Abstract
The purpose of this study was to determine the correlation of different methods of assessing fluid overload and determine which metrics are associated with development of acute kidney injury (AKI) in the period immediately following Norwood palliation. This was a retrospective single-center study of Norwood patients from January 2011 through January 2021. AKI was defined using the Kidney Disease Improving Global Outcomes (KDIGO). Patients were separated into two groups: those with AKI and those without. A logistic regression analysis was conducted with AKI at any point in the study period as the dependent variable and clinical and laboratory data as independent variables. Analysis was conducted as a stepwise regression. The coefficients from the logistic regression were then used to develop a cumulative AKI risk score. Spearman correlations were conducted to analyze the correlation of fluid markers. 116 patients were included, and 49 (42.4%) developed AKI. The duration of open chest, duration of mechanical ventilation, need for dialysis, need for extracorporeal membrane oxygenation, and inpatient mortality were associated with AKI (p ≤ 0.05). Stepwise logistic regression demonstrated the following significant independent associations AKI: age at Norwood in days (p < 0.01), blood urea nitrogen (p < 0.01), central venous pressure (p = 0.04), and renal oxygen extraction ratio (p < 0.01). The area under the receiver operating characteristic curve for the logistic regression was 0.74. The fluid markers had weak R-value. Urea, central venous pressure, and renal oxygen extraction ratio are associated with AKI after the Norwood operation. Common clinical metrics used to assess fluid overload are poorly correlated with each other for postoperative Norwood patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fluid overload and acute kidney injury (AKI) are common complications following pediatric cardiac surgery and are associated with increased morbidity and mortality in the intensive care unit (ICU) [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16]. Infants are at risk for fluid overload after surgery for many reasons and as many as 30–68% of patients develop at least 10% fluid overload following cardiac surgery. Infants seem to be particularly at risk for fluid overload after surgery due to increased susceptibility to hemodilution and capillary permeability and may have greater stimulus to retain fluid due to age-specific nuances in the renin–angiotensin–aldosterone system. Fluid overload has previously been demonstrated to be associated with AKI, need for dialysis, acute lung injury, need for extracorporeal membrane oxygenation, and mortality. AKI is a frequent complication of fluid overload with an incidence of 15–60% after cardiac surgery and is an independent risk factor for worse outcomes, including prolonged hospital stay, longer duration of mechanical ventilation, and mortality. Younger children, particularly neonates, are at higher risk for developing AKI following cardiac surgery after adjusting for cardiopulmonary bypass time and surgical complexity.
Because of the consequences of fluid overload, monitoring for fluid overload is important. However, quantifying fluid overload after cardiac surgery remains difficult. Anecdotally, the patient’s weight has been used as the gold standard, however, this metric may be complicated by many factors, including scales, calibration, and inability to obtain weights due to patient condition. Net fluid balance, blood urea nitrogen, and central venous pressure are also utilized to estimate fluid status, but none are without their own limitations. There is no consensus regarding best practice for quantifying fluid status.
Children with single ventricle physiology typically undergo the Norwood palliation as the first step of the staged palliation. The Norwood palliation is associated with morbidity and mortality rates above 10%, and AKI has become a known risk factor for worse outcomes following cardiac surgery [1]. This study aimed to determine the correlation of different methods of assessing fluid overload and to determine which of these metrics are associated with the development of AKI in the period immediately following Norwood palliation.
Methods
Study Design
This was a retrospective single-center study. Institutional review board approval was received for this study. The study is in concordance with the Helsinki Declaration.
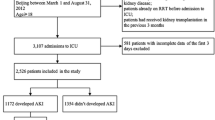
Patients who underwent the Norwood operation from January 2011 through January 2021 were identified through the Advocate Children’s Heart Institute surgical database. Those with AKI prior to Norwood and those who were required extracorporeal membrane oxygenation prior to Norwood were excluded from the analyses. The remainder of these patients were included for the final analyses.
Data of Interest
Data were collected for the following variables: age at Norwood (days), weight at Norwood (kg), central venous pressure (mmHg), fluid balance (mls), serum blood urea nitrogen(mg/dL), serum creatinine (mg/dL), mean arterial blood pressure (mmHg), pulse oximetry, and renal near infrared spectroscopy.
