Abstract
Background
Image-guided percutaneous core needle biopsy is a common procedure for diagnosis of both solid tumors and hematological malignancies in children. Despite recent improvements, a certain rate of non-diagnostic biopsies persists.
Objective
To assess the factors influencing the diagnostic yield and accuracy of percutaneous core needle biopsies of pediatric tumors.
Materials and methods
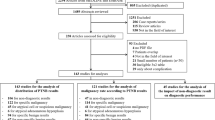
We conducted a single-center retrospective study of a 26-year experience with image-guided biopsies in children and young adults. Using uni- and multivariate analysis, we evaluated the association of diagnostic yield and accuracy with technical factors (image-guided procedure, pathological technique) and clinical factors (complication rate, histological type and anatomical location).
Results
We retrieved data relating to 396 biopsies were performed in 363 children and young adults (mean age: 7.4 years). Overall, percutaneous core needle biopsy showed a diagnostic yield of 89.4% (95% confidence interval [CI] 85.9–92.2) and an accuracy of 90.9% (CI 87.6–93.6) with a complication rate of 2.5% (CI 1.2–4.6).The diagnostic yield increased with the use of advanced tissue assessment techniques (95.7% with immunohistochemistry versus 82.3% without immunohistochemistry; P < 0.0001) and an increased number of passes (mean: 3.96 for diagnostic biopsies versus 3.62 for non-diagnostic biopsies; P = 0.044).
Conclusion
The use of advanced pathological techniques and an increased number of passes are the two main factors influencing the diagnostic success of biopsies in pediatric tumors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Image-guided percutaneous core needle biopsy plays an increasingly important role in the diagnosis of both solid tumors [1] and hematological malignancies [2]. Recent literature has confirmed that image-guided biopsy is a safe, accurate and reliable diagnostic procedure for childhood tumors [1–9].
Major advances in pathology techniques during the last two decades, including molecular pathology (such as reverse transcription polymerase chain reaction [RT-PCR] and fluorescence in situ hybridization [FISH]) [10] and cytogenetics (such as amplification of the MYCN gene, and the DNA index for neuroblastoma) [1, 11, 12] have greatly contributed to improvements in biopsy diagnostic accuracy [13]. Despite these improvements, however, a certain rate of non-diagnostic biopsies persists.
The purpose of this study was, first, to globally evaluate the diagnostic yield and accuracy of image-guided biopsy of solid tumors and hematological malignancies in children. Second, it aimed to identify the factors that positively or negatively affect those indicators — whether they relate to radiologic or histological techniques or to the type and location of the lesion — with a view toward informing the discussion on potential areas of improvement for interventional radiology practitioners.
Materials and methods
We retrospectively retrieved data pertaining to all image-guided biopsies undertaken over a 26-year period (1986 to 2012) in a single center (Imaging Department of Armand Trousseau Hospital, Paris, France). The study was conducted in accordance with the recommendations of the institutional review board.
We included biopsies for diagnosis of solid organ and soft-tissue tumors of unknown nature and suspected hematological malignancies. Biopsies undertaken to document an already known infection or to diagnose diffuse liver or renal disease with no clearly identifiable mass lesion were excluded, as well as cases with incomplete data. We also reviewed medical, pathology and interventional radiology records for relevant clinicopathological data, including histopathology and biopsy procedures, as well as cancer history when recurrence of a previous primary malignant tumor was suspected. Final reference diagnoses were obtained from surgical pathology reports, bone marrow biopsies, and radiographic or clinical follow-up.
Before each biopsy, patient blood had been screened with coagulation testing and platelet count. As per the policy at our institution, the biopsy was generally done under general anesthesia in children younger than 8 years and in uncooperative children, whereas premedication and local anesthesia were given to children older than 8 years, with the exception of vertebral biopsies.
