Abstract
This retrospective study aimed to evaluate whether there was still a place for ESWL therapy in the endourological era. From 1988 to 2018, ESWL therapy was performed with 3 successive types of lithotripters in our hospital. From 1988 to 1998, the electrohydraulic lithotripter NS-15 was used, and the electromagnetic lithotripter HK-V was put to use in 1999. Since 2010, the electromagnetic lithotripter HK-Vm has been used. Over the 30-year period, 16,969 urolithiasis patients underwent ESWL therapy, including 124 paediatric cases and 178 special cases. The stone clearance rate (SCR) and postoperative complications in the 3 lithotripter groups were recorded and analysed. The SCR was estimated by ultrasonography or plain X-ray, while the complications were recorded by the modified Clavien grading system. The primary stone clearance rate (pSCR) of ureteral and renal stones was significantly improved in the HK-Vm group compared with the NS-15 and HK-V groups. The final stone clearance rate (fSCR) of lower calyx stones was considerably higher in the HK-Vm group (55.9%) than in the NS-15 (41.1%) and HK-V (44.1%) groups. Most complications were grade I and II, while the incidence of grade III and above complications was less than 3%. Additionally, the fSCR in paediatric and special cases ranged from 66.5% to 83.5%, with no record of severe complications. As our data showed, ESWL was effective and safe for most urolithiasis patients, including paediatric patients and special cases. Therefore, ESWL is still the major treatment option in the current endourological era.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
ESWL, one of the main treatments for urolithiasis, is widely used in China; however, its use is increasingly challenged by the rapid development of endourological technologies such as flexible ureteroscopy (FUR) and percutaneous nephrostolithotomy (PCNL). These endourological technologies are becoming the preferred choice for treating urinary stones in an increasing number of medical centres [1, 2]. Many urologists and patients prefer FUR or PCNL to ESWL therapy. Thus, the status of ESWL therapy has been questioned in the present endourological era. Moreover, ESWL is no longer used in some Chinese hospitals. As one of the earliest medical centres in China, our hospital began to perform ESWL therapy in 1988. Over the 30-year period from 1988 to 2018, we treated 16,969 cases by using three types of lithotripter machines. The goal of this retrospective study was to investigate the effectiveness and safety of ESWL therapy for urinary stones.
Materials and methods
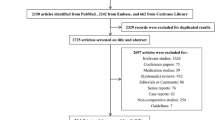
From August 1988 to December 2018, a total of 22,039 patients with urinary stones underwent therapy in our hospital, and 16,667 (76%) were treated with ESWL therapy. Among the patients, there were 124 paediatric patients and 178 special patients. Those special cases included 63 allograft kidneys stone, 48 horseshoe kidneys stone, 41 polycystic kidneys stone and 26 solitary kidneys stone. The average patient age was 41.7 years (range 4–87). To determine and compare the stone clearance rate, all of the patients had single stones in this study.
Over the thirty years, three types of lithotripters were used in our department. From 1988 to 1998, the first-generation electrohydraulic extracorporeal lithotripter (NS-15, Huikang China) was used, and it was replaced by an electromagnetic lithotripter (HK-V, Huikang China) from 1999 to 2010. The HK-V lithotripter was equipped with a high voltage electromagnetic generator, which could discharge 13–16 kV shock wave energy. It was also equipped with a dual-mode imaging system. Since 2010, a new multiple function electromagnetic lithotripter (HK-Vm, Huikang China) has been developed. The newer machine was equipped with a multifunctional operating table, high-resolution X-ray and an ultrasonic stone positioning system. The dual-mode imaging system, combined with the ergonomic design, ensures an accurate stone localization and a smooth operation. The high voltage discharge range of the shock wave generator is 13–20 kV, and the shock wave energy can be steplessly adjusted.
