Abstract
Background
The ratio of the transverse diameter of the main pulmonary artery (MPA) to ascending aorta as determined at multi-detector CT is a tool that can be used to assess the pulmonary arterial size in cases of pulmonary arterial hypertension in children.
Objective
To establish a ratio of MPA to ascending aorta diameter using multi-detector CT imaging suggestive of pulmonary arterial hypertension in children. We hypothesize that a defined ratio of MPA to ascending aorta is identifiable on multi-detector CT and that higher ratios can be used to reliably diagnose the presence of pulmonary arterial hypertension in children.
Materials and methods
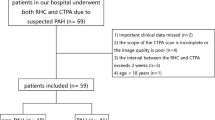
We calculated the multi-detector CT ratio of MPA to ascending aorta diameter in 44 children with documented pulmonary arterial hypertension by right heart catheterization and in 44 age- and gender-matched control children with no predisposing factors for pulmonary arterial hypertension. We compared this multi-detector-CT-determined ratio with the MPA pressure in the study group, as well as with the ratio of MPA to ascending aorta in the control group. A threshold ratio value was calculated to accurately identify children with pulmonary arterial hypertension.
Results
Children with documented primary pulmonary arterial hypertension have a significantly higher ratio of MPA to ascending aorta (1.46) than children without pulmonary arterial hypertension (1.11). A ratio of 1.3 carries a positive likelihood of 34 and a positive predictive value of 97% for the diagnosis of pulmonary arterial hypertension.
Conclusion
The pulmonary arteries were larger in children with pulmonary arterial hypertension than in a control group of normal children. A CT-measured ratio of MPA to ascending aorta of 1.3 should raise the suspicion of pulmonary arterial hypertension in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary arterial hypertension is defined as a mean pulmonary artery pressure of >25 mmHg as measured by right heart catheterization [1]. Early diagnosis of this disease is especially important in children because advanced pulmonary arterial hypertension is associated with a poorer long-term prognosis [2].
Multi-detector CT of the chest is commonly performed in children with pulmonary arterial hypertension and in children at risk of pulmonary arterial hypertension. It is also commonly performed in children in whom pulmonary arterial hypertension is not suspected but who have other nonspecific respiratory or cardiac symptoms. Most investigators have focused on the dilatation of the MPA in absolute terms, or in a ratio as compared with the ascending aorta, to diagnose pulmonary arterial hypertension. Dilatation of the pulmonary arteries has been established as a reliable criterion for the diagnosis of pulmonary arterial hypertension in adults [3] and as a common finding in children with idiopathic pulmonary arterial hypertension [4].
Multi-detector CT has been shown to correlate well with the gold standard of right heart catheterization, demonstrating good inter-observer agreement [3, 5–7].
The ratio of MPA to ascending aorta is a tool to assess the dilatation of the pulmonary arterial segments, because pulmonary arterial hypertension causes selective enlargement of the MPA and its major branches but not of the ascending aorta. It is calculated by dividing the transverse diameter of the MPA by the transverse diameter of the ascending aorta (Fig. 1).
In a previous study [8] we defined a set of normal values for the ratio of MPA to ascending aorta as determined at multi-detector CT in a population of 200 normal children with no predisposing factors for pulmonary arterial hypertension.
That study showed that ratio of MPA to ascending aorta in children (younger than 18 years) is not equal to the accepted value of 1 for adults (P < 0.0001). The average ratio of MPA to ascending aorta was 1.085, with a significant difference among age groups (1.12 for age 0–6 years, 1.05 for age 7–18 years). There was no difference between boys and girls (P > 0.05).
The hypothesis of this subsequent study is that children with primary pulmonary arterial hypertension have a larger ratio of MPA to ascending aorta than children without pulmonary arterial hypertension and a determined ratio value can be useful to identify them. The aim of this article is to propose a ratio of MPA to ascending aorta diameter as determined at multi-detector CT that is suggestive of pulmonary arterial hypertension in children and carries a high positive predictive value.
Materials and methods
The research ethics committee of the Hospital for Sick Children approved this study.