The majority of children were monitored clinically for 4–5 h in the hospital post biopsy before being discharged on the same day. When lung biopsies were done, patients were controlled for absence of pneumothorax with a chest radiograph 6 h after the procedure. Several pediatric radiologists did the biopsies under CT or US guidance. In biopsies performed for solid organs, lung and mediastinum, soft-tissue lesions, and bone lesions with cortical disruption, the type of needle was either a semiautomatic cutting needle (Gallini medical services, Mantova, Italy) or a semi-automated co-axial Temno biopsy system (CareFusion, McGaw Park, IL), with needle gauge ranging from 18 to 22 and throw length from 10 cm to 16 cm. Tissue from sclerotic bone was obtained with larger bone biopsy needles (e.g., 11-G trephine needle, Laredo type). Radiologists performed the biopsies in the radiology department or in the operating room. In cases of renal tumor that required biopsies, percutaneous core needle biopsies were done with a retroperitoneal approach to minimize the risk of flank tumor dissemination.
The classification of complications was undertaken in accordance with the guidelines published by the Society of Interventional Radiology [14]. Major complications were defined as requiring an admission to hospital for therapy (for outpatient procedures), such as in cases of clinically significant bleeding or infection, an unplanned increase in the level of care or prolonged hospitalization, permanent adverse sequelae or death. Minor complications were defined as those resulting in short hospital stay for observation only or minimal therapy (e.g., management of pain). In cases of soft-tissue tumors or suspicion of Ewing sarcoma, surgical advice on needle tract choice was sought to facilitate the subsequent resection.
During the biopsy procedure, an experienced pathologist was present in the room to optimize the handling of biopsy samples. For histopathological processing and immunohistochemical analysis, samples were fixed in 10% formalin. Samples of fresh tissue were rapidly frozen for DNA index, FISH, or polymerase chain reaction (PCR) analysis or placed in a standard cell culture media (Roswell Park Memorial medium) or ethylenediaminetetraacetic acid for cytogenetics (karyotyping, FISH assessment of MYCN amplification status, tumor DNA index [ploidy], or array comparative genomic hybridization [CGH] of neuroblastoma) and molecular pathology analysis (RT-PCR or FISH to detect tumor-specific fusion products). Bacteriological analysis was done when an infection could not be excluded, especially in the case of bone lesions.
The descriptive results are presented as means (± standard deviation [SD]; range minimum–maximum) or medians (interquartile range [IQR]) for continuous data and as percentages for categorical data.
For the diagnostic yield and accuracy analysis, the final diagnosis defining the reference status was determined by using the results from all available post-biopsy examinations or clinical data, including surgical or bone marrow specimens and clinical or radiographic follow-up. Diagnostic yield was calculated as the proportion of successful biopsies among all biopsies performed, following the guidelines to define successful diagnostic biopsies as those yielding sufficient material to establish a pathological diagnosis or to appropriately guide clinical care [14]. Diagnostic accuracy was calculated as the proportion of accurate biopsies among all biopsies performed, defining accurate biopsies as those being diagnostic or suggestive of the final result but requiring further diagnostic procedures to ascertain the final diagnosis. Inadequate biopsies were defined as samples with which the pathologist could not make a diagnosis because of insufficient size, necrosis, blood or crush artifacts.
In addition to the aforementioned analyses, a more detailed assessment of the extent of agreement between biopsy and final diagnosis was done by computing the unweighted and weighted kappa coefficients, along with their bootstrapped 95% confidence intervals. This was done by considering the following possible diagnostic categories: non-informative/inadequate, normal tissue, inflammatory tissue, benign tumor, and malignant tumor. The weighted kappa coefficients allow for penalizing differently the disagreements observed, depending on whether malignancy was the cause of the discrepancies between examinations and thus attaching greater emphasis to diagnostic errors involving malignancy than to errors across nonmalignant categories. The kappa values were interpreted as follows: kappa >0.75 indicates excellent agreement, 0.40–0.75 fair to good, and below 0.40 poor [15].
Univariate analyses were done with the use of chi-square or Fisher exact tests for categorical variables, and unpaired t-test or Mann–Whitney rank sum test for continuous variables, as appropriate, for comparing diagnostic yield and accuracy according to the potential factors described above. Correlation between continuous variables (e.g., number of passes, age) was assessed by the use of Pearson correlation coefficients. Univariate and multivariate analyses were conducted using logistic regression models, considering diagnostic success or accuracy as the dependent variable, using the Firth penalized maximum likelihood estimate to take into account the small sample size, and expressing results as odds ratios (OR) along with their 95% confidence intervals. Factors associated at the level of P < 0.2 in univariate analysis were entered in the model as potential predictors, and a stepwise approach was followed by removing non-significant variables at each step until reaching the final model. Temporal changes in indices were additionally assessed by using chi-square tests for trend. A two-sided P-value ≤0.05 was considered statistically significant. All statistical analyses were done with the Stata software version 12.1 (StataCorp, College Station, TX).
