Abstract
Spondyloarthritides are a group of inflammatory rheumatological diseases that cause arthritis with a predilection for spinal or sacroiliac involvement in addition to a high association with HLA-B27. Juvenile spondyloarthritis is distinct from adult spondyloarthritis and manifests more frequently as peripheral arthritis and enthesitis. Consequently juvenile spondyloarthritis is often referred to as enthesitis-related arthritis (ERA) subtype under the juvenile idiopathic arthritis (JIA) classification criteria. The American College of Rheumatology Treatment Recommendations for JIA, including ERA, are based on the following clinical parameters: current treatment, disease activity and the presence of poor prognostic features. The MRI features of juvenile spondyloarthritis include marrow edema, peri-enthesal soft-tissue swelling and edema, synovitis and joint or bursal fluid. Marrow edema is nonspecific and can be seen with other pathologies as well as in healthy subjects, and this is an important pitfall to consider. With further longitudinal study and validation, however, whole-body MRI with dedicated images of the more commonly affected areas such as the spine, sacroiliac joints, hips, knees, ankles and feet can serve as a more objective tool compared to clinical exam for early detection and monitoring of disease activity and ultimately direct therapeutic management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The term juvenile spondyloarthritis refers to a group of inflammatory rheumatological diseases distinct from adult spondyloarthritis. An association with the major histocompatibility complex (MHC) class I molecule HLA-B27 is found in 60–80% of children with juvenile spondyloarthritis [1]. Juvenile spondyloarthritis accounts for 20% of children with arthritis, or juvenile idiopathic arthritis (JIA) [2]. Juvenile spondyloarthritis commonly manifests as peripheral arthritis and enthesitis. Axial involvement is less common at onset compared to adult spondyloarthritis but often develops 5–10 years from disease onset. The joints of the lower limbs (hips, knees, ankles and feet) are the most commonly affected sites in contrast to spine and sacroiliac joint involvement, which occurs infrequently at disease onset but develops during the disease course [3]. The disease course is variable but can be associated with significant long-term morbidity, especially when the hips or spine are affected. Up to 40% of affected children develop ankylosing spondylitis within 10 years of disease onset [4]. Predictors of sacroiliitis or ankylosing spondylitis include HLA-B27, DRB1*04, male gender, age at onset of symptoms, family history of ankylosing spondylitis, arthritis, polyarthritis, enthesitis, tarsitis, hip involvement, axial involvement and psoriasis [5, 6].
Most pediatric rheumatologists utilize the International League of Associations for Rheumatology (ILAR) classification criteria for JIA to distinguish among the various forms of juvenile spondyloarthritis. Juvenile spondyloarthritis types are largely represented by the enthesitis-related arthritis (ERA), psoriatic arthritis and undifferentiated arthritis sub-types of JIA [7]. These subtypes typically occur during late childhood or adolescence. The mean age at time of diagnosis for ERA and psoriatic arthritis has been shown to be 11.7 years and 8.9 years, respectively [2].
The American College of Rheumatology Treatment Recommendations for JIA are based on current treatment, disease activity and features of poor prognosis [8]. From the treatment guidelines, features of poor prognosis include arthritis affecting designated areas (hip, cervical spine, ankle or wrist), prolonged elevation of inflammatory markers, and radiographic damage (erosions or joint space narrowing) [8]. Accurate and early detection of disease activity and features of poor prognosis is vital for the appropriate selection of therapeutic agents. In ERA, expensive therapies such as biological agents (anti-tumor necrosis factor therapy) are indicated only in children with axial involvement or with refractory peripheral disease with poor prognostic factors unresponsive to standard therapies [8]. Subjective assessment of disease activity by clinical exam, however, has been shown to overestimate peripheral enthesitis in pediatric patients with enthesitis-related arthritis compared to MRI [9]. Furthermore, poor prognostic indicators are based on radiographic evidence of disease, which is delayed and not necessarily reflective of active disease.