The following values were calculated from the data: creatinine to baseline creatinine ratio, fluid overload percent, and renal perfusion pressure. Creatinine to baseline creatinine was calculated by dividing the current creatinine by the baseline creatinine. Fluid overload percent was calculated as follows: ((current weight − baseline weight)/baseline weight) × 100. Renal perfusion pressure was calculated as mean arterial pressure − central venous pressure. Renal oxygen extraction ratio was calculated as follows: ((pulse oximetry − renal near infrared spectroscopy)/(pulse oximetry)) × 100.
Time Points
Baseline data (postoperative day 0) were collected the morning of the surgical day prior to going to the operating room. Data for all subsequent postoperative data were collected the morning of that specific postoperative day.
The fluid balance for each day represented the fluid balance for the prior 24 h. Thus, for postoperative day 2, the fluid balance represents the fluid balance from 7 am the day prior to 7 am that day. Data for fluid balance only is reported for postoperative day 2 onwards as the postoperative day 1 fluid balance would represent the fluid from the surgical day which would include fluid include from the operating room. What is often charted from the operating room may not actually be how much was administered to a patient due to the nature of how fluid in the operating room is charted; thus, we elected to eliminate the postoperative day 1 fluid balance point from the analyses.
Central venous pressure, mean arterial blood pressure, and the renal near infrared spectroscopy values represent an average of the preceding 24 h.
AKI
AKI was defined as per the Kidney Disease Improving Global Outcomes (KDIGO) serum creatinine to baseline creatinine criteria. As such, AKI was deemed present if the current creatinine to baseline creatinine ratio was greater than or equal to 1.5. AKI was then further stratified by stage using the KDIGO criteria as well. Stage one AKI was present when the current creatinine to baseline creatinine ratio was greater than or equal to 1.5 and less than 2.0; stage two AKI was present when the current creatinine to baseline creatinine was greater than or equal to 2.0 and less than 3.0; and stage three AKI was present when the current creatinine to serum creatinine ratio was greater than 3.0. For this study, the urine output criteria set forth by KDIGO were not utilized. The presence of AKI was determined for each specific postoperative day and then whether it was present in the first 5 postoperative days or not.
Statistical Analysis
Patients were separated into two groups: those with AKI and those without. Distribution of data was assessed by means of kurtosis and skewness. Due to non-normal distribution, continuous variables were reported as median and range while categorical variables were reported as absolute frequency and percent of total.
Spearman correlations were conducted to analyze the correlation between fluid overload percent, blood urea nitrogen, central venous pressure, and fluid balance.
Next, receiver operator curve analyses were run with AKI as the state variable and one of the variables of interest. Receiver operator curve analyses were run using the value of each variable on each individual postoperative day as well as by using the 5-day average. This was done just to determine if a single-day value may have a particularly different effect compared to other days for the same variable. The optimal cutoff point was selected by using the distance furthest from the diagonal reference line.
Next, a logistic regression analysis was conducted with AKI at any point in the study period as the dependent variable and fluid overload, blood urea nitrogen, central venous pressure, fluid balance, mean arterial pressure, serum lactate, renal oxygen extraction ratio, and renal perfusion pressure. Cardiopulmonary bypass time and cross clamp time were also included in the regression. This regression was conducted as a stepwise selection of most informative explanatory variables.
The coefficients from the logistic regression were then used to develop a cumulative AKI risk score. This risk score was then calculated for each patient using the 5-day average values. This was done only for variables found to be statistically significant associated with AKI A receiver operator curve analysis was then done to determine the sensitivity and specificity of the AKI risk score. This receiver operator curve analysis was also used to determine an optimal cutoff.
Finally, the frequency of AKI for specific ranges of AKI risk scores was assessed.
All statistical analyses were done using SPSS Version 23.0. A p-value of less than 0.05 was considered statistically significant. All use of the word “significant”, “significance”, or “significantly” in the manuscript refer to statistical significance unless explicitly specified otherwise.