Results
Study cohort and final diagnoses
Among the 517 image-guided percutaneous core needle biopsy procedures performed in our department during the study period, 399 biopsies were performed for a solid mass or a suspected hematological malignancy. Three cases were excluded for incomplete data, yielding a total of 396 biopsies performed in 166 females and 197 males. The patients’ ages at biopsy ranged from 5 days to 21.1 years (mean: 7.4 years; median: 6.4 years). Of the 396 percutaneous biopsies included, 334 (84.3%) were indicated for primary diagnosis of a suspected solid tumor or hematological malignancy. Sixty-two (15.7%) were indicated to document a suspected recurrent malignancy in patients with known primary cancer.
The final diagnoses were malignant tumors (n = 277), benign tumors (n = 67), and non-neoplastic disease (n = 52, including 31 inflammatory and infectious lesions and 21 normal tissue samples).
Overall diagnostic yield and accuracy of percutaneous core needle biopsy
Across the whole study period, the diagnostic yield of biopsy was 89.4% (95% confidence interval 85.9–92.2) and its accuracy 90.9% (87.6–93.6) (Table 1).
Time-trend analysis (Table 1) showed a non-significant evolution in diagnostic yield between 1986 and 2012 (P = 0.185) and accuracy (P = 0.073).
Non-diagnostic biopsies
Forty-two biopsies were non-diagnostic, which represents 10.6% of our study cohort. There were six non-diagnostic but accurate biopsies (ie suggestive of the final result but requiring further work-up) of which three were eventually confirmed as Langerhans cell histiocytosis, two as lipoblastoma and one as thymic cyst. There were 36 inaccurate results, including 24 inadequate biopsies.
Obtaining the final diagnosis
Of the 36 inaccurate biopsies, 5 were repeated after initial failure. In four of these, the results of the new biopsy were confirmed either by surgery (n = 3) or by bone marrow biopsy in a case of lymphoma (n = 1). In one case (Wilms tumor), the diagnosis could not be assessed based on the repeated biopsy and was obtained at surgery. In 29 cases, the final diagnosis was obtained at surgery (surgical biopsy or surgical resection). In two cases of lymphoma, confirmation was obtained through bone marrow biopsy alone, without recourse to surgery.
Inaccurate biopsies — pathology results
In two cases, results consisted of benign tumors (angiomyolipoma and mesenchymal hamartoma) erroneously interpreted as nonspecific malignant tumor proliferation.
Biopsies resulted in a misdiagnosis of a malignant tumor as a benign tumor in two cases of ganglioneuroblastoma. The neuroblastic malignant component was missed at biopsy, and a ganglioneuroma was suggested (Fig. 1). In one case of malignancy (Hodgkin disease), the sample contained only inflammatory tissue, with no tumor cells present. In the 31 remaining inaccurate results, biopsies failed to detect a malignant tumor proliferation because the tissue samples were inadequate (n = 24) (due to small size, fibrosis, or necrosis) (Fig. 2) or because normal tissue was biopsied instead of the lesion (n = 7).
