Abstract
A non-contractile transannular patch (TAP) in the right ventricular outflow tract (RVOT) contributes to ventricular dysfunction after tetralogy of Fallot (TOF) repair. We compared regional right ventricular (RV) strain in repaired TOF with valvar pulmonary stenosis (VPS) after balloon valvuloplasty to investigate the effects of TAP. Retrospective review of 26 cardiac magnetic resonance studies of TOF (n = 13) and VPS (n = 13) subjects matched by degree and duration of pulmonary regurgitation (PR). Feature tracking strain analysis was performed. Student’s t tests, Pearson correlation, and linear regression were applied. RV ejection fraction (EF) was normal and similar between TOF and VPS (60 and 65%, respectively, p = 0.8). RV 4-chamber Lagrangian longitudinal strain (RV 4ch LS) was worse in both groups compared to normals but comparable to each other: −18.2 (95% CI −3.6 to −33) for TOF and −20.2 (95% CI −12.4 to −28) for VPS, p = 0.5. RVOT LS was worse than RV 4ch LS in TOF, p = 0.05, but not in VPS, p = 0.19. There were no significant differences in RVOT strain between groups, p = 0.18. RVOT strain and RV 4ch LS correlated positively with RV EF in VPS (r = 0.72, p = 0.003 and r = 0.55, p = 0.04). PR degree correlated negatively with RVOT LS for TOF and VPS. Longitudinal strain is diminished in VPS and TOF subjects with preserved RV EF. TAP could explain worse RVOT strain in TOF. Longitudinal studies are needed to ascertain if RV strain predicts worsening of RV EF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Outcomes in tetralogy of Fallot (TOF) are in part determined by residual pulmonary regurgitation (PR) following repair, usually with placement of a transannular and/or right ventricular outflow tract (RVOT) patch. With time, PR results in right ventricular (RV) dilation and eventually ventricular dysfunction in many patients. A non-contractile patch in the RV outflow tract has been associated with RV systolic dysfunction [1] although specific effects of the RVOT patch on regional RV function have not been completely defined. 2D strain analysis by cardiac magnetic resonance (CMR) is a robust technique for evaluating regional cardiac function [2]. We aimed to characterize regional RV systolic function using feature tracking strain analysis (FTS) by comparing patients with repaired TOF and RVOT patch to patients with valvar pulmonary stenosis (VPS) after balloon dilation valvuloplasty, who do not have RVOT patches. We hypothesized that even after matching for duration and severity of PR, there would be differences in regional function between the two groups that might be related to the presence of an RVOT patch.
Materials and Methods
This study was approved by The Children’s Hospital of Philadelphia Institutional Review Board for the Protection of Human Subjects.
Study Population
Subjects 8–18 years with surgically repaired TOF or VPS after balloon valvuloplasty were identified. These subjects had previously participated in a cross-sectional study for whom protocol-based CMRs were available and had provided informed consent at enrollment [3, 4]. Subjects were matched by duration and severity of PR using propensity scores. Severity of PR was defined by regurgitant fraction (RF) and considered mild if ≤20%, moderate if 20–40%, and severe if >40%. Duration of PR was defined as the time (years) between initial procedure (complete repair for TOF or balloon valvuloplasty for VPS) and CMR. Residual RVOT obstruction may have an effect on strain; thus, subjects with RVOT peak velocity >2 m/sec were excluded.