All patients underwent ultrasonography and abdominal plain film X-ray or CT scan examinations before and after the ESWL therapy. Patients with residual stones underwent a second ESWL, with an interval of 1 to 2 weeks. For the adult patients, the shock wave ranged from 1300 to 4000 shocks under a voltage of 13–18 kV, with a frequency ranging from 60 to 120 shocks per minute. However, the shock wave for paediatric patients ranged from 600 to 1500 shocks under a voltage of 9–13 kV, and the frequency ranged from 40 to 60 shocks per minute. The details of the patients as well as the stone location and size are described in Table 1. Ultrasonography or plain X-ray was used to estimate the stone clearance, and a residual stone fragment that is smaller than 2 mm was considered a successful stone clearance. The postoperative complications were determined by the modified Clavien grading system [3, 4]. The grade 1 complications mainly included gross haematuria, fever and low back pain and could resolve without medical care. Perirenal haematoma, infections or blood transfusion were recorded as grade II complications and required hospital care and medical attention. A double J stent insertion or a nephrostomy with local anaesthesia were marked as grade IIIa complications, and surgical interventions such as PCNL or FURL under general anaesthesia were classified as grade IIIb complications. Life-threatening complications requiring ICU treatment were categorized as grade IV complications. Patient death was regarded as a grade V complication.
Statistical analysis
Statistical analysis was performed with SPSS (version 24.0). Continuous variables are reported as the median and interquartile range (IQR); categorical variables are reported as the number of cases (No.) and the percent (%). The Mann–Whitney U test was used to compare the continuous variables. Pearson χ2 correlation was used for evaluating the categorical variables. P < 0.05 was considered significant.
Results
As the recorded data showed, the pSCR of ureteral and renal stones ranged from 32.6% to 66.1% after a single ESWL using the NS-15 lithotripter. After multiple therapies, the fSCR could increase from 41.1% to 83.6% and the lowest SCR was obtained from ESWL when stones were in the lower pole of the kidney. The pSCR was only 32.6%, whereas the fSCR could increase to 41.1%.
The incidence of grade I complications was 33.2%, while that of grade II complications was 5.8%. Seventy-three (1.6%) patients required a double J stent insertion or a nephrostomy under local anaesthesia (grade IIIa). Fifty-nine (1.5%) patients underwent operations under general anaesthesia (grade IIIb). Four patients had serious uroseptic or haemorrhagic shock and required emergency ICU medical care (grade IV). In addition, one patient with a coagulation dysfunction died of serious haemorrhagic shock in 1993 (grade V).
When the electromagnetic HK-V lithotripter was used from 1999 to 2009, the pSCR ranged from 33.5% to 72.4%, depending on the stone locations. The fSCR of distal ureter stones increased to 83.1%, and the fSCR decreased to 44.1% for stones in the lower pole. In the HK-V lithotripter group, the incidence of grade I and II complications was 26.9% and 5.7%, respectively. Grade IIIa complications, including 78 double J stent insertions and 35 percutaneous nephrostomies, were recorded in 113 patients. In total, 79 patients had surgeries, including 51 FURL, 25 PCNL and 3 open surgeries under general anaesthesia. Among them, two patients needed ICU medical care due to uroseptic shock, and one patient underwent a nephrectomy because of a kidney rupture.
In 2010, the new electromagnetic lithotripter HK-Vm was put to use in our hospital. The pSCRs for ureteral and renal stones (45.9–80%) were significantly higher than those in the NS-15 and HK-V groups. Although the fSCR was also improved, the difference was not statistically significant. However, the fSCR of lower calyx stones (55.9%) was obviously higher than that in the NS-15 (41.4%) and HK-V (44.4%) groups.
The incidence of grade I (17.5%) and grade II complications (1.4%) was significantly lower than that of the other lithotripter groups. Grade IIIa complications occurred in 60 patients (1.1%). Forty-one patients were treated with a double-J stent insertion due to stone streets. Thirteen patients underwent PCNL because of serious hydronephrosis, and the remaining six patients underwent a selected renal arteriographic embolism for serious renal haemorrhage. In addition, thirty-four patients (0.6%) needed operations, such as FURS and PCNL under general anaesthesia (grade IIIb). Only one patient with diabetes was admitted to the ICU because of uroseptic shock combined with a renal haematoma. All of the details of stone clearance and complications in the different lithotripter groups are shown in Table 2.
In terms of paediatric patients, the fSCR could reach up to 80% (103/124). Thirteen patients with ESWL failure underwent FURS or PCNL. Most complications were mild, and only two patients needed emergency double J stent insertion under general anaesthesia due to stone streets.