Results
Cohort Description
A total of 116 patients were included in the final analyses. Of these 49 (42.4%) developed AKI. A majority (77, 66%) of these patients had hypoplastic left heart syndrome. The second most common primary cardiac diagnosis in this cohort was interrupted aortic arch (13, 11%) with the third most common being double inlet left ventricle (6, 5%) and double outlet right ventricle (6, 5%). Only 5 (4%) of these patients had systemic ventricular dysfunction and only 6 (5%) had moderate or greater atrioventricular valve regurgitation.
Average age and weight at the time of Norwood was not significantly different between the two groups. The duration of open chest, duration of mechanical ventilation, need for dialysis, need for extracorporeal membrane oxygenation, and inpatient mortality also did not significantly differ between the two groups (Table 1).
Correlation of Clinical Fluid Balance Markers
Correlation analyses demonstrated significant correlation between blood urea nitrogen and fluid overload percent and fluid balance and fluid overload percent. Despite these correlations being significant, the R-value demonstrated a weak correlation. Table 2 outlines the correlation between the various clinical fluid balance markers.
Association of Clinical and Laboratory Variables with AKI
Fluid overload percent was significantly different between the two groups on postoperative day 5 (Fig. 1). Blood urea nitrogen was significantly different between the two groups on postoperative days 2, 3, 4, and 5 (Fig. 2). Central venous pressure was significantly different between the two groups on postoperative days 2, 3, and 4 (Fig. 3). Fluid balance did not differ at any time point (Fig. 4).
When comparing the 5-day average value for all collected variables, only blood urea nitrogen, central venous pressure, and renal oxygen extraction ratio were significantly different between the two groups (Table 3).
Receiver operator curve analyses for the utility of various clinical and laboratory variables to predict AKI are outlined in Table 4. There was no significant change with time in the area under curve for any of the variables. Fluid overload percent, fluid balance, mean arterial blood pressure, serum lactate, and renal perfusion pressure all demonstrated weak predictive value. Blood urea nitrogen, central venous pressure, renal oxygen extraction ratio, and renal infrared spectroscopy demonstrated moderate predictive value.
Stepwise logistic regression demonstrated the following significant independent associations with AKI: age at Norwood in days (beta coefficient 0.03, p < 0.01), blood urea nitrogen (beta coefficient 0.21, p < 0.01), central venous pressure (beta coefficient 0.37, p = 0.04), and renal oxygen extraction ratio (beta coefficient 1.01, p < 0.01). The resulting equation for the AKI risk score was thus as follows: age in days at Norwood × 0.03 + blood urea nitrogen × 0.21 + central venous pressure × 0.37 + renal oxygen extraction ratio × 1.01.
The mean acute injury risk score was 43.11 in those with AKI group versus 40.45 in those without AKI. Receiver operator curve analysis for the utility of the AKI risk score to predict AKI resulted in an area under the curve of 0.74. A score of 40.87 was found to offer 82% sensitivity and 55% specificity (Table 5).
Those with an AKI risk score of less than 35 had a 15% risk of AKI. Those with a score of greater than or equal to 35 but less than 40 had a 20% risk. Those with a score of greater than or equal to 40 but less than 45 had a 46% risk. Those with a score of greater than or equal to 45 but less than 50 had a 75% risk. Those with a score greater than or equal to 50 had an 80% risk.
Discussion
AKI is a known complication following Norwood operation, and the associations between fluid status and AKI have not been thoroughly described in this high-risk population [4, 5, 8, 11, 15, 17,18,19]. The prevalence of AKI after Norwood operation in our cohort was 42% in the first 5 days following Norwood operation. This finding is similar to a previous study by SooHoo et al. reported a prevalence of 40% in a similar population following Norwood operation [17]. Although the incidence of AKI was high in this cohort, the presence of AKI was not significantly associated with duration of open chest, duration of mechanical ventilation, need for dialysis, need for extracorporeal membrane oxygenation, or inpatient mortality. AKI in this cohort lasted for an average of 1–2 days, suggesting short duration of AKI may not negatively impact outcomes [19].