Whole-body MRI for evaluation of juvenile spondyloarthritis is advantageous in that it allows for assessment of both disease activity and extent. Several studies have shown it to be a valuable adjunct to clinical exam in adults with spondyloarthropathies and psoriatic arthritis [10–14]. Studies in the pediatric population are limited, but whole-body MRI has been shown to be superior to clinical examination in detecting arthritis in the hips, sacroiliac joints and spine [9]. Consequently, whole-body MRI may play an important role alongside clinical exam and radiography as an objective tool for assessing active disease activity and guiding therapy in juvenile spondyloarthropathy patients.
Protocol
Scans are performed on an Avanto 1.5-T MRI scanner with a dedicated multichannel surface coil system (Siemens Total Imaging Matrix; Siemens Healthcare, Erlangen, Germany). Patients are placed supine with arms down by the sides and the whole body is covered with coils to allow for continguous scanning. Integrated head, neck, spine, body and peripheral angiography surface coils are utilized. Images are acquired at multiple stations with the patient free-breathing; the images are subsequently reconstructed using the vendor-specific software package (Siemens Composing; Siemens, Erlangen, Germany) to form a whole-body image (Fig. 1). Images, sequences and parameters are as outlined in Table 1 and include the following short tau inversion recovery (STIR) sequences: coronal whole body, sagittal spine, coronal oblique sacroiliac joints, axial pelvis, sagittal knee joints and sagittal ankle/forefoot. Stations on whole-body sequences are overlapped 25–30% to improve quality of the final composed image. Parallel imaging is utilized to accelerate image acquisition. Gadolinium and antiperistaltic agents are not routinely administered for this study. The need for sedation is evaluated case-by-case but is not frequently used in our experience. Total scan time is approximately 1 h but varies with patient size and number of stations required. Studies are scheduled with 1.5-h time slots.
Each study is billed to the Ontario Health Insurance Program. Billing codes for MRI thorax, abdomen, pelvis and extremities are submitted because a billing code for whole-body MRI does not exist in the Ontario Health Insurance Program.
Distribution
Inflammation of the entheses, or enthesitis, is a predominant finding in juvenile spondyloarthritis and has been shown to affect 60–80% of patients [15]. Entheses are the sites of attachment of tendons, ligaments, joint capsules or fascia onto bone. The term “enthesis organ” encompasses the enthesis itself and the adjacent associated structures that function to dissipate the biomechanical stresses at the bone–enthesis interface [16]. Associated structures include fibrocartilages, bursae and fat pads. The Achilles tendon insertion is the prototypical example of the enthesis organ (Fig. 2) and one of the most common sites of involvement in juvenile spondyloarthritis. Enthesitis is manifest as marrow edema at entheseal sites, peri-enthesal soft-tissue swelling and edema, synovitis and associated joint or bursal fluid on MRI.
The arthritic and entheseal changes of juvenile spondyloarthritis can involve both the axial and peripheral appendicular skeleton.
Appendicular skeleton
Lower extremities
Enthesitis of the lower extremity joints is typical of juvenile spondyloarthritis, particularly involving the hips, knees, ankles and feet (Fig. 3). The inferior pole of the patella (50%) (Fig. 4), plantar fascial insertion into the calcaneus (38%) or metatarsal head (22%) and Achilles tendon insertion into the calcaneus (22%) (Fig. 5) were the most frequently affected sites in a cohort of patients with ERA [17]. The entheses at the hip joints, particularly the extensor muscle insertions at the greater trochanter, are also commonly involved. A cross-sectional study by Rachlis et al. [9] that utilized whole-body MRI identified the hip extensor insertion at the greater trochanter as the most common site of involvement (Fig. 6).