Apart from paediatric patients, ESWL is also effective in treating special cases. For stones in allograft kidneys, the fSCR was 71.4% (44/63). Eleven patients with ESWL failure underwent PCNL, and two underwent an emergency percutaneous nephrostomy due to ureter obstructions. For stones present in polycystic kidneys, the fSCR was 73.2%. Six patients with ESWL failure underwent FURS, and five underwent PCNL. Two patients had perirenal haematomas and were hospitalized. The remaining eight patients with ESWL failure underwent FURS. The fSCR of solitary kidney stones was 69.2%, while that of horseshoe kidney stones was 72.9%. Four patients underwent FURS, and five received PCNL therapy as a result of ESWL failure. Two patients needed emergency double J stent insertion, and one underwent open surgery to alleviate an obstruction. All of the details of the stone clearance and complications in the special stone cases mentioned above are described in Table 3.
Discussion
ESWL has dramatically changed the treatment of urinary stones and has remained the first-line treatment in the past four decades [5, 6]. However, it was difficult to accurately determine the proportion of ESWL in all of the stone treatment methods. The reported proportion ranged from 35% in a German primary urolithiasis centre in 2007 [7] to 70–80% in the United States in 2000 [8]. With the rapid development of endourological technologies in recent years, most urinary stones can be treated safely and effectively with FUR [9] or PCNL [10]. Is ESWL still valid in the endourological era at present?
According to our data, over 70% of the urinary stone patients had undergone ESWL therapy within thirty years. Although the use of ESWL therapies has been declining since 2010, these therapies are still the first-line treatment option for most urinary stone patients. This result was consistent with other related reports [11,12,13]. ESWL was particularly effective in treating ureter stones, such as stones in the distal ureter, with an estimated fSCR of 80–90%. ESWL was less effective in treating lower calyx stones, as the fSCR was only 40–5%. In terms of the paediatric patients, ESWL was also effective, with a fSCR of 81.5%. For stones in allograft kidneys, polycystic kidneys, solitary kidneys and horseshoe kidneys, the fSCR could increase to approximately 70%, which was consistent with the literature [14,15,16,17].
In addition, ESWL is less invasive and is therefore safe. According to the medical data, most complications were mild; the complications did not require any additional medical care; and only a small number of patients with a prerenal haematoma, ureter obstruction or serious infections needed to be hospitalized. A few patients with ESWL failure underwent open surgeries. Thanks to the recent developments in endourological technology, open surgeries have been replaced by minimally invasive operations such as FURS or PCNL. One patient, diagnosed with a coagulation dysfunction when admitted to the hospital, died of severe haemorrhagic shock in 1993. Since then, coagulation profiles have been routinely performed prior to ESWL. No severe complications were recorded for patients who had stones in allograft kidneys, horseshoe kidneys, or polycystic or solitary kidneys.
Apart from the effectiveness and safety, ESWL is more convenient and less expensive than other endourological surgeries [18, 19]. First, it is performed as an outpatient service and is performed anaesthesia free in China, so patients do not need to be hospitalized. In addition, compared with other endourological surgeries, it costs much less, roughly one-twentieth of the other techniques.
Due to the above reasons, ESWL is still the most preferred practice in treating urinary stones in China. Its effectiveness in stone clearance and in reducing the side effects of organ injury is still improving thanks to the improvements in biomedical engineering technology. The new generation lithotripter, combined with fluoroscopy and ultrasound in a modular design with detachable units, provide multiple functions that can be used not only in lithotripsy but also in a broad range of endourological applications [20]. With the recent developments in imaging, lithotripters are equipped with optical or acoustic tracking systems, which are beneficial to targeting stones and reducing radiation exposure [21]. An acoustic feedback system has also been developed to monitor stone disintegration in a timely manner, which can prevent overtreatment [22]. ESWL is getting more accurate and less invasive.
To safely perform ESWL therapy, the following practices should be observed. First, the patients should be carefully selected in strict accordance with the guidelines. ESWL is mainly recommended in the treatment of stones that are less than 2 cm and that are located in the renal pelvis or the upper or middle calyx [23]. The success rate of ESWL in treating complicated stones is very low, and there were recorded failures in cases of partial staghorn stones and when treating large stones that were over 4 cm. Therefore, other endourological surgeries, such as PCNL, should be performed to treat large or complicated stones, while flexible ureteroscopy or mini PCNL is highly recommended for lower calyx stones [24, 25]. ESWL should be avoided in cases of large stones over 1.5 cm or secondary stones caused by an abnormal anatomy. Additionally, the shock wave intensity and treatment intervals should be strictly controlled to minimize complications. Shock waves could induce renal parenchyma vascular damage [26] and can cause renal haematomas and even a kidney rupture [27]. Neither the voltage nor shocks should be increased for high-intensity stones. Urinary stones associated with severe hydronephrosis are likely to cause kidney rupture and require careful treatment. More importantly, prior to ESWL therapy, a percutaneous nephrostomy is recommended.