Fluid overload is a common finding following cardiac surgery and many studies show there is association between fluid overload and poor outcomes [7, 9, 20]. Hazle et al. used fluid balance and daily weight as markers for estimating fluid overload in neonates, however, there is no universally accepted measure for estimating fluid overload and there are limitations to these measures, particularly in critically ill infants in the immediate post-operative period who may be too unstable to accurately weigh and/or may not have accurate intraoperative measures of fluid input and output [20]. The analyses in this study demonstrated that the most used markers of fluid balance did not correlate strongly with one another in this specific population in the immediate postoperative period. While we demonstrated significant correlations between blood urea nitrogen and fluid overload percent and fluid balance and fluid overload percent, the correlations were weak suggesting these markers are not interchangeable.
Because of the poor correlation between metrics used to assess fluid overload, the next question became which would be the most optimal for use. In order to try to better focus this question, the study sought to determine the association of various metrics with AKI. The logic behind this being that fluid overload may mediate poor outcomes by development of AKI. Fluid overload percent, blood urea nitrogen, central venous pressure, and renal oxygen extraction ratio were significantly different between cohorts with and without AKI at different time points, while average blood urea nitrogen, ventral venous pressures, and renal oxygen extraction ratio were significantly higher in the AKI group over the 5-day period. These data suggest that elevated blood urea nitrogen, central venous pressures, and renal oxygen extraction ratio are therefore most significantly independently associated with AKI. These findings that may be consistent with a relatively intravascularly deplete state for the AKI cohort as evidenced by an elevated blood urea nitrogen with a compensatory increase in central venous pressure to increase intravascular pressure and subsequent decrease in renal oxygen delivery.
Renal oxygen delivery had the greatest area under the curve in the receiver operator curve analyses and the greatest beta-coefficient in the multivariable analysis. This is an important finding as it highlights the importance of renal oxygen delivery. Historically, much attention has been paid to renal perfusion pressure. Recent studies, however, have investigated renal oxygen delivery, many utilizing renal near infrared spectroscopy [21,22,23,24,25,26,27,28]. Some studies have noted significant associations between AKI and renal oxygen delivery but not mean arterial pressure or renal perfusion pressure. This should not come as a surprise as volume and pressure metrics are not equal [29]. Just because the pressure in a vessel is higher does not necessarily mean it contains more blood, and subsequently, oxygen. Pressure is the product of flow and resistance so the pressure in a vessel can simply be elevated because resistance is high. Certainly, without knowing what the resistance in the vessel is, pressure cannot be accurately used to assess flow in the vessel. The organs all need oxygen, and it is the cardiovascular system’s goal to simply deliver this oxygen. Pressure is simply the driving force for oxygen-containing blood in the vasculature but does not impact oxygen content itself. Thus, it is should be little surprise that an actual oxygen delivery metric outperforms a pressure metric with respect to kidney function. This has in fact, been demonstrated with mean arterial blood pressure and systemic oxygen delivery as a whole as well [30,31,32,33,34,35].
From the above-mentioned findings, an AKI risk score was developed to identify patients at higher risk for developing AKI in the immediate post-operative period following Norwood operation. Post-operative management of these patients often requires early need for aggressive volume resuscitation, with simultaneous need for diuresis. These conflicting management requirements put this population at particularly high risk for developing AKI and determining patients’ intravascular volume status is often difficult in this particularly high-risk time frame. This score may allow providers to identify patients at high risk for developing AKI at any time point in the postoperative period and adjust management strategies to prevent development of AKI during this time period.
Such preventive strategies are currently limited although a network meta-analysis identified milrinone, levosimendan, and aminophylline may provide protective benefit. Placed in the context of the findings of this study, optimization of renal oxygen delivery appears to be of importance as has been demonstrated by other studies. Being able to identify those at high-risk for AKI can help design studies investigating preventive strategies whether they be perioperative strategies, pharmacologic, or procedural [36,37,38,39,40,41,42].
Limitations of this study include its single-center, retrospective design, which may not account for site-specific and other unaccounted variables that are not reproducible. Prospective application and implantation at other institutions could validate this scoring system and improve utility. Additionally, the cohort is large, but there is likely era effect due to the 10-year interval. The frequency of mortality was also low, which limits statistical power of our findings that there was no significant association between AKI and mortality. Another limitation is that AKI was treated as a binary outcome and thus a logistic regression was done rather than a time-dependent analysis.
Conclusion
Various clinical metrics used to assess fluid overload have poor correlation in those who have undergone a Norwood operation. Blood urea nitrogen, central venous pressure, and renal oxygen extraction ratio, however, are associated with AKI after the Norwood operation.