Enthesitis of the lower extremities. Short tau inversion recovery (STIR) MR images show abnormal hyperintense signal in areas of involvement in the bones of the feet and ankles (arrows) in two 14-year-old boys (a, b) and one 12-year-old boy (c). a Axial image shows right foot second metatarsal and cuboid. b Sagittal image shows left foot talus, cuboid and anterior calcaneus. c Sagittal image shows base of the 5th metatarsal, site of insertion of the peroneus brevis tendon
Tarsitis is inflammation of the intertarsal joints, overlying tendons, entheses and soft tissues of the midfoot and is a characteristic finding in juvenile spondyloarthritis (Fig. 7). It has been reported in up to one-third of children at disease onset [18]. A separate study demonstrated midfoot enthesitis in 88% of patients with active inflammatory disease at short-term follow-up [19]. Children present with a painful, swollen and restricted midfoot characterized by marrow and soft-tissue edema, synovitis, joint effusions and bursitis on MRI. Findings should be distinguished from edema-like changes seen in the feet of healthy children, which are usually symmetrical and lack the associated inflammatory features. These are suspected to represent residual hematopoietic marrow and disappear with age [20, 21].
Upper extremities
Upper extremity involvement in juvenile spondyloarthritis occurs with less frequency. Enthesitis can affect the shoulder at the humeral tuberosities (Fig. 8) and at the acromioclavicular joints (Fig. 9). Elbow joint involvement is seen much less commonly in comparison. The small joints of the hand are usually spared clinically [1].
Upper extremity involvement is less common but usually involves the shoulders and can involve the humeral tuberosities with marrow edema adjacent to the insertion of the supraspinatus. Coronal short tau inversion recovery (STIR) MR image of the shoulder shows foci of hyperintensity in the right humeral epiphyses (arrow) of a 16-year-old boy
Axial skeleton
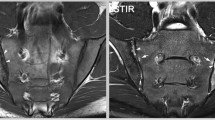
Although axial involvement is less common at presentation compared to adult spondyloarthritis, it can develop within several years of disease onset and typically manifests in the sacroiliac joints first (Figs. 10 and 11). A cohort study involving 59 children with ERA reported the development of MRI evidence of sacroiliitis in 30% of children within 1 year of disease onset [6]. The number of joints and entheses with disease at onset was predictive of subsequent sacroiliac joint involvement. Other studies have shown radiographic evidence of sacroiliitis in up to 92% of children with juvenile spondyloarthritis 5 years after disease onset [22]. MRI findings typical of sacroiliitis include T2 hyperintensity and enhancement at the sacroiliac joints in acute disease, sclerosis, erosions and ankylosis.
Axial skeleton involvement in a 14-year-old boy with enthesitis-related arthritis who presented with hip and sacroiliac joint pain. a Coronal oblique and (b) axial short tau inversion recovery (STIR) MR images demonstrate increased signal intensity at the sacral and iliac sides of the sacroiliac joints, right greater than left, consistent with sacroiliitis
Axial skeleton involvement in a 15-year-old boy with juvenile spondyloarthritis. a, b Coronal short tau inversion recovery (STIR) MRI images show increased marrow signal involving the iliac and sacral edges of the sacroiliac joints. Abnormal signal is also noted in the sacroiliac joints bilaterally. Additionally noted is increased STIR signal at the peritrochanteric region of the proximal left femur (arrow in b). STIR short tau inversion recovery
Corner lesions, or Romanus lesions, of the spine can also be seen in juvenile spondyloarthritis; these lesions represent erosions, marrow edema or osteitis at the vertebral body endplates (Fig. 12). Other sites of axial enthesitis-osteitis include the various ligamentous and muscular attachments of the pelvis: iliac crest, sartorius insertion at the anterior superior iliac spine, pubic symphysis and ischiopubic synchondrosis (Fig. 13).