The study and control groups are outlined in Tables 1 and 2. We identified 44 children (median age 41 months, age range 1–204 months) with pulmonary arterial hypertension as determined by right heart catheterization. All 44 had undergone a thoracic multi-detector CT examination with intravenous contrast agent, as well as a right-side heart catheterization, within 9 months of each other (median time 17 days, standard deviation [SD] 69 days), between February 2000 and April 2013. The group consisted of 12 boys (median age 25 months, range 1–192 months) and 32 girls (median age 63 months, range 1–204 months). The etiology of pulmonary arterial hypertension in this cohort of children is detailed in Table 1.
All right-side heart catheterizations were performed by the same team using standard techniques, with mean pulmonary artery pressure obtained at rest in all children.
The control group consisted of 44 age- and gender-matched children who underwent a thoracic multi-detector CT between January 2010 and December 2013 and had no predisposing factors for pulmonary hypertension (Table 2). These children were part of our previous study to assess the ratio of MPA to ascending aorta in healthy children using multi-detector CT [8].
Exclusion criteria for the study group consisted of children with primary malformations of the wall of the aorta or MPA (truncus arteriosus and aortic coarctation). Exclusion criteria for the control group consisted of children with entities known to predispose to pulmonary arterial hypertension, including congenital cardiovascular disease, interstitial lung disease, thoracic radiation therapy, chemotherapy, mediastinal mass and bone marrow transplantation.
Computed tomography protocol
The CT images were part of the clinical assessment of the children. The median interval from CT to right heart catheterization was 17 days (SD 69 days, range 0–257 days).
The CT studies were performed with a 64-slice GE Discovery CT750HD (GE Healthcare, Milwaukee, WI). All children were imaged in the supine position, with breath-holding at full inspiration when they were able to cooperate. No cardiac gating was used.
CT parameters were calculated based on weight, ranging between 80 kilovoltage peak (kVp) and120 kVp (80 kVp for 0–9 kg, 100 kVp for 9–23 kg, 120 kVp for >23 kg).
For children weighing more than 15 kg, milliampere (mA) was selected using a dose-modulated technique. The institutional CT dose index ranges between 2.6 milligrays (mGy) and 2.8 mGy for ages 0–6 months, 2.8–4 mGy for 6–18 months, 3.2–4.5 mGy for 18 months to 5 years, 4–6 mGy for 5–13 years and 3.5–6.5 mGy for 13–18 years, based on a 32-cm phantom.
Standard acquisition parameters included a field of view that varied depending on patient size, slice acquisition of 0.625 mm with 2.5- and 5-mm reconstructions, pitch of 1.375 (0.969 for pulmonary embolism) and rotation time of 0.5 seconds (s).
Intravenous contrast administration consisted of iodixanol (Vispaque 320; GE Healthcare, Mississaugua, Ontario) administered via pump injection through a 22- or 24-gauge intravenous catheter placed in a peripheral vein with a 1–2 cc/s injection rate, depending on the intravenous catheter size and cooperation of the child. Average delay from injection was approximately 35 s. Scans for pulmonary embolism were started using SmartPrep technique with visual threshold determination.
CT scans were reconstructed at section widths of 5-mm axial for evaluation at the mediastinal window (2.5 mm in children younger than 2 years), 2-mm coronal and sagittal mediastinal window on a standard algorithm, and 5-mm axial lung window on a lung algorithm (2.5 mm in children younger than 2 years).
Image analysis
Two investigators (a pediatric radiologist with 25 years of experience with chest CT and a pediatric radiology fellow with 2 years of fellowship experience) measured independently and on different dates the diameters of the ascending aorta and MPA for the determination of MPA-to-ascending-aorta ratio. They were blinded to each other’s measurements and to the reports of right heart catheterization. The widest short-axis diameter of the ascending aorta and MPA at the level of the bifurcation (Figs. 1 and 2) was obtained on axial 5-mm slices with up to 100% magnification and on 2.5-mm slices for children younger than 2 years (mediastinal window settings were used with a width of 400 Hounsfield units [HU] and a level of 40 HU). The measurements were obtained in the axial plane and included only the luminal diameter, excluding the wall of the vessel. The angle of the measurements of the ascending aorta and MPA were drawn perpendicular to the long axis of the vessel at that level. The diameter was measured only in the axial plane (not as an area) without multiplanar reconstructions in order to simplify reproducibility.