CMR: CMR studies were performed as part of a study protocol on a Siemens 1.5-Tesla Avanto Whole-Body Magnetic Resonance system (Siemens Medical Solutions, Malvern, Pennsylvania) using a standardized protocol, previously published by our group (Table 1) [5]. Balanced steady-state free-precession (SSFP) cine CMR acquisitions were obtained in 4-chamber and long-axis planes and contiguous short-axis cine imaging from the atrioventricular junction through the cardiac apex. A cine SSFP sequence in the short-axis view was used (TE/TR 2.0/45 ms; flip angle 75°–90°; matrix size 196 × 196) to assess ventricular end-systolic and end-diastolic volumes (ESV, EDV). The RV infundibulum was included in the RV volume up to the pulmonary annulus. Balanced SSFP cines were analyzed using standard Siemens analysis software (Argus) for ventricular volumes and function. RV ejection fraction (EF) was calculated as [(EDV − ESV)/EDV] × 100 (in %). Phase-contrast velocity mapping with a flow-sensitive, gradient-echo sequence was performed in the main pulmonary artery to assess the RF. CMR variables included RVEF, RV EDV, and RV ESV, and pulmonary RF. For RV volumetric calculations, the endocardial contour included the RVOT region. Trabeculations were included within the RV cavity. All volumes were indexed to body surface area, and corresponding z-scores were calculated using published normative data [6, 7].
RV Strain Measurements on CMR
Feature tracking strain analysis of SSFP cines was performed on the RV in 4-chamber long axis (4ch) and sagittal RVOT views to yield RV 4ch LS and RVOT LS (Fig. 1 and Online Supplemental Video 1). Strain measurements were performed with 2D Cardiac Performance Analysis (TomTec 2D CPA, v1.0, Munich, Germany). 2D CPA is a vector-based method that performs strain analysis via feature tracking techniques, as previously described [8]. A contour was applied by a single trained reader (SA) along the RV endocardial border, and the software automatically propagated the contour by following its features through the remainder of the cardiac cycle. The 4ch RV contour included the RV free wall and ventricular septum. The tracing was visually inspected to ensure adequate tracking. Studies with poor tracking of the endocardium were excluded. The FTS software-derived parameters of ventricular function including strain, strain rate, tissue velocity, and displacement. Validation of this analysis system has been previously reported against harmonic phase tagged MRI [8]. By convention, longitudinal strain is expressed as a negative value; therefore, a higher negative number indicates greater LS and therefore better systolic function. Normal longitudinal strain was defined as >−29% in the RV 4ch view [9]. Strain at the RVOT was derived to perform comparisons between groups. To our knowledge, normal values for RVOT strain have not been defined in the literature.
Statistical Analysis
Variables are presented as mean, and categorical variables as counts (percentages). The data were normally distributed; thus, two-tailed paired Student’s t tests were applied to evaluate differences between groups. Pearson correlation was used to assess relationships between variables. The absolute value of RV strain was used to compare the magnitude of strain to PR, RV volumes, and RV EF. Statistical significance was reached for p values <0.05. Statistical analyses were performed using Stata 11.2 (Stata Corporation, College Station, Texas).
Results
Demographics, Pulmonary Regurgitation, RV Volume, and Ejection Fraction
There were 26 subjects in the study: 13 matched pairs of TOF and VPS. There were no significant differences between the TOF and VPS groups in age, body surface area (BSA), RV volumes (indexed to BSA), and RV ejection fraction (Table 2). By study design, duration and severity of PR were comparable between the two groups. RV ejection fraction was normal in both groups (Table 2).
Region-Specific RV Strain
RV LS from the 4-chamber view (RV 4ch LS) was diminished in the TOF and VPS groups compared to published normals (Table 2) [9]. There was no significant difference in RVOT or RV 4ch LS in the TOF group as compared to the VPS group (Table 2). Strain at the RVOT was worse than RV 4ch LS in the TOF group, p = 0.05. In contrast, there was no difference between RVOT and RV 4ch LS in the VPS group, p = 0.19 (Table 3).
Associations of RV Strain with Severity of PR, RV Volumes, and RV Function
Severity of PR:We found a moderate negative correlation between RVOT LS and severity of PR (as quantified by regurgitant fraction) in both groups, suggesting that RVOT strain is worse with more severe PR (Table 4; Fig. 2).
