Abstract
Background
At present, there is no universally accepted standard of care for osteoradionecrosis (ORN), and comprehensive clinical guidelines remain absent. The primary objective of this study is to offer insights into the effectiveness and safety of microvascular reconstruction approach in patients with ORN.
Methods
A retrospective analysis was conducted on all patients who underwent free flap reconstruction following a diagnosis of ORN by the senior author, from 2005 to 2022. Data regarding the patient’s demographics, comorbidities, previous treatments, ORN classification, postoperative complications, and therapeutic outcome were collected.
Results
Fifty-three free flaps were carried out in a cohort of 48 patients. One maxilla ORN and 42 mandible ORN were treated. The most common flap chosen was free fibula flap. The only risk factor that was statistically significant for major complications was previous neck dissection. Concerning complications after discharge, 41 patients had follow-up with an average follow-up duration of 60 months. Exposure of osteosynthesis material and fistula were the most common long-term complications that required return to the OR. Only 11.36% had recurrence of ORN.
Conclusions
The iliac crest flap represents a valuable option for mandible reconstruction. However, this preference does not extend to ORN; fibula flap remains the optimal choice. It is worth noting that flap and complication rates are notably higher in ORN. Patients with a history of neck dissection are at a heightened risk of complications. Our study demonstrates a reassuring outcome as ORN recurrence occurred approximately in only one out of eight patients.
Level of evidence: Level IV, risk/prognostic.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
While a precise consensus on the definition of osteoradionecrosis (ORN) remains elusive, it is conventionally characterized as a condition in which irradiated bone becomes exposed, and the skin or mucosa fails to heal for a minimum duration of 3 months, in the absence of tumor recurrence or bisphosphonate-related osteonecrosis of the jaws [1,2,3].
The prevalence of jaw ORN exhibits considerable variability, ranging from 0.4 to 56%, with the most reported prevalence falling within the range of 5 to 15% [4]. Nonetheless, the probability of ORN development in patients undergoing radiation therapy for head and neck cancer has markedly decreased in recent years [5].
In its early clinical stages, jaw ORN often presents with subtle or inconspicuous symptoms and is primarily characterized by bone exposure. Pain is a commonly reported symptom, with some patients experiencing severe discomfort, with significant impairing of overall quality of life. Additional associated symptoms include dysesthesia, halitosis, and dysgeusia. In severe cases, patients may develop fistulas, pathological fractures, and an inability to engage in oral feeding [6, 7].
The underlying mechanisms of ORN remain poorly understood. Early hypotheses postulated that ORN originates from radiation-induced endarteritis, resulting in hypoxia, hypocellularity, and hypovascularity, with dental surgical procedures being a potential triggering factor [1]. This hypothesis formed the basis for the adoption of hyperbaric oxygen therapy as a treatment approach for this condition. However, recent evidence has cast doubt on this theory, proposing that ORN may not primarily result from hypoxia but rather from a radiation-induced fibro-atrophic process driven by the activation and dysregulation of fibroblastic activity in response to radiation. This revised pathophysiological understanding has provided a rationale for the use of potent antifibrotic agents, such as pentoxifylline-tocopherol, in preventing the development of ORN [8].
At present, there is no universally accepted standard of care for jaw ORN, and comprehensive clinical guidelines remain absent [9]. Nevertheless, a review of the existing literature supports the notion that conservative approaches are suitable for managing early-stage disease, while surgical intervention is generally reserved for advanced cases [10].
Microvascular free tissue transfer for mandibular ORN reconstruction is increasingly prevalent in clinical practice [11]. As highlighted by Chang et al., successful management of advanced cases hinges on the comprehensive removal of all necrotic tissue, followed by immediate reconstruction. Free flaps offer distinct advantages by facilitating the transfer of vascularized bone as well as non-irradiated soft tissue components, thereby enabling optimal functional reconstruction and achieving favorable cosmetic outcomes [12, 13].
In the present study, the authors aim to evaluate the outcomes of free flap reconstruction in patients with advanced ORN following treatment for head and neck tumors. The analysis encompasses the short and long-term incidence of postoperative complications. The primary objective of this study is to offer insights into the effectiveness and safety of microvascular reconstruction approach in patients with ORN and to formulate a treatment algorithm for advanced mandibular ORN.
Material and methods
A retrospective analysis was conducted on all patients who underwent free flap reconstruction following a diagnosis of ORN by the senior author—Prof. Horácio Costa, from 2005 to 2022, in Centro Hospitalar Vila Nova de Gaia. Patients with concurrent tumor diagnoses and those exclusively treated with pedicled flaps were excluded from this study.
Demographic data, comprising age, gender, and primary tumor information, in addition to comorbidities such as smoking status, alcohol consumption, and underlying medical conditions, were gathered through a retrospective process. Furthermore, comprehensive information pertaining to prior treatments, including tumor therapies and chemotherapy, as well as specific ORN-related specifics including disease severity and previous treatments, was systematically collected.
The study also documented short and long-term postoperative complications, with major complications defined as those necessitating surgical intervention. Complications that occurred during the initial inpatient period were classified as immediate, while those manifesting after hospital discharge were designated as long-term complications.
Disease severity and extent were assessed using Schwartz and Kagan’s classification [14], and mandibular surgical defects were characterized according to the classification proposed by Zenha [15].
All patients had previously undergone tracheostomy during the same surgical procedure. A two-team approach was employed for patient management: one team was responsible for flap raising, while the second team focused on ORN excision, mandibular defect modulation, and preparation of the recipient vessels. In cases requiring immediate ORN resection, the extent of mandibular resection was estimated through preoperative imaging and confirmed through macroscopic assessment, ensuring resection until normal bone bleeding was observed.