Main pulmonary artery diameter in a 16-year-old girl with primary pulmonary arterial hypertension. Axial multi-detector contrast-enhanced CT of the chest shows enlargement of the main pulmonary artery (MPA), with a ratio of MPA to ascending aorta diameter of 1.92. Right heart catheterization demonstrated an increased MPA mean pressure of 58 mmHg
Statistical analysis
Descriptive statistics such as mean, median, standard deviation and range are used to describe the sample. Differences between patient groups were evaluated with non-parametric paired tests to account for data matching. We used Pearson correlation coefficients to evaluate correlation of ratio of MPA to ascending aorta with age, gender and pulmonary pressure. Interobserver agreement was assessed with intraclass correlation coefficients (ICC). A ratio of MPA to ascending aorta with a discriminatory value suggestive of pulmonary arterial hypertension and its ROC area under the curve were calculated. A P-value of less than 0.05 was considered significant. SAS 9.4 software (SAS Institute, Cary, NC) was used for statistical analysis.
Results
Table 3 details the results. There was excellent reader agreement for the measurements of the transverse diameters of the pulmonary artery and ascending aorta between readers. The intraclass correlation coefficient (ICC; 95% confidence interval [CI]) was 1.0 (0.99, 1.00) for the MPA measurement and 0.99 (0.99, 1.00) for the ascending aorta.
The mean transverse diameter of the MPA of children with pulmonary arterial hypertension was 22.8 mm (22.9 mm in boys and 22.8 mm in girls) and the median 22.5 mm. The mean MPA diameter of the control group was 17.1 mm and the median 16.8 mm; here the mean MPA diameter was 17.2 mm in boys and 17.1 mm in girls, with no statistical difference for gender (P = 0.9387).
The average ratio of MPA to ascending aorta was 1.46 in children with pulmonary arterial hypertension. There was no statistical difference between boys (1.45) and girls (1.46) (P = 0.8889). The ratio of MPA to ascending aorta was 1.11 in the control group. There was no statistical difference between boys (1.13) and girls (1.10) (P = 0.6149). The difference in ratio of MPA to ascending aorta between normal children and children with pulmonary arterial hypertension was statistically significant across all age groups (Table 3). There was no statistically significant difference between the ratio of MPA to ascending aorta (P = 0.11) or MPA diameter (P = 0.21) between the groups of children with pulmonary arterial hypertension caused by congenital heart disease and those with idiopathic pulmonary hypertension. However, the mean MPA pressure was significantly higher in children with primary pulmonary arterial hypertension than in children with congenital heart disease (P = 0.007) (Table 1).
Multiple values between 1.1 and 1.4 were tested as a discriminating CT-measured ratio of MPA to ascending aorta in order to identify children with pulmonary arterial hypertension with a high positive predictive value (PPV) to avoid a high number of false-positives. A discriminating CT ratio of MPA to ascending aorta of 1.3 carries a positive likelihood ratio of 34 (PPV of 97%) and specificity of 98%. The receiver operating characteristic (ROC) area under the curve for the discriminatory value of 1.3 is 0.94 (Fig. 3).
A discriminating CT-measured ratio of main pulmonary artery to ascending aorta of 1.3 carries a positive predictive value of 97% in the group of children with pulmonary arterial hypertension. The receiver operating characteristic (ROC) area under the curve for the discriminatory value of 1.3 is 0.94
Discussion
This study has shown that multi-detector CT may provide the first indication of a potential diagnosis of pulmonary arterial hypertension in children. It is possible to discriminate children with pulmonary arterial hypertension from children without it using the MPA diameter and the multi-detector-CT-determined ratio of MPA to ascending aorta.
In this study, the MPA diameter and the ratio of MPA to ascending aorta diameter were significantly larger in a group of 44 children with primary pulmonary hypertension than in a control group of children who underwent a chest CT for different reasons and had no risk factors of pulmonary arterial hypertension.
This CT-derived ratio has shown excellent interobserver agreement as seen on previous studies [3] and it is probably easier to use in daily practice than tables of the transverse diameter of the main pulmonary artery stratified by age.
The largest adult population cohort in which pulmonary artery dimensions were assessed by CT was described in the Framingham Heart Study of 3,171 adults (mean age 51 years, 51% men), of whom 706 were identified as asymptomatic without any cardiopulmonary risk factors. The MPA size in this reference subset was 24.7 mm (SD 2.7) and the ratio of MPA to ascending aorta for adults was therefore determined to equal 0.80 (SD 0.09) [7].