Linear regression of absolute longitudinal strain at the right ventricular outflow tract (RVOT LS) versus pulmonary valve regurgitant reaction (RF) Tetralogy of Fallot (left panel) and valvar pulmonary stenosis (right panel). There is a negative correlation between pulmonary valve RF and RVOT LS, r = −0.55 (p = 0.04) in TOF and r = −0.57 (p = 0.03) in VPS
Indexed RV Volumes: Absolute RVOT LS had a moderate negative correlation with indexed RV end-systolic volume in the VPS group (p = 0.03). A similar trend was noted in TOF although this did not reach statistical significance (Table 4; Fig. 3). There were no significant relationships between RVOT strain and indexed end-diastolic volumes.
Linear regression of absolute longitudinal strain at the right ventricular outflow tract (RVOT LS) versus RV end-systolic volume (indexed to BSA) Tetralogy of Fallot (left panel) and valvar pulmonary stenosis (right panel). There is a negative correlation between RV ESVi and RVOT LS, r = −0.53 (p = 0.05) in TOF and r = −0.58 (p = 0.03) in VPS
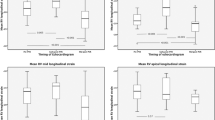
RV Ejection Fraction:For the VPS group, the absolute RVOT strain had a strong positive correlation with RV EF and the 4ch LS had a moderate correlation with RVEF. These associations were not significant in the TOF group (Table 4; Fig. 4).
Linear regression of RV ejection fraction (EF) versus absolute longitudinal strain at the right ventricular outflow tract (RVOT LS) Tetralogy of Fallot (left panel) and valvar pulmonary stenosis (right panel). There is a positive correlation between RV EF and RVOT LS in VPS r = 0.72 (p = 0.003) but not in TOF r = 0.55 (p = 0.06)
Discussion
The goal of this study was to evaluate right ventricular systolic function and in particular to assess the right ventricular outflow tract (RVOT), in an attempt to evaluate the contribution of the RVOT patch to RV function in patients with Tetralogy of Fallot following repair. Specifically, the hypothesis was that patients with an RVOT patch would have worse systolic function quantified by strain as compared to patients with valvar pulmonary stenosis treated with a catheter-based intervention and therefore without an RVOT patch. Our study did not find a difference in strain in the RVOT in the two groups. At the same time, the study did find that in the TOF group, RVOT strain is worse compared to other regions in the RV, which did not occur in the VPS group.
Reduced RV function in TOF patients has been reported in several studies [10–14], and RV volumes and function stand out as the strongest independent factors associated with clinical outcome [15, 16]. Orwat et al. recently reported that RV strain measured on cardiac MRI using the FTS method was an independent predictor of clinical outcome in TOF patients [17]. In our study, RV strain was reduced in both the TOF and VPS groups, whereas ejection fraction by conventional CMR measurements was normal. This finding suggests that even mild PR can be associated with RV dysfunction measured by strain. While TOF as a group is well recognized to have RV dysfunction, it is noteworthy that VPS patients with mild residual PR and preserved EF may have subtle abnormalities in RV function as detected by strain. These findings suggest that both groups should be followed with measures that are more sensitive to detect abnormalities in function than ejection fraction. It is possible that strain could serve as an early indicator of dysfunction given that it is abnormal prior to overt changes in ejection fraction [18–21]. Similar to our results, Luijnenburg et al. studied patients with valvar pulmonary stenosis and TOF and reported comparable RV ejection fractions between the two groups, even though the TOF group had more severe pulmonary regurgitation and more dilated right ventricles [1]. This finding suggests that their pump function is comparable, but does not provide information on contractility, since ejection fraction does not identify the abnormal myocardial mechanics that may exist between different pathological states affecting the RV. Puranik et al. previously reported significantly diminished RV systolic function (by EF) and larger end-systolic volumes in TOF subjects compared to VPS [22] and postulated that patients with a non-contractile RVOT have reduced overall RV function compared to those with contractile RVOTs. We demonstrate that strain can be diminished in the RVOT in comparison to the rest of the RV in TOF patients. This suggests that strain may be reported as a complementary parameter of function in the assessment of RV systolic function in this patient population.