Non-contributive percutaneous core needle biopsy resulting from insufficient sampling of the tumor in a 13-year-old girl with a retroperitoneal ganglioneuroblastoma. a Axial contrast-enhanced abdominal CT obtained in prone position before biopsy shows a large retroperitoneal hypointense mass encasing the inferior mesenteric artery (arrows). b Biopsy of the mass with the tip of the biopsy needle shown (arrowhead). c Histology of the tumor biopsy shows Schwannian component (solid arrow) with mature ganglionic cells (dashed arrow) without neuropile component (hematoxylin and eosin, magnification x400). d Histological examination after surgical resection shows neuropile component with maturing and mature neuroblasts (arrows) (hematoxylin and eosin, magnification x400)
Non-contributive percutaneous core needle biopsy resulting from necrotic tissue biopsy in a 7-year-old boy with a renal papillary carcinoma. a Axial contrast-enhanced abdominal CT image obtained in prone position before biopsy shows a well-defined left renal mass, with regular borders and a hypodense center (arrows). b Axial CT at the same level as (a) shows the biopsy needle (arrowhead). c Histology of the tumor biopsy shows normal architecture of the renal cortex (solid arrow) and necrotic tissue (dotted arrow) (hematoxylin & eosin, magnification x5). d Histological examination of the surgical specimen shows the presence of tumor cells of type I papillary carcinoma (arrowheads) (hematoxylin & eosin, magnification x40)
Regarding agreement between biopsy and final diagnosis, when we considered that misdiagnosing a malignant tumor had the same impact as misdiagnosing non-malignancy, the unweighted kappa coefficient obtained was 0.786 (P < 0.0001). When misdiagnosis of a malignant tumor was over-penalized, the corresponding weighted kappa coefficient was only slightly higher at 0.796 (P < 0.0001) (Table 2).
Diagnostic yield and accuracy according to clinicopathological characteristics
No statistically significant difference in diagnostic yield and accuracy was observed between image-guided biopsy for primary disease and biopsy for recurrence or metastasis (90.1% [86.4–93.1] versus 85.5% [74.2–93.1] diagnostic yield, P = 0.276; 91.6% [88.1–94.4] versus 87.1% [76.1–94.3] accuracy, P = 0.256). Patients with diagnostic biopsies were younger than those with non-diagnostic biopsies (mean age: 7.2 years [±standard deviation 5.3] versus 9.4 [±5.7]; P = 0.011) and patients with accurate biopsies were younger than those with inaccurate biopsies (mean age: 7.2 [±5.2] versus 9.7 [±5.9]; P = 0.008). A statistically significant negative correlation was found between age and the number of passes (r = −0.10; P = 0.040); the mean number of passes was 4.0 (±1.0) in patients 8 years and younger and 3.8 (±1.1) in patients older than 8 years (P = 0.062).
Table 1 presents a summary of the indices according to anatomical and histological type of tumor. No statistically significant difference was observed in diagnostic yield between the different histological (global P = 0.193) and anatomical locations (global P = 0.460), and in accuracy between anatomical locations (global P = 0.172), whereas accuracy differed significantly across histological types (global P = 0.002), with the highest accuracy found in nonmalignant lesions.
Diagnostic performance indices according to histopathological techniques
No association was found between the failure rates and the pathologists who did the analyses (P = 0.905 diagnostic yield; P = 0.959 accuracy). Figure 3 presents the evolution of the histopathological techniques used between 1986 and 2012, and Table 3 shows the corresponding diagnostic yield and accuracy indices.
Ancillary studies, including immunohistochemistry, biopsy sample freezing, molecular pathology, and cytogenetic analysis, were increasingly used toward the end of the study period. Of particular note was the finding that diagnostic yield was significantly increased when immunohistochemistry was used (P < 0.0001), as well as the use of freezing (P = 0.011).
Molecular pathology analyses were done in 28 cases, mainly to detect tumor-specific fusion products through RT-PCR or FISH. Cytogenetic analysis was mainly used to determine MYCN status (in 53 neuroblastoma samples) and array CGH (in 10 neuroblastoma samples). From 2011 onward, use of the CGH array technique greatly increased (0% for 1986–1996, 0.6% for 1997–2006, and 8.3% for 2007–2012; P < 0.0001).
Diagnostic yield and accuracy according to radiologic techniques
The procedure was done under general anesthesia in 235 cases and local anesthesia in 159 cases (missing data in two cases (1984 and 1998)). The biopsies were performed under CT guidance in 64% of cases (n = 256) or US guidance in 35% (n = 140). Biopsies were performed at the radiology department in 350 cases and in the operating room in 44 cases (missing data in two cases (different from above): (1988 and 2002)).