References
Alten JA, Cooper DS, Blinder JJ, Selewski DT, Tabbutt S, Sasaki J, Gaies MG, Bertrandt RA, Smith AH, Reichle G, Gist KM, Banerjee M, Zhang W, Hock KM, Borasino S, Neonatal PH, Renal Outcomes Network I (2021) Epidemiology of AKI after neonatal cardiac surgery: a report from the multicenter neonatal and pediatric heart and renal outcomes network. Crit Care Med 49:e941–e951
Bellos I, Iliopoulos DC, Perrea DN (2020) Association of postoperative fluid overload with adverse outcomes after congenital heart surgery: a systematic review and dose-response meta-analysis. Pediatr Nephrol 35:1109–1119
Blinder JJ, Goldstein SL, Lee VV, Baycroft A, Fraser CD, Nelson D, Jefferies JL (2012) Congenital heart surgery in infants: effects of AKI on outcomes. J Thorac Cardiovasc Surg 143:368–374
Cunningham TW, Tan Y, Krawczeski CD, Spencer JD, Bai S, Phelps C, Yates AR (2021) Incidence and impact of AKI in patients with hypoplastic left heart syndrome following the hybrid stage 1 palliation. Cardiol Young 31:414–420
Girgis A, Millar J, Butt W, d’Udekem Y, Namachivayam SP (2020) Peak creatinine, cardiopulmonary bypass, and mortality after stage 1 single-ventricle reconstruction. Ann Thorac Surg 109:1488–1494
Hassinger AB, Wald EL, Goodman DM (2014) Early postoperative fluid overload precedes AKI and is associated with higher morbidity in pediatric cardiac surgery patients. Pediatr Crit Care Med 15:131–138
Lex DJ, Toth R, Czobor NR, Alexander SI, Breuer T, Sapi E, Szatmari A, Szekely E, Gal J, Szekely A (2016) Fluid overload is associated with higher mortality and morbidity in pediatric patients undergoing cardiac surgery. Pediatr Crit Care Med 17:307–314
Loomba RS, Rausa J, Farias JS, Villarreal EG, Acosta S, Savorgnan F, Flores S (2022) Impact of medical interventions and comorbidities on Norwood admission for patients with hypoplastic left heart syndrome. Pediatr Cardiol 43:267–278
Mah KE, Hao S, Sutherland SM, Kwiatkowski DM, Axelrod DM, Almond CS, Krawczeski CD, Shin AY (2018) Fluid overload independent of AKI predicts poor outcomes in neonates following congenital heart surgery. Pediatr Nephrol 33:511–520
Seguin J, Albright B, Vertullo L, Lai P, Dancea A, Bernier PL, Tchervenkov CI, Calaritis C, Drullinsky D, Gottesman R, Zappitelli M (2014) Extent, risk factors, and outcome of fluid overload after pediatric heart surgery. Crit Care Med 42:2591–2599
SooHoo M, Griffin B, Jovanovich A, Soranno DE, Mack E, Patel SS, Faubel S, Gist KM (2018) AKI is associated with subsequent infection in neonates after the Norwood procedure: a retrospective chart review. Pediatr Nephrol 33:1235–1242
Pande CK, Noll L, Afonso N, Serrano F, Monteiro S, Guffey D, Puri K, Achuff BJ, Akcan-Arikan A, Shekerdemian L (2022) Neurodevelopmental outcomes in infants with cardiac surgery associated AKI. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2022.03.020
Van den Eynde J, Rotbi H, Gewillig M, Kutty S, Allegaert K, Mekahli D (2021) In-hospital outcomes of AKI after pediatric cardiac surgery: a meta-analysis. Front Pediatr 9:733744
Wilder NS, Yu S, Donohue JE, Goldberg CS, Blatt NB (2016) Fluid overload is associated with late poor outcomes in neonates following cardiac surgery. Pediatr Crit Care Med 17:420–427
Wong JH, Selewski DT, Yu S, Leopold KE, Roberts KH, Donohue JE, Ohye RG, Charpie JR, Goldberg CS, DeWitt AG (2016) Severe AKI following stage 1 Norwood palliation: effect on outcomes and risk of severe AKI at subsequent surgical stages. Pediatr Crit Care Med 17:615–623