In this study, strain was reduced at the RVOT as compared to 4ch longitudinal strain which did not include the RVOT in the TOF group. This is likely due to the presence of a non-contractile (and sometimes aneurysmal) RVOT patch in patients with TOF. Prior studies have also reported diminished RVOT function in the TOF population using different techniques [23]. RVOT fibrosis appears to contribute to RVOT dysfunction, which in turn is associated with overall RV dysfunction [24, 25]. These studies suggest that the RVOT patch has a negative impact on overall ventricular function and therefore inform our understanding of regional RV dysfunction. RVOT fibrosis and dysfunction have been specifically linked to clinical outcomes in patients following TOF repair. Babu-Narayan et al. reported late gadolinium enhancement (LGE) indicating fibrosis or scar at surgical sites in the RVOT in 99% of patients following TOF repair. Patients with increased fibrosis or scarring had increased biomarkers of myocardial stretch, exercise intolerance, and RV dysfunction [24]. Wald et al. reported that RVOT dyskinesis and higher LGE score correlated significantly with worse RV EF and lower aerobic exercise capacity [25].
Worse RVOT strain was associated with greater pulmonary regurgitation in both the TOF and VPS groups. A similar finding was reported in asymptomatic children after TOF repair, although the study did not examine differences in RVOT strain [26]. Reduced RVOT strain was associated with greater PR in both TOF and VPS groups. It is possible that PR has a negative impact in the contractile properties of the RVOT even in patients without an RVOT patch, or alternatively, worse PR is a reflection of disease severity and therefore is associated with worse RVOT strain. Further study is needed to corroborate this idea.
Finally, this study demonstrates a useful application of feature tracking strain, a technique that can be used in patients with congenital heart disease without adding to the length of the MRI study. FTS has been validated against grid-tagging (spatial modulation of magnetization, SPAMM), the current gold-standard for non-invasive strain assessment [8]. From a technical standpoint, FTS can analyze the thin-walled RV, which has been challenging with SPAMM, and has the potential for widespread application in a number of right-heart disease states. One of the potential benefits of FTS could be the ability to identify subclinical dysfunction in patients with preserved ejection fraction, which has been demonstrated in other disease states, such as cardiomyopathy following exposure to cardio toxic agents [18–21]. Sensitive detection of subclinical dysfunction may become particularly useful in the longitudinal follow-up of patients with repaired TOF, VPS as well as in other forms of congenital and acquired heart disease.
Conclusions and Limitations
We studied a relatively healthy population with mild PR and preserved EF with a small sample size. In particular, the difference in RVOT and 4ch longitudinal strain in the TOF group barely reached statistical significance. However, our findings are of interest given the presence of diminished strain in patients with a relatively normal ejection fraction, and could be more pronounced in a larger sample size and/or in patients with more significant PR or decreased RV EF. Although adverse RV–LV interactions have been noted in patients with dysfunctional RVs, this association was not evaluated in this study. A follow-up study could investigate the effects of RV dysfunction on LV strain.
In conclusion, strain is diminished even in the presence of mild pulmonary regurgitation and preserved ejection fraction. If longitudinal studies confirm that abnormal strain predicts a subsequent drop in RV EF in this setting, then strain might become a sensitive tool to detect right ventricular dysfunction premorbidly. Either way, measures of RV strain would appear to be a useful tool with which to assess RV function concurrently with other measurements. Finally, the role of RVOT dysfunction merits further investigation and longitudinal studies are warranted to further validate its use.