Most biopsies were done with an 18-gauge needle size (G) (n = 332). The median number of passes was 4 (range: 1–10 passes; IQR 3–4). The mean number of passes increased over time from 3.77 to 4.31 between 1986 and 2012. The number of passes was higher in diagnostic biopsies than in non-diagnostic biopsies (mean: 3.96 versus 3.62, respectively; P = 0.044), as in accurate biopsies when compared to inaccurate biopsies (3.96 versus 3.56, respectively; P = 0.021). No statistically significant difference was observed in diagnostic yield nor accuracy when the biopsy was done under general anesthesia at the radiology department rather than under local or general anesthesia in the operating room (diagnostic yield: 92.1% [95% confidence interval: 87.4–95.5], 88.1% [82.0–92.6] and 81.8% [67.3–91.8], respectively, P = 0.107; accuracy: 93.7% [89.3–96.7], 89.3% [83.4–93.6], and 84.1% [70.0–93.4], respectively, P = 0.092).
No statistically significant difference in diagnostic yield (P = 0.340) nor accuracy (P = 0.375) was found among interventional radiologists. Regarding the needle gauge, no statistically significant difference was found between ≤17-G and ≥18-G needle sizes (diagnostic yield, P = 0.215; accuracy, P = 0.864).
Independent predictors of diagnostic yield and accuracy
Results from multivariate analysis by logistic regression are shown in Table 4. Decreasing age and use of immunochemistry were found to be independently associated with diagnostic success. The same two factors and diagnostic group were independently associated with accuracy.
Complications
Complications were reported in 10 cases out of the 396 biopsies (2.5% [1.2–4.6]), with 7 considered as minor and 3 as major. No biopsy-related deaths or needle tract tumor recurrences were observed in this study.
Major complications consisted of two major bleeds that required transfusion and hospitalization. One patient bled intraperitoneally after a hepatic biopsy to investigate leukemia and had successful hemostatic surgery. Another patient presented with a compressive hemothorax after a chest biopsy for a thymic cyst, which was resolved by chest tube drainage. A third patient sustained peritonitis from a small-intestine perforation after a celiac lymph node biopsy for a T-cell lymphoma.
Minor complications included pain and slight bleeding (n = 5) that resolved spontaneously, pneumothorax (n = 1) that did not require a chest tube, and transient laryngotracheal spasm (n = 1) that was treated by transient placement of an endotracheal tube.
Between 1986 and 2012, the number of biopsy complications decreased by 3.3% [95% CI: 0.9–8.2] for 1986–1996, 2.4% [0.7–6.0] for 1997–2006, and 1.9% [0.2–6.5] for 2007–2012 (P = 0.77). The complication rate appeared slightly higher in the non-diagnostic biopsy results than in diagnostic results (7.1% [1.5–19.5] complications versus 2.0% [0.8–4.0], P = 0.079).
Discussion
This study, based on almost three decades of data collection at our center, has shown that image-guided biopsies can be highly efficient in diagnosing both solid and hematological malignancy in children. However, our experience indicates that a certain rate of non-diagnostic biopsies remains non-reducible. In addition to the revolutionary advances in pathological techniques over the study period, there remain several aspects of radiologic methods that may have strong potential for improvement.
In this study, image-guided biopsies were found to have overall diagnostic yield of 89.4% and accuracy of 90.9%. This is in accordance with previous studies, in which the reported rates of biopsy diagnostic accuracy ranged from 76% to 98% [1–9].
Though not reaching statistical significance, our study showed an apparent improvement in percutaneous core needle biopsy success over time, from 85.1% to 91.7%, between 1986 and 2012. It is likely that advances in pathological assessment techniques have at least partly contributed to the improvement of the biopsy success rate, as reported in recent literature [16]. In particular, immunohistochemical staining has greatly increased the diagnostic capability of pathologists in distinguishing small round blue cell tumors [6, 13, 17]. Molecular pathology techniques, such as RT-PCR and FISH, have become important tools for the detection of pathogenic fusion translocations associated with pediatric soft-tissue tumors, such as Ewing sarcoma/primitive neuroectodermal tumor (PNET), alveolar rhabdomyosarcoma, desmoplastic small round cell tumor, and synovial sarcoma [6, 10, 18]. The recent development of cytogenetic analysis of neuroblastoma, including MYCN copy number [1, 12] and CGH array [13], has also contributed to the increasing success of biopsy as a prognostic marker.
