be used because of the positive safety profiles of these agents, unless the examination is being performed for a hepatobiliary indication. In this setting, gadoxetate disodium (Eovist; Bayer HealthCare Pharmaceuticals, Whippany, NJ) might prove useful. While the package insert for gadoxetate disodium states that adequate, well-controlled studies have not yet been conducted in the pediatric population, no safety issues were noted in an observation study of 52 pediatric patients (>2 months to <18 years old) receiving this contrast agent [33]. Like conventional GBCAs, there is a general paucity of data regarding the use of gadoxetate disodium in neonates, and its use should be limited to when it is truly indicated. Renal immaturity from extremely young age alone is not a specific contraindication to GBCA administration.
Conclusion
High-quality neonatal body MRI is possible in neonates and young infants. However, careful attention to the numerous special considerations described here is required to image both safely and effectively, particularly when compared to older children. Importantly, completely free-breathing body MRI protocols are now available, likely decreasing the need for breath-holding as well as sedation and general anesthesia. Intravenous GBCAs can be administered safely in the neonatal population but their use should be reserved for those cases in which the potential information gained will importantly and uniquely inform patient care.
References
Vieira AL, dos Santos AM, Okuyama MK et al (2011) Factors associated with clinical complications during intra-hospital transports in a neonatal unit in Brazil. J Trop Pediatr 57:368–374
Don Paul JM, Perkins EJ, Pereira-Fantini PM et al (2018) Surgery and magnetic resonance imaging increase the risk of hypothermia in infants. J Paediatr Child Health 54:426–431
Windram J, Grosse-Wortmann L, Shariat M et al (2012) Cardiovascular MRI without sedation or general anesthesia using a feed-and-sleep technique in neonates and infants. Pediatr Radiol 42:183–187
Kurugol S, Seager CM, Thaker H et al (2020) Feed and wrap magnetic resonance urography provides anatomic and functional imaging in infants without anesthesia. J Pediatr Urol 16:116–120
Vanderby SA, Babyn PS, Carter MW et al (2010) Effect of anesthesia and sedation on pediatric MR imaging patient flow. Radiology 256:229–237
United States Food and Drug Administration (2017) FDA drug safety communication: FDA approves label changes for use of general anesthetic and sedation drugs in young children. FDA website. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-approves-label-changes-use-general-anesthetic-and-sedation-drugs. Accessed 23 Mar 2021
Yamamura K, Takatsu Y, Miyati T, Inatomi T (2018) Brain magnetic resonance imaging using a customized vacuum shape-keeping immobilizer without sedation in preterm infants. Magn Reson Imaging 54:171–175
Dalal PG, Porath J, Parekh U et al (2016) A quality improvement project to reduce hypothermia in infants undergoing MRI scanning. Pediatr Radiol 46:1187–1198
Bekiesińska-Figatowska M, Rutkowska M, Stankiewicz J et al (2019) Neonatal brain and body imaging in the MR-compatible incubator. Adv Clin Exp Med 28:945–954
Machado-Rivas F, Leitman E, Jaimes C et al (2021) Predictors of anesthetic exposure in pediatric MRI. AJR Am J Roentgenol 216:799–805
Morelli JN, Runge VM, Ai F et al (2011) An image-based approach to understanding the physics of MR artifacts. Radiographics 31:849–866
Malik SJ, Beqiri A, Price AN et al (2015) Specific absorption rate in neonates undergoing magnetic resonance procedures at 1.5 T and 3 T. NMR Biomed 28:344–352
Hillenbrand CM, Reykowski A (2012) MR imaging of the newborn: a technical perspective. Magn Reson Imaging Clin N Am 20:63–79
Helle M, Jerosch-Herold M, Voges I et al (2011) Improved MRI of the neonatal heart: feasibility study using a knee coil. Pediatr Radiol 41:1429–1432