Abbreviations
- PR:
-
Pulmonary regurgitation
- TOF:
-
Tetralogy of Fallot
- RV:
-
Right ventricle
- TAP:
-
Transannular patch
- RVOT:
-
Right ventricular outflow tract
- VPS:
-
Valvar pulmonary stenosis
- CMR:
-
Cardiac magnetic resonance
- PR:
-
Pulmonary regurgitation
- FTS:
-
Feature tracking strain
- 4ch:
-
4-chamber
- LS:
-
Longitudinal strain
- EF:
-
Ejection fraction
- SSFP:
-
Steady-state free-precession
- ESV:
-
End-systolic volume
- EDV:
-
End-diastolic volume
- RF:
-
Regurgitant fraction
- CPA:
-
Cardiac performance analysis
- HARP:
-
Harmonic phase
- BSA:
-
Body surface area
- LGE:
-
Late gadolinium enhancement
- SPAMM:
-
Spatial modulation of magnetization
References
Luijnenburg SE, de Koning WB, Romeih S et al (2012) Exercise capacity and ventricular function in patients treated for isolated pulmonary valve stenosis or Tetralogy of Fallot. Int J Cardiol 158:359–363. doi:10.1016/j.ijcard.2011.01.038
Hor KN, Wansapura JP, Al-Khalidi HR et al (2011) Presence of mechanical dyssynchrony in Duchene muscular dystrophy. J Cardiovasc Magn Reson 13:12. doi:10.1186/1532-429X-13-12
Mercer-Rosa L, Paridon SM, Fogel MA et al (2015) 22q11.2 deletion status and disease burden in children and adolescents with Tetralogy of Fallot. Circulation 8:74–81. doi:10.1161/CIRCGENETICS.114.000819
Mercer-Rosa L, Ingall E, Zhang X et al (2014) The impact of pulmonary insufficiency on the right ventricle: a comparison of isolated valvar pulmonary stenosis and Tetralogy of Fallot. Pediatr Cardiol 36:796–801. doi:10.1007/s00246-014-1087-z
Mercer-Rosa L, Yang W, Kutty S et al (2012) Quantifying pulmonary regurgitation and right ventricular function in surgically repaired tetralogy of Fallot: a comparative analysis of echocardiography and magnetic resonance imaging. Circulation 5:637–643. doi:10.1161/CIRCIMAGING.112.972588
Sarikouch S, Peters B, Gutberlet M et al (2010) Sex-Specific pediatric percentiles for ventricular size and mass as reference values for cardiac MRI: assessment by steady-state free-precession and phase-contrast MRI flow. Circulation 3:65–76. doi:10.1161/CIRCIMAGING.109.859074
Robbers Visser D, Boersma E, Helbing WA (2009) Normal biventricular function, volumes, and mass in children aged 8 to 17 years. J Magn Reson Imaging 29:552–559. doi:10.1002/jmri.21662
Hor KN, Gottliebson WM, Carson C et al (2010) Comparison of magnetic resonance feature tracking for strain calculation with harmonic phase imaging analysis. J Am Coll Cardiol 3:144–151. doi:10.1016/j.jcmg.2009.11.006
Levy PT, Sanchez Mejia AA, Machefsky A et al (2014) Normal ranges of right ventricular systolic and diastolic strain measures in children: a systematic review and meta-analysis. J Am Soc Echocardiogr 27(549–560):e3. doi:10.1016/j.echo.2014.01.015
Solarz DE, Witt SA, Glascock BJ et al (2004) Right ventricular strain rate and strain analysis in patients with repaired Tetralogy of Fallot: possible interventricular septal compensation. J Am Soc Echocardiogr 17:338–344. doi:10.1016/j.echo.2004.01.012
Weidemann F, Eyskens B, Jamal F et al (2002) Quantification of regional left and right ventricular radial and longitudinal function in healthy children using ultrasound-based Strain Rate and Strain Imaging. J Am Soc Echocardiogr 15:20–28. doi:10.1067/mje.2002.116532
Kowalik E, Kowalski M, Różański J et al (2011) The impact of pulmonary regurgitation on right ventricular regional myocardial function: an echocardiographic study in adults after total repair of Tetralogy of Fallot. J Am Soc Echocardiogr 24:1199–1204. doi:10.1016/j.echo.2011.08.008