Forty-two biopsies in our study were non-diagnostic. Although their proportion tended to decrease, there was no significant difference in their rate over time. Several factors might explain this non-reducible rate of non-diagnostic biopsies.
First, most of the non-diagnostic biopsies were a result of inadequate tissue samples (24 cases), as reported in other studies [4, 19]. The inclusion [1, 2, 19] or exclusion [5, 6, 20] of these inadequate results is debatable. We chose not to exclude inadequate samples in calculating the overall accuracy of biopsies because their exclusion, based on the hypothesis that they occur at random, is potentially inexact. Inadequate samples may contain overly high levels of false-negative results; thus, their exclusion could artificially increase diagnostic yield and accuracy [21]. An intrinsic weakness of the percutaneous core needle biopsy technique lies in the difficulty of procuring adequate material for diagnosis [20] as a result of tumor heterogeneity, necrosis, and crush artifacts. This highlights the value of the presence of a pathologist during the biopsy procedure to avoid inappropriate handling of samples and to assist the radiologist in confirming their adequacy. Similarly, as reported in other studies [22], we recommend on-site cytopathological examinations of touch preparations or aspirate to check whether the samples obtained contain necrosis or abnormal cells. Radiologists would therefore have more information available to assist them in deciding whether further passes are necessary, which could improve the diagnostic success of biopsies.
Second, the diagnosis of some tumors is difficult given the pathology of biopsies. In our study, biopsy misdiagnosed a malignant tumor as a benign tumor in two cases of a ganglioneuroblastoma; in these cases the biopsy missed the malignant component and diagnosed a ganglioneuroma. This underlines the necessity for negative biopsies to be repeated or further explored when clinical and radiologic suspicion of malignancy is high [3, 4]. It is noteworthy that, among the non-diagnostic biopsies in our study, four of the five repeated biopsies produced a result in agreement with the suspicions related to the first biopsy. Other areas are worth exploring to achieve a reduction in this rate of non-diagnostic biopsies.
Interestingly, percutaneous core needle biopsy showed higher diagnostic yield and accuracy in children younger than 8 years. The clinical significance of this result remains unclear. Based on our experience, fast-growing tumors reaching a higher tumor volume can more frequently be observed in younger children at the time of biopsy and hence are likely associated with a facilitated access for the operator. However, we lacked the ability to actually test this association, given the absence of information on tumor volume in our data set drawn from a retrospective review.
Among other possible factors, we found a negative correlation between age and the number of passes. Though indicating a clinically poor to moderate association, this could in part contribute to the higher diagnostic yield and accuracy in younger children.
The frequent use of CT guidance is very specific to our department practice. In the literature, US is preferred over CT for image guidance in pediatric biopsy because of its ability to image in true real time, its portability, the speed of the procedure, and the absence of ionizing radiation [23–27]. Pulmonary lesions and osseous lesions of the spine and pelvis are best approached with CT guidance, as are lesions that are difficult to observe with sonography [28]. Reducing the radiation exposure of the patient is essential. When CT scan was not done for diagnosis and tumor extension evaluation as a single procedure, we minimized the coverage to the area of concern and limited the delivered dose by reducing mAs to the lowest level that provides adequate visualization of a lesion for biopsy purposes, as described in recent studies on CT-guided biopsy procedure [8, 9, 29, 30]. Finally, all things being equal, biopsies are likely to be of better quality when undertaken in the radiologists’ habitual working environment, using equipment with which they are familiar.
In our study, biopsy success increased with the number of passes, as reported in other studies [31]. The mean number of passes increased over time from 3.77 to 4.31 between 1986 and 2012. The supplementary specimen was provided to pathologists for ancillary studies. However, the number of passes remained lower in our study compared with others [1].
Complications were rare and mostly of minor clinical consequence. The overall complication rate in our study was 2.5%, whereas the rate of major complications was 0.75%. With an upper 95% confidence limit less than 5%, this finding is in agreement with previous findings from the literature [6, 14].