Conclusion
Through a retrospective review of 16,667 patients who underwent ESWL therapy in our hospital during the 30-year period (1988–2018), we concluded that ESWL was still effective in treating most urinary stones, including paediatric and special cases, such as allograft kidney stones, horseshoe kidney stones, polycystic kidney stones, and solitary kidney stones. ESWL is convenient and inexpensive, and it is still widely performed in China and is becoming increasingly accurate thanks to technological developments. Therefore, we believe there is still a place for ESWL in the present endourological era.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- ESWL:
-
Extracorporeal shockwave lithotripsy
- FUR:
-
Flexible ureteroscopy
- PCNL:
-
Percutaneous nephrostolithotomy
- pSCR:
-
Primary stone clearance rate
- fSCR:
-
Final stone clearance rate
References
Srisubat A, Potisat S, Lojanapiwat B, Setthawong V, Laopaiboon M(2014) Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst Rev. 24:CD007044.
Rassweiler J, Rieker P, Rassweiler-Seyfried MC (2020) Extracorporeal shock-wave lithotripsy: is it still valid in the era of robotic endourology? Can it be more efficient? Curr Opin Urol 30:120–129
Kadlec AO, Greco KA, Fridirici ZC, Hart ST, Vellos TG, Turk TM (2013) Comparison of complication rates for unilateral and bilateral percutaneous nephrolithotomy (PCNL) using a modified Clavien grading system. BJU Int 111:E243-248
Bas O, Bakirtas H, Sener NC, Ozturk U, Tuygun C, Goktug HN, Imamoglu MA (2014) Comparison of shock wave lithotripsy, flexible ureterorenoscopy and percutaneous nephrolithotripsy on moderate size renal pelvis stones. Urolithiasis 42:115–120
Basulto-Martínez M, Klein I, Gutiérrez-Aceves J (2019) The role of extracorporeal shock wave lithotripsy in the future of stone management. Curr Opin Urol 29:96–102
Badawy AA, Saleem MD, Abolyosr A, Aldahshoury M, Elbadry MS, Abdalla MA, Abuzeid AM (2012) Extracorporeal shock wave lithotripsy as first line treatment for urinary tract stones in children: outcome of 500 cases. Int Urol Nephrol 44:661–666
Ather MH, Nazim SM, Sulaiman MN (2009) Efficacy of semirigid ureteroscopy with pneumatic lithotripsy for ureteral stone surface area of greater than 30 mm2. J Endourol 23:619–622
Honeck P, Wendt-Nordahl G, Krombach P, Bach T, Häcker A, Alken P, Michel MS (2009) Does open stone surgery still play a role in the treatment of urolithiasis? Data of a primary urolithiasis center. J Endourol 23:1209–1212
Doizi S, Traxer O (2018) Flexible ureteroscopy: technique, tips and tricks. Urolithiasis 46:47–58
Ghani KR, Andonian S, Bultitude M, Desai M, Giusti G, Okhunov Z, Preminger GM, de la Rosette J (2016) Percutaneous nephrolithotomy: update, trends, and future directions. Eur Urol 70:382–396
Milligan M, Berent AC (2019) Medical and interventional management of upper urinary tract uroliths. Vet Clin North Am Small Anim Pract 49:157–174
McClinton S, Cameron S, Starr K et al (2018) TISU: Extracorporeal shockwave lithotripsy, as first treatment option, compared with direct progression to ureteroscopic treatment, for ureteric stones: study protocol for a randomised controlled trial. Trials 22:286
Seklehner S, Laudano MA, Jamzadeh A, Del Pizzo JJ, Chughtai B, Lee RK (2014) Trends and inequalities in the surgical management of ureteric calculi in the USA. BJU Int 113:476–483
Jeong US, Lee S, Kang J, Han DH, Park KH, Baek M (2013) Factors affecting the outcome of extracorporeal shock wave lithotripsy for unilateral urinary stone in children: a 17-year single-institute experience. Korean J Urol 54:460–466