Wu Y, Hua X, Yang G, Xiang B, Jiang X (2020) Incidence, risk factors, and outcomes of AKI in neonates after surgical procedures. Pediatr Nephrol 35:1341–1346
SooHoo MM, Patel SS, Jaggers J, Faubel S, Gist KM (2018) AKI defined by fluid corrected creatinine in neonates after the Norwood procedure. World J Pediatr Congenit Heart Surg 9:513–521
Garcia RU, Natarajan G, Walters HL, Delius RE, Aggarwal S (2018) AKI following first-stage palliation in hypoplastic left heart syndrome: hybrid versus Norwood palliation. Cardiol Young 28:261–268
Gist KM, Borasino S, SooHoo M, Soranno DE, Mack E, Hock KM, Rahman A, Brinton JT, Basu RK, Alten JA (2022) Transient and persistent AKI phenotypes following the Norwood operation: a retrospective study. Cardiol Young 32:564–571
Hazle MA, Gajarski RJ, Yu S, Donohue J, Blatt NB (2013) Fluid overload in infants following congenital heart surgery. Pediatr Crit Care Med 14:44–49
Adams PS, Vargas D, Baust T, Saenz L, Koh W, Blasiole B, Callahan PM, Phadke AS, Nguyen KN, Domnina Y, Sharma M, Kellum JA, Sanchez-de-Toledo J (2019) Associations of perioperative renal oximetry via near-infrared spectroscopy, urinary biomarkers, and postoperative AKI in infants after congenital heart surgery: should creatinine continue to be the gold standard? Pediatr Crit Care Med 20:27–37
Ruf B, Bonelli V, Balling G, Horer J, Nagdyman N, Braun SL, Ewert P, Reiter K (2015) Intraoperative renal near-infrared spectroscopy indicates developing AKI in infants undergoing cardiac surgery with cardiopulmonary bypass: a case-control study. Crit Care 19:27
Zhang Y, Zhou X, Wang B, Guo L, Zhou R (2020) Goal-directed perfusion to reduce AKI after paediatric cardiac surgery (GDP-AKIp): study protocol for a prospective randomised controlled trial. BMJ Open 10:e039385
Zhang Y, Wang B, Zhou XJ, Guo LJ, Zhou RH (2022) Nadir oxygen delivery during pediatric bypass as a predictor of AKI. Ann Thorac Surg 113:647–653
Gist KM, Kaufman J, da Cruz EM, Friesen RH, Crumback SL, Linders M, Edelstein C, Altmann C, Palmer C, Jalal D, Faubel S (2016) A decline in intraoperative renal near-infrared spectroscopy is associated with adverse outcomes in children following cardiac surgery. Pediatr Crit Care Med 17:342–349
Neunhoeffer F, Wiest M, Sandner K, Renk H, Heimberg E, Haller C, Kumpf M, Schlensak C, Hofbeck M (2016) Non-invasive measurement of renal perfusion and oxygen metabolism to predict postoperative AKI in neonates and infants after cardiopulmonary bypass surgery. Br J Anaesth 117:623–634
Flechet M, Guiza F, Scharlaeken I, Vlasselaers D, Desmet L, Van den Berghe G, Meyfroidt G (2019) Near-infrared-based cerebral oximetry for prediction of severe AKI in critically ill children after cardiac surgery. Crit Care Explor 1:e0063
Harer MW, Chock VY (2020) Renal tissue oxygenation monitoring—an opportunity to improve kidney outcomes in the vulnerable neonatal population. Front Pediatr 8:241
Loomba RS, Flores S, Bronicki RA (2022) When volume and pressure are not equal. Pediatr Crit Care Med 23:333–334
Tweddell JS, Ghanayem NS, Mussatto KA, Mitchell ME, Lamers LJ, Musa NL, Berger S, Litwin SB, Hoffman GM (2007) Mixed venous oxygen saturation monitoring after stage 1 palliation for hypoplastic left heart syndrome. Ann Thorac Surg 84:1301–1310 (discussion 1310-1311)
Tweddell JS, Hoffman GM, Fedderly RT, Ghanayem NS, Kampine JM, Berger S, Mussatto KA, Litwin SB (2000) Patients at risk for low systemic oxygen delivery after the Norwood procedure. Ann Thorac Surg 69:1893–1899