On the other hand, other factors seem to have no correlation with the non-diagnostic biopsy rate. There was no statistically significant difference between the diagnostic yield and accuracy in primary malignancies than in recurrences. The reason for biopsy failure was not related to tumor anatomical location or to lesion histological type [4], with the exception of rare sarcomas such as myxoid liposarcoma, which has been associated with lower diagnostic yield and accuracy [32].
The literature suggests that operator dependency in percutaneous core needle biopsy is low, thanks to the precision and reliability provided by automated biopsy devices [4, 24, 33]. This was confirmed in our study, in which no significant association between operator experience and diagnostic success was found.
This study has several limitations. First, we did not review cross-sectional imaging studies to specifically record the lesion size and accessibility and the needle position. This was because of the impossibility of using standardized measures, the data before 2005 being available only on paper and not in the computer database. It is noteworthy that the complication rate was higher in non-diagnostic biopsies than diagnostic biopsies. This suggests that failure to obtain sufficient material by percutaneous core needle biopsy could be related to technical limitations, such as difficulty of accessing the lesion.
Second, minor complications, such as pain or clinically insignificant bleeds, may have been underestimated, partly because of the retrospective nature of the study and partly because of difficulties in clinical assessment of pain in young children.
Finally, given the observational retrospective design of our study, no strict causal inference can be made; thus, the interpretation of our findings related to determinants of accuracy should be done with caution. Because the data collection was monocentric, the external validity of our results in other settings could also be questioned. It is noteworthy that decisions to do biopsy are made at our center regardless of the underlying technical difficulty and that the choice of the radiologist responsible is made in our department independently of the tumor type or the other professionals involved. Although we believe that these elements are in favor of limited over-optimism in our estimation of accuracy, further prospective and comparative studies should be done to provide stronger evidence in that regard.
Conclusion
Initial non-diagnostic results can often be resolved by repeating passes when the pathologist observes that the material is inadequate during the procedure or by repeating negative biopsies. The use of advanced pathological techniques and an increased number of passes are the two main factors influencing the diagnostic success of biopsies in pediatric tumors.
References
Garrett KM, Fuller CE, Santana VM et al (2005) Percutaneous biopsy of pediatric solid tumors. Cancer 104:644–652
Garrett KM, Hoffer FA, Behm FG et al (2002) Interventional radiology techniques for the diagnosis of lymphoma or leukemia. Pediatr Radiol 32:653–662
Sklair-Levy M, Lebensart PD, Applbaum YH et al (2001) Percutaneous image-guided needle biopsy in children — summary of our experience with 57 children. Pediatr Radiol 31:732–736
Skoldenberg EG, Jakobson AA, Elvin A et al (2002) Diagnosing childhood tumors: a review of 147 cutting needle biopsies in 110 children. J Pediatr Surg 37:50–56
Guimaraes AC, Chapchap P, de Camargo B et al (2003) Computed tomography-guided needle biopsies in pediatric oncology. J Pediatr Surg 38:1066–1068
Sebire NJ, Roebuck DJ (2006) Pathological diagnosis of paediatric tumours from image-guided needle core biopsies: a systematic review. Pediatr Radiol 36:426–431
Shin HJ, Amaral JG, Armstrong D et al (2007) Image-guided percutaneous biopsy of musculoskeletal lesions in children. Pediatr Radiol 37:362–369
Hryhorczuk AL, Strouse PJ, Biermann JS (2011) Accuracy of CT-guided percutaneous core needle biopsy for assessment of pediatric musculoskeletal lesions. Pediatr Radiol 41:848–857