Corner lesions and spinous process involvement in (a) a 12-year-old boy, (b) a 16-year-old boy and (c) a 13-year-old girl. MRI shows foci of increased STIR signal at the posterior aspect of the superior end-plate of L3 and anterior aspect of the inferior end-plates of T12 and L1 (arrows in a and c). Spinous process involvement at T11 and T12 is also shown (circles in b and c). STIR short tau inversion recovery
MRI of pelvic sites of enthesitis-osteitis. a Coronal short tau inversion recovery (STIR) MR image shows signal abnormality at the pubic bodies (arrows) in a 12-year-old boy. b Coronal STIR MR image shows abnormal signal in a 13-year-old girl extending into the ischiopubic synchondrosis and adjacent right quadratus femoris (small circle). There is also a small left hip effusion (large circle). c Coronal STIR MR image demonstrates abnormal signal at the anterior inferior iliac spines bilaterally (arrows) in a 13-year-old boy with enthesitis-related arthritis (ERA). d Oblique coronal STIR MR image of the sacroiliac joints in a 13-year-old girl with ERA shows abnormal marrow signal at the right superior iliac crest extending to the adjacent muscle (circle)
Limitations
Peri-entheseal bone marrow edema is a typical feature on whole-body MRI in juvenile spondyloarthritis. Bone marrow edema, however, can be nonspecific. Focal areas of bone marrow edema-like signal changes have also been shown in the carpal bones of 55.8% of healthy children [23]. The clinical significance of edema-like changes seen in the marrow of healthy children is an important potential pitfall to consider during interpretation, and further longitudinal studies are needed to determine clinical significance of such changes. In addition, although bone marrow edema seen on MRI has been shown to be predictive of erosive damage in adults, similar findings do not exist for the pediatric population [24].
Studies on the use of whole-body MR imaging in adult spondyloarthropathies and psoriatic arthritis have demonstrated findings seen in juvenile spondyloarthritis in healthy control subjects. For instance Poggenborg and colleagues [10] identified MRI findings of enthesitis in 14% of imaged entheseal sites in healthy subjects, 42% of these at the greater trochanters, which are commonly affected in juvenile spondyloarthritis. Similarly, Weber and colleagues [14] identified a single vertebral corner inflammatory lesion in up to 26% of healthy individuals. Further studies are needed to fully evaluate whole-body MRI in juvenile spondyloarthritis as a tool for diagnosing, monitoring disease activity and guiding treatment. Studies including a healthy control group are critical to this purpose.
Conclusion
Juvenile spondyloarthritis is a group of HLA-B27-associated inflammatory arthropathies characterized by arthritis and enthesitis; it predominantly affects the lower extremities at presentation, with development of axial involvement and sacroiliitis later in the disease course. Peri-enthesal bone marrow edema is a typical finding on MRI. Associated tendon or ligament thickening, adjacent soft-tissue swelling and edema, synovitis, and joint or bursal fluid are important features that may help distinguish juvenile spondyloarthritis from other pathology or edema-like findings seen in healthy subjects. Tarsitis is a characteristic manifestation of juvenile spondyloarthritis. Disease activity and the presence of poor prognostic factors including radiographic evidence of sacroiliitis are key determinants affecting treatment, especially in the initiation of expensive therapies such as biological agents. With further study and validation, whole-body MRI can be a valuable tool for early detection and diagnosis, an important adjunct for monitoring disease activity, and instrumental in guiding initiation and discontinuation of anti-arthritis therapies.
References
Tse SM, Laxer RM (2012) New advances in juvenile spondyloarthritis. Nat Rev Rheumatol 8:269–279
Saurenmann RK, Rose JB, Tyrrell P et al (2007) Epidemiology of juvenile idiopathic arthritis in a multiethnic cohort: ethnicity as a risk factor. Arthritis Rheum 56:1974–1984
Burgos-Vargas R, Pacheco-Tena C, Vazquez-Mellado J (2002) A short-term follow-up of enthesitis and arthritis in the active phase of juvenile onset spondyloarthropathies. Clin Exp Rheumatol 20:727–731