In children, Akay et al. [9] measured the mean pulmonary artery size in a cohort of 133 children who had no history of cardiac or pulmonary disease. The authors concluded that there is a significant relationship between the ratio of MPA to ascending aorta and the CT diameter of the major thoracic vessels and the age of the patient and they found no difference between genders. In our previous and current studies, we have identified similar findings.
It has been suggested that the ratio of MPA to ascending aorta is a more accurate marker of MPA pressure because confounding variables, such as patient size, influence the size of the pulmonary artery and ascending aorta equally, enabling a form of internal standardization [3].
In adults, a ratio of MPA to ascending aorta of more than 1 is suspicious for pulmonary arterial hypertension with a PPV 96% and a specificity of 92% [3]. In a previous study of 200 children with no predisposing factors for pulmonary arterial hypertension, we demonstrated that the ratio of MPA to ascending aorta is not equal to 1 in children. The value of 1 used in adults should not, therefore, be used for children. The previous study showed that a ratio of MPA to ascending aorta of 1.085 is more appropriate for normal children [8]. In the control group of the present study, the mean ratio of MPA to ascending aorta is 1.11, slightly higher than in the previous study, probably related to the younger average age of the children in the current study.
A discriminating CT-measured ratio of MPA to ascending aorta of 1.3 carries a positive likelihood ratio of 34 (PPV of 97%) in this group of children with pulmonary arterial hypertension. This threshold could prevent the possibility of false-positives that sometimes result in negative catheterizations.
We do not advocate using CT to screen children for pulmonary arterial hypertension. We suggest using this ratio to alert clinicians to the possibility so that further investigations, such as echocardiography or right heart catheterization, can be clinically pursued if indicated.
Limitations to this study include its retrospective nature, small sample size, heterogeneous study population, absence of right heart catheterization in the control group and relative time interval between CT and right catheterization in some children. The determination of the time interval after which the enlargement of the pulmonary arteries is appreciable on multi-detector CT is beyond the scope of this study. Therefore, this finding might not be applicable in children suspected of having acute pulmonary arterial hypertension. The lack of cardiac gating could be considered as another potential limitation. However, we did not exclude any study because of motion artifact that precluded the measurement of the ratio of MPA to ascending aorta.
Conclusion
Children with pulmonary arterial hypertension have a larger main pulmonary artery than normal children. We have confirmed the suspicion that a dilated MPA is useful for identifying pulmonary arterial hypertension in these children. A ratio of MPA to ascending aorta that is equal to or more than 1.3 suggests pulmonary arterial hypertension and should alert the radiologist and the referring physicians to the need for further investigation.
References
Hoeper MM (2009) Definition, classification, and epidemiology of pulmonary arterial hypertension. Semin Respir Crit Care Med 30:369–375
Rubin LJ (2004) Diagnosis and management of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest 126:7S–10S
Ng CS, Wells AU, Padley SP (1999) A CT sign of chronic pulmonary arterial hypertension: the ratio of main pulmonary artery to aortic diameter. J Thorac Imaging 14:270–278
Chaudry G, MacDonald C, Adatia I et al (2007) CT of the chest in the evaluation of idiopathic pulmonary arterial hypertension in children. Pediatr Radiol 37:345–350
Edwards PD, Bull RK, Coulden R (1998) CT measurement of main pulmonary artery diameter. Br J Radiol 71:1018–1020
Karazincir S, Balci A, Seyfeli E et al (2008) CT assessment of main pulmonary artery diameter. Diagn Interv Radiol 14:72–74
Truong QA, Massaro JM, Rogers IS et al (2012) Reference values for normal pulmonary artery dimensions by noncontrast cardiac computed tomography: the Framingham heart study. Circ Cardiovasc Imaging 5:147–154
Compton GL, Florence J, MacDonald C et al (2015) Main pulmonary artery-to-ascending aorta diameter ratio in healthy children on MDCT. AJR Am J Roentgenol 205:1322–1325
Akay HO, Ozmen CA, Bayrak AH et al (2009) Diameters of normal thoracic vascular structures in pediatric patients. Surg Radiol Anat 31:801–807
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Caro-Domínguez, P., Compton, G., Humpl, T. et al. Pulmonary arterial hypertension in children: diagnosis using ratio of main pulmonary artery to ascending aorta diameter as determined by multi-detector computed tomography. Pediatr Radiol 46, 1378–1383 (2016). https://doi.org/10.1007/s00247-016-3636-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-016-3636-5