Ballah D, Nijs E, Keller MS et al (2013) Percutaneous CT-guided vertebral bone biopsy in children. Pediatr Radiol 43:582–588
Chang CC, Shidham VB (2003) Molecular genetics of pediatric soft tissue tumors: clinical application. J Mol Diagn 5:143–154
Shimada H, Stram DO, Chatten J et al (1995) Identification of subsets of neuroblastomas by combined histopathologic and N-myc analysis. J Natl Cancer Inst 87:1470–1476
Hoffer FA, Chung T, Diller L et al (1996) Percutaneous biopsy for prognostic testing of neuroblastoma. Radiology 200:213–216
Sebire NJ (2011) Oncology: histopathology and imaging in the future. Pediatr Radiol 41:S170–S171
Gupta S, Wallace MJ, Cardella JF et al (2010) Quality improvement guidelines for percutaneous needle biopsy. J Vasc Interv Radiol 21:969–975
Fleiss JL (1981) Statistical methods for rates and proportions. Wiley, New York
Marshall D, Laberge JM, Firetag B et al (2013) The changing face of percutaneous image-guided biopsy: molecular profiling and genomic analysis in current practice. J Vasc Interv Radiol 24:1094–1103
Hogan MJ, Hoffer FA (2010) Biopsy and drainage techniques in children. Tech Vasc Interv Radiol 13:206–213
Klijanienko J, Couturier J, Bourdeaut F et al (2010) Fine-needle aspiration as a diagnostic technique in 50 cases of primary Ewing sarcoma/peripheral neuroectodermal tumor. Institut Curie’s experience. Diagn Cytopathol 40:19–25
Agid R, Sklair-Levy M, Bloom AI et al (2003) CT-guided biopsy with cutting-edge needle for the diagnosis of malignant lymphoma: experience of 267 biopsies. Clin Radiol 58:143–147
Puri A, Shingade VU, Agarwal MG et al (2006) CT-guided percutaneous core needle biopsy in deep seated musculoskeletal lesions: a prospective study of 128 cases. Skeletal Radiol 35:138–143
McInnes MD, Kielar AZ, Macdonald DB (2011) Percutaneous image-guided biopsy of the spleen: systematic review and meta-analysis of the complication rate and diagnostic accuracy. Radiology 260:699–708
Tsou MH, Tsai SF, Chan KY et al (2009) CT-guided needle biopsy: value of on-site cytopathologic evaluation of core specimen touch preparations. J Vasc Interv Radiol 20:71–76
Nobili V, Comparcola D, Sartorelli MR et al (2003) Blind and ultrasound-guided percutaneous liver biopsy in children. Pediatr Radiol 33:772–775
Hugosson CO, Nyman RS, Cappelen-Smith JM et al (1999) Ultrasound-guided biopsy of abdominal and pelvic lesions in children. A comparison between fine-needle aspiration and 1.2 mm-needle core biopsy. Pediatr Radiol 29:31–36
Fontalvo LF, Amaral JG, Temple M et al (2006) Percutaneous US-guided biopsies of peripheral pulmonary lesions in children. Pediatr Radiol 36:491–497
Bittles MA, Hoffer FA (2007) Interventional radiology and the care of the pediatric oncology patient. Surg Oncol 16:229–233
Roebuck DJ (2010) Paediatric interventional oncology. Cancer Imaging 10:S27–S34
Hoffer FA (2005) Interventional radiology in pediatric oncology. Eur J Radiol 53:3–13
Smith JC, Jin DH, Watkins GE et al (2011) Ultra-low-dose protocol for CT-guided lung biopsies. J Vasc Interv Radiol 22:431–436
Patel AS, Soares B, Courtier J et al (2013) Radiation dose reduction in pediatric CT-guided musculoskeletal procedures. Pediatr Radiol 43:1303–1308
Wu JS, Goldsmith JD, Horwich PJ et al (2008) Bone and soft-tissue lesions: what factors affect diagnostic yield of image-guided core-needle biopsy? Radiology 248:962–970
Pohlig F, Kirchhoff C, Lenze U et al (2012) Percutaneous core needle biopsy versus open biopsy in diagnostics of bone and soft tissue sarcoma: a retrospective study. Eur J Med Res 17:29
Elvin A, Andersson T, Jaremko G et al (1994) Significance of operator experience in diagnostic accuracy of biopsy gun biopsies. Eur Radiol 4:430–433
Acknowledgments
We would like to express our grateful thanks to Mr. James Winter for helping in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Blondiaux, E., Laurent, M., Audureau, E. et al. Factors influencing the diagnostic yield and accuracy of image-guided percutaneous needle biopsy of pediatric tumors: single-center audit of a 26-year experience. Pediatr Radiol 46, 372–382 (2016). https://doi.org/10.1007/s00247-015-3484-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-015-3484-8