van der Hulst AE, Delgado V, Holman ER et al (2010) Relation of left ventricular twist and global strain with right ventricular dysfunction in patients after operative “correction” of Tetralogy of Fallot. Am J Cardiol 106:723–729. doi:10.1016/j.amjcard.2010.04.032
Lu JC, Ghadimi Mahani M, Agarwal PP et al (2013) Usefulness of right ventricular free wall strain to predict quality of life in “repaired” Tetralogy of Fallot. Am J Cardiol 111:1644–1649. doi:10.1016/j.amjcard.2013.01.336
Geva T (2011) Repaired Tetralogy of Fallot: the roles of cardiovascular magnetic resonance in evaluating pathophysiology and for pulmonary valve replacement decision support. J Cardiovasc Magn Reson 13:9. doi:10.1186/1532-429X-13-9
Knauth AL, Gauvreau K, Powell AJ et al (2008) Ventricular size and function assessed by cardiac MRI predict major adverse clinical outcomes late after Tetralogy of Fallot repair. Heart 94:211–216. doi:10.1136/hrt.2006.104745
Orwat S, Diller G-P, Kempny A et al (2016) Myocardial deformation parameters predict outcome in patients with repaired Tetralogy of Fallot. Heart 102:209–215. doi:10.1136/heartjnl-2015-308569
Toro-Salazar OH, Gillan E, O’Loughlin MT et al (2013) Occult cardiotoxicity in childhood cancer survivors exposed to anthracycline therapy. Circulation 6:873–880. doi:10.1161/CIRCIMAGING.113.000798
Sawaya H, Sebag IA, Plana JC et al (2011) Early detection and prediction of cardiotoxicity in chemotherapy-treated patients. Am J Cardiol 107:1375–1380. doi:10.1016/j.amjcard.2011.01.006
Negishi K, Negishi T, Hare JL et al (2013) Independent and incremental value of deformation indices for prediction of trastuzumab-induced cardiotoxicity. J Am Soc Echocardiogr 26:493–498. doi:10.1016/j.echo.2013.02.008
Thavendiranathan P, Poulin F, Lim K-D et al (2014) Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol 63:2751–2768. doi:10.1016/j.jacc.2014.01.073
Puranik R, Tsang V, Lurz P et al (2012) Long-term importance of right ventricular outflow tract patch function in patients with pulmonary regurgitation. J Thorac Cardiovasc Surg 143:1103–1107. doi:10.1016/j.jtcvs.2011.09.039
Menteer J, Weinberg P, Fogel M (2005) Quantifying regional right ventricular function in Tetralogy of Fallot. J Cardiovasc Magn Reson 7:753–761. doi:10.1080/10976640500283439
Babu-Narayan SV, Kilner PJ, Li W et al (2006) Ventricular fibrosis suggested by cardiovascular magnetic resonance in adults with repaired Tetralogy of Fallot and its relationship to adverse markers of clinical outcome. Circulation 113:405–413. doi:10.1161/CIRCULATIONAHA.105.548727
Wald RM, Haber I, Wald R et al (2009) Effects of regional dysfunction and late gadolinium enhancement on global right ventricular function and exercise capacity in patients with repaired Tetralogy of Fallot. Circulation 119:1370–1377. doi:10.1161/CIRCULATIONAHA.108.816546
Eyskens B, Brown SC, Claus P et al (2010) The influence of pulmonary regurgitation on regional right ventricular function in children after surgical repair of Tetralogy of Fallot. Eur J Echocardiogr 11:341–345. doi:10.1093/ejechocard/jep209
Funding
The funding was provided by Children’s Hospital of Philadelphia (US), National Institutes of Health (Grant No. 3U01HL098153-03S1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Mark A. Fogel and Laura Mercer-Rosa are Co-senior authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Anwar, S., Harris, M.A., Whitehead, K.K. et al. The Impact of the Right Ventricular Outflow Tract Patch on Right Ventricular Strain in Tetralogy of Fallot: A Comparison with Valvar Pulmonary Stenosis Utilizing Cardiac Magnetic Resonance. Pediatr Cardiol 38, 617–623 (2017). https://doi.org/10.1007/s00246-016-1558-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-016-1558-5