Hoffman GM, Ghanayem NS, Scott JP, Tweddell JS, Mitchell ME, Mussatto KA (2017) Postoperative cerebral and somatic near-infrared spectroscopy saturations and outcome in hypoplastic left heart syndrome. Ann Thorac Surg 103:1527–1535
Hoffman GM, Ghanayem NS, Kampine JM, Berger S, Mussatto KA, Litwin SB, Tweddell JS (2000) Venous saturation and the anaerobic threshold in neonates after the Norwood procedure for hypoplastic left heart syndrome. Ann Thorac Surg 70:1515–1520 (discussion 1521)
Bronicki RA, Acosta S, Savorgnan F, Flores S, Achuff BJ, Loomba RS, Ahmed M, Ghanayem N, Heinle JS, Asadourian V, Lasa JJ (2022) The acute impact of vasopressin on hemodynamics and tissue oxygenation following the Norwood procedure. JTCVS Open. https://doi.org/10.1016/j.xjon.2022.01.008
Loomba RS, Culichia C, Schulz K, Vogel M, Savorgnan F, Flores S, Bronicki RA (2021) Acute effects of vasopressin arginine infusion in children with congenital heart disease: higher blood pressure does not equal improved systemic oxygen delivery. Pediatr Cardiol 42:1792–1798
Jahnukainen T, Keski-Nisula J, Tainio J, Valkonen H, Patila T, Jalanko H, Suominen P (2018) Efficacy of corticosteroids in prevention of AKI in neonates undergoing cardiac surgery—a randomized controlled trial. Acta Anaesthesiol Scand. https://doi.org/10.1111/aas.13134
Van den Eynde J, Cloet N, Van Lerberghe R, Sa M, Vlasselaers D, Toelen J, Verbakel JY, Budts W, Gewillig M, Kutty S, Pottel H, Mekahli D (2021) Strategies to prevent AKI after pediatric cardiac surgery: a network meta-analysis. Clin J Am Soc Nephrol 16:1480–1490
Reagor JA, Clingan S, Gao Z, Morales DLS, Tweddell JS, Bryant R, Young W, Cavanaugh J, Cooper DS (2020) Higher flow on cardiopulmonary bypass in pediatrics is associated with a lower incidence of AKI. Semin Thorac Cardiovasc Surg 32:1015–1020
Tadphale SD, Ramakrishnan K, Spentzas T, Kumar TKS, Allen J, Staffa SJ, Zurakowski D, Bigelow WA, Gopal SH, Boston US, Jonas RA, Knott-Craig CJ (2021) Impact of different cardiopulmonary bypass strategies on renal injury after pediatric heart surgery. Ann Thorac Surg 111:1374–1379
Van Driest SL, Jooste EH, Shi Y, Choi L, Darghosian L, Hill KD, Smith AH, Kannankeril PJ, Roden DM, Ware LB (2018) Association between early postoperative acetaminophen exposure and AKI in pediatric patients undergoing cardiac surgery. JAMA Pediatr 172:655–663
Wang H, Luo Q, Li Y, Zhang L, Wu X, Yan F (2020) Effect of prophylactic levosimendan on all-cause mortality in pediatric patients undergoing cardiac surgery—an updated systematic review and meta-analysis. Front Pediatr 8:456
Yavuz Y, Isildak FU (2022) Effect of intraoperative theophylline use on AKI in paediatric cardiac surgery. Cardiol Young. https://doi.org/10.1017/S1047951122000245
Acknowledgements
None.
Funding
No sources of funding to report.
Author information
Authors and Affiliations
Contributions
RL and JW were responsible for study design. JW performed data collection. RL performed data analysis and prepared figures and tables. JW and RL wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors have disclosed that they do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Weld, J., Kim, E., Chandra, P. et al. Fluid Overload and AKI After the Norwood Operation: The Correlation and Characterization of Routine Clinical Markers. Pediatr Cardiol 45, 1440–1447 (2024). https://doi.org/10.1007/s00246-023-03167-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-023-03167-0