Semerci B, Verit A, Nazli O, Ilbey O, Ozyurt C, Cikili N (1997) The role of ESWL in the treatment of calculi with anomalous kidneys. Eur Urol 31:302–304
Srivastava A, Bansal R, Srivastava A, Chaturvedi S, Ranjan P, Ansari MS, Yadav A, Kapoor R (2012) Percutaneous nephrolithotomy in polycystic kidney disease: is it safe and effective? Int Urol Nephrol 44:725–730
Vuksanovic A, Micic S, Petronic V, Bojanic N (1997) Solitary kidney stone treatment by extracorporeal shock wave lithotripsy. Eur Urol 31:305–310
Perez-Ardavin J, Lorenzo L, Caballer-Tarazona V et al (2020) Comparative analysis of direct and indirect costs of two minimally invasive techniques for the treatment of renal/ureteral calculi smaller than 2 cm. Actas Urol Esp (Engl Ed) 44:505–511
Constanti M, Calvert RC, Thomas K, Dickinson A, Carlisle S (2020) Cost analysis of ureteroscopy (URS) vs extracorporeal shockwave lithotripsy (ESWL) in the management of ureteric stones <10 mm in adults: a UK perspective. BJU Int 125:457–466
Talso M, Tefik T, Mantica G, Rodriguez Socarras M, Kartalas Goumas I, Somani BK, Esperto F (2019) Extracorporeal shockwave lithotripsy: current knowledge and future perspectives. Minerva Urol Nefrol 71:365–372
Bach C, Karaolides T, Buchholz N (2012) Extracorporeal shock wave lithotripsy: What is new? Arab J Urol 10:289–295
Leighton TG, Fedele F, Coleman AJ, McCarthy C, Ryves S, Hurrell AM, De Stefano A, White PR (2008) A passive acoustic device for real-time monitoring of the efficacy of shockwave lithotripsy treatment. Ultrasound Med Biol 34:1651–1665
Pradère B, Doizi S, Proietti S, Brachlow J, Traxer O (2018) Evaluation of guidelines for surgical management of urolithiasis. J Urol 199:1267–1271
Junbo L, Yugen L, Guo J, Jing H, Ruichao Y, Tao W (2019) Retrograde intrarenal surgery vs. percutaneous nephrolithotomy vs. extracorporeal shock wave lithotripsy for lower pole renal stones 10–20 mm: a meta-analysis and systematic review. Urol J 16:97–106
Zhang H, Hong TY, Li G, Jiang N, Hu C, Cui X, Chu C, Zhao JL (2019) Comparison of the efficacy of ultra-mini PCNL, flexible ureteroscopy, and shock wave lithotripsy on the treatment of 1–2 cm lower pole renal calculi. Urol Int 102:153–159
Li X, Long Q, Cheng X, He D (2014) Shock wave induces biological renal damage by activating excessive inflammatory responses in rat model. Inflammation 37:1317–1325
Jeon BH, Jang JH, Oh JH, Oh SY, Lee SJ, Kim SE, Kim CW, Choe JW, Lee KJ (2009) Kidney rupture after extracorporeal shockwave lithotripsy: report of a case. J Emerg Med 37:13–14
Acknowledgements
The abstract of our data was presented as a poster at the 34th EAU congress in Barcelona, 2019. It was titled “What’s the role of extracorporeal shockwave lithotripsy (ESWL) in the endoscopic era?” -- a retrospective review of ESWL for urinary tract calculi in the past thirty years.” This abstract can be accessed at https://resource-centre.uroweb.org/resource. center/eau19/187016/Abstract.
Author information
Authors and Affiliations
Contributions
XC: supervise the study and interpretation of data. JC: operation and record the data. XZ: operation and record the data. QL: acquisition and analysis. HH: revised the paper. XL: designed the study and drafted the work.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Ethical standards
All authors have seen the manuscript and approved its submission to your journal. The study was approved by our institutional review board and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, X., Chen, J., Zhou, X. et al. Is there a place for extracorporeal shockwave lithotripsy (ESWL) in the endoscopic era?. Urolithiasis 50, 369–374 (2022). https://doi.org/10.1007/s00240-022-01307-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-022-01307-4