Pipe JG (1999) Motion correction with PROPELLER MRI: application to head motion and free-breathing cardiac imaging. Magn Reson Med 42:963–969
Chen F, Taviani V, Tamir JI et al (2018) Self-calibrating wave-encoded variable-density single-shot fast spin echo imaging. J Magn Reson Imaging 47:954–966
Serai SD, Hu HH, Ahmad R et al (2020) Newly developed methods for reducing motion artifacts in pediatric abdominal MRI: tips and pearls. AJR Am J Roentgenol 214:1042–1053
Kishida Y, Koyama H, Seki S et al (2018) Comparison of fat suppression capability for chest MR imaging with Dixon, SPAIR and STIR techniques at 3 tesla MR system. Magn Reson Imaging 47:89–96
Delfaut EM, Beltran J, Johnson G et al (1999) Fat suppression in MR imaging: techniques and pitfalls. Radiographics 19:373–382
Chandarana H, Block TK, Rosenkrantz AB et al (2011) Free-breathing radial 3D fat-suppressed T1-weighted gradient echo sequence: a viable alternative for contrast-enhanced liver imaging in patients unable to suspend respiration. Investig Radiol 46:648–653
Ichikawa S, Motosugi U, Kromrey ML et al (2020) Utility of stack-of-stars acquisition for hepatobiliary phase imaging without breath-holding. Magn Reson Med Sci 19:99–107
Kim JR, Yoon HM, Cho YA et al (2020) Free-breathing contrast-enhanced upper abdominal MRI in children: comparison between Cartesian acquisition and stack-of-stars acquisition with two different fat-suppression techniques. Acta Radiol 62:541–550
Chandarana H, Feng L, Block TK et al (2013) Free-breathing contrast-enhanced multiphase MRI of the liver using a combination of compressed sensing, parallel imaging, and golden-angle radial sampling. Investig Radiol 48:10–16
Kim JS, Chandler A, Borzykowski R et al (2012) Maximizing time-resolved MRA for differentiation of hemangiomas, vascular malformations and vascularized tumors. Pediatr Radiol 42:775–784
Alenezi K, Kamath BM, Siddiqui I et al (2018) Magnetic resonance imaging findings in neonatal hemochromatosis. J Pediatr Gastroenterol Nutr 66:581–587
Neubauer H, Li M, Müller VR et al (2017) Diagnostic value of diffusion-weighted MRI for tumor characterization, differentiation and monitoring in pediatric patients with neuroblastic tumors. Rofo 189:640–650
Dillman JR, Trout AT, Merrow AC et al (2019) Non-contrast three-dimensional gradient recalled echo Dixon-based magnetic resonance angiography/venography in children. Pediatr Radiol 49:407–414
Yoneyama M, Zhang S, Hu HH et al (2019) Free-breathing non-contrast-enhanced flow-independent MR angiography using magnetization-prepared 3D non-balanced dual-echo Dixon method: a feasibility study at 3 tesla. Magn Reson Imaging 63:137–146
Forbes-Amrhein MM, Dillman JR, Trout AT et al (2018) Frequency and severity of acute allergic-like reactions to intravenously administered gadolinium-based contrast media in children. Investig Radiol 53:313–318
Dillman JR, Ellis JH, Cohan RH et al (2007) Frequency and severity of acute allergic-like reactions to gadolinium-containing i.v. contrast media in children and adults. AJR Am J Roentgenol 189:1533–1538
Nardone B, Saddleton E, Laumann AE et al (2014) Pediatric nephrogenic systemic fibrosis is rarely reported: a RADAR report. Pediatr Radiol 44:173–180
Woolen SA, Shankar PR, Gagnier JJ et al (2020) Risk of nephrogenic systemic fibrosis in patients with stage 4 or 5 chronic kidney disease receiving a group II gadolinium-based contrast agent: a systematic review and meta-analysis. JAMA Intern Med 180:223–230
United States Food and Drug Administration (2008) Highlights of prescribing information: Eovist. Online document. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/022090s011lbl.pdf. Accessed 23 Mar 2021
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dillman, J.R., Tkach, J.A. Neonatal body magnetic resonance imaging: preparation, performance and optimization. Pediatr Radiol 52, 676–684 (2022). https://doi.org/10.1007/s00247-021-05118-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-021-05118-4