Minden K, Niewerth M, Listing J et al (2002) Long-term outcome in patients with juvenile idiopathic arthritis. Arthritis Rheum 46:2392–2401
Flato B, Hoffmann-Vold AM, Reiff A et al (2006) Long-term outcome and prognostic factors in enthesitis-related arthritis: a case–control study. Arthritis Rheum 54:3573–3582
Pagnini I, Svelli S, Matucci-Cerinic M et al (2010) Early predictors of juvenile sacroiliitis in enthesitis-related arthritis. J Rheumatol 37:2395–2401
Petty RE, Southwood TR, Manners P et al (2004) International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol 31:390–392
Beukelman T, Patkar NM, Saag KG et al (2011) 2011 American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: initiation and safety monitoring of therapeutic agents for the treatment of arthritis and systemic features. Arthritis Care Res 63:465–482
Rachlis A, Babyn, Lobo-Mueller E et al (2011) Whole body magnetic resonance imaging in juvenile spondyloarthritis: will it provide vital information compared to clinical exam alone? Arthritis Rheum 63:S292
Poggenborg RP, Eshed I, Østergaard M et al (2014) Enthesitis in patients with psoriatic arthritis, axial spondyloarthritis and healthy subjects assessed by ‘head-to-toe’ whole-body MRI and clinical examination. Ann Rheum Dis. doi:10.1136/annrheumdis-2013-204239
Weckbach S, Schewe S, Michaely HJ et al (2011) Whole-body MR imaging in psoriatic arthritis: additional value for therapeutic decision making. Eur J Radiol 77:149–155
Karpitschka M, Godau-Kellner P, Kellner H et al (2013) Assessment of therapeutic response in ankylosing spondylitis patients undergoing anti-tumour necrosis factor therapy by whole-body magnetic resonance imaging. Eur Radiol 23:1773–1784
Song IH, Hermann K, Haibel H et al (2011) Effects of etanercept versus sulfasalazine in early axial spondyloarthritis on active inflammatory lesions as detected by whole-body MRI (ESTHER): a 48-week randomized controlled trial. Ann Rheum Dis 70:590–596
Weber U, Hodler J, Kubik RA et al (2009) Sensitivity and specificity of spinal inflammatory lesions assessed by whole-body magnetic resonance imaging in patients with ankylosing spondylitis or recent-onset inflammatory back pain. Arthritis Rheum 61:900–908
Petty R, Cassidy JT (2011) Textbook of pediatric rheumatology. Elsevier, Amsterdam
Benjamin M, McGonagle D (2001) The anatomical basis for disease localization in seronegative spondyloarthropathy at entheses and related sites. J Anat 199:503–526
Weiss PF, Klink AJ, Behrens EM et al (2011) Enthesitis in an inception cohort of enthesitis-related arthritis. Arthritis Care Res 63:1307–1312
Alvarez-Madrid C, Merino R, De Inocencio J et al (2009) Tarsitis as an initial manifestation of juvenile spondyloarthropathy. Clin Exp Rheumatol 27:691–694
Burgos-Vargas R, Pacheco-Tena C, Vazquez-Mellado J (2002) A short-term follow-up of enthesitis and arthritis in the active phase of juvenile onset spondyloarthropathies. Clin Exp Rheumatol 20:727–731
Pal CR, Tasker AD, Ostlere SJ et al (1999) Heterogeneous signal in bone marrow on MRI of children’s feet: a normal finding? Skelet Radiol 28:274–287
Shabshin N, Schweitzer ME, Morrison WB et al (2006) High-signal T2 changes of the bone marrow of the foot and ankle in children: red marrow or traumatic changes? Pediatr Radiol 36:670–676
Burgos-Vargas R, Clark P (1989) Axial involvement in the seronegative enthesopathy and arthropathy syndrome and its progression to ankylosing spondylitis. J Rheumatol 16:192–197
Müller LS, Avenarius D, Damasio B et al (2011) The paediatric wrist revisited: redefining MR findings in healthy children. Ann Rheum Dis 70:605–610
McQueen FM (2000) Magnetic resonance imaging in early inflammatory arthritis: what is its role? Rheumatology 39:700–706
Acknowledgments
We thank Danny Aguilar for his illustration of the Achilles tendon entheseal organ.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
CME activity This article has been selected as the CME activity for the current month. Please visit the SPR Web site at www.pedrad.org on the Education page and follow the instructions to complete this CME activity.
Rights and permissions
About this article
Cite this article
Aquino, M.R., Tse, S.M.L., Gupta, S. et al. Whole-body MRI of juvenile spondyloarthritis: protocols and pictorial review of characteristic patterns. Pediatr Radiol 45, 754–762 (2015). https://doi.org/10.1007/s00247-015-3319-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-015-3319-7