The collected data underwent initial analysis using fundamental descriptive statistical methods. Subsequently, further tests were conducted to explore significant associations among the variables in question. Variables of interest, including organizational, demographic, operative, and follow-up factors, were examined for their independence in relation to the occurrence of complications, with the chi-square test employed for statistical analysis. Missing values were excluded for statistical analysis.
Results
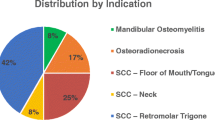
A total of 53 free flap procedures were performed within a cohort consisting of 48 patients, comprising 33 males and 15 females, with an average age of 58 years (ranging from 20 to 82 years). Detailed demographic and clinical information of the patients is presented in Table1.
Among these patients, 7 had previously undergone ORN excision and required mandibular defect reconstruction alone. There was 1 case of maxillary ORN and 42 cases of mandibular ORN treated. Of the 53 flap procedures performed, 1 involved a double flap (2 anterolateral thigh flaps), 1 was a flow-through flap, and in 4 cases, a second free flap was required due to complete necrosis of the initial flap. The most frequently utilized flap was the fibula flap (n = 41), comprising 34 osteoseptocutaneous (OC) fibula free flaps, 5 osteomuscular (OM) fibula flaps, 1 free fibula osteomuscular-pedicled pectoralis major myocutaneous flap, and 1 flow-through flap with OC fibula flaps and a forearm flap. Detailed characteristics of the flaps are presented in Table 2.
The most common mandibular defects were type 1 (n = 12) and type 4 (n = 12). Table 3 provides an overview of the mandibular defects and the corresponding selection of free flaps for their reconstruction.
In one patient, a reconstruction procedure was initially planned to be a sequential link flow-through flap concept, combined with an osteocutaneous (OC) fibula flap. However, during the surgery, the blood supply to the OC fibula flap was insufficient. As a result, the decision was made to remove the fibula flap during the procedure. Consequently, no bone reconstruction was performed in this patient.
In another patient, bilateral ascending ramus (type 3 bilateral) ORN was observed. In this case, only bone resection and a double ALT free flap were performed, with no bone reconstruction.
Figures 1 and 2 depict the surgical reconstructions of class I and class IV mandibular defects utilizing the iliac crest and fibula flaps, respectively.
Of the 53 flap procedures, 35.85% of cases experienced complications that required subsequent surgical interventions. However, it is important to note that the overall flap failure rate remained relatively low at 13.21%. The average follow-up duration was 60 months. Exposure of osteosynthesis material and the occurrence of fistulas emerged as the most prevalent long-term complications necessitating a return to the operating room. Further details regarding these complications are displayed in Table 4.
Previous neck dissection was the only risk factor for the occurrence of major complications, and the use of vein grafts was the only risk factor for flap failure. These findings, delineating the key determinants of surgical success, are meticulously detailed in Table 5.
Comparable outcomes were observed when assessing recipient site complications and donor area complications (Table 6).
Discussion
In recent years, the incidence of ORN as an indication for free flap reconstruction has shown a consistent upward trend [16]. Therefore, it is imperative for plastic surgeons to possess a keen understanding of the distinctive attributes associated with the ORN patient population and to be cognizant of the heightened susceptibility to complications within this cohort [17]. Comprehensive counseling to patients is important, to ensure that they possess a reasonable understanding of the potential risks associated with their treatment choices.
In a systematic review conducted by Lee et al. [18], the overall flap failure rate was determined to be 9.8%, with the highest reported rate reaching up to 20% [19]. In alignment with the prevailing literature, the findings of our study corroborate this trend, with a total flap failure rate of 13.21%. It is worth noting that this failure rate is comparatively higher than studies that include patients reconstructed for different etiologies, which consistently report success rates exceeding 95% [20].
The profound impact of radiotherapy (RT) on wound healing and surgical outcomes is well-established [21]. A comprehensive meta-analysis examining free flap outcomes in irradiated recipient sites, encompassing qualitative and quantitative analysis of 18.776 flaps, revealed a significant association between preoperative RT and an increased risk of both total and partial free flap failure [22]. The deleterious structural changes inflicted on recipient blood vessels by irradiation, such as fibrosis of small vessels, luminal narrowing of larger vessels, endothelial cell dehiscence, and reduced smooth muscle density, increase susceptibility to thrombosis in microvascular surgery [23, 24]. We hypothesize that radiated tissue condition will lead to a higher rate of vascular thrombosis leading to a higher flap failure, and even after the excision of bone necrosis, the persistence of vascular alterations and fibrosis changes can potentially contribute to a higher incidence of late complications. Among the seven patients who had previously undergone excision, receiving only bone-end debridement followed by flap reconstruction did not result in a lower rate of complications. This observation suggests that variances in the timing of ORN resection and subsequent reconstruction do not necessarily yield improved outcomes, as physiological and anatomical alterations may persist.
Among patients discharged after successful free flap procedures, 88.64% achieved a recurrence-free status of ORN during a 5-year follow-up period. This suggests that extended resection followed by reconstruction with non-irradiated tissues may be considered as the primary treatment approach for patients with advanced disease [13, 25].
In the experience of our department, iliac crest flap is the first line treatment for only bone mandibular reconstruction [15, 26] due its natural contour and bone stock [27]. However, in the authors’ experience, in ORN, there often exists a mucous or skin defect or fistula that requires more extensive soft tissue reconstruction. Consequently, the fibula flap is often the preferred choice, primarily due to its reliability as a composite flap. Moreover, the fibula flap facilitates the reconstruction of longer bony segments, with our series exclusively employing it for defects exceeding 12 cm and the longest segment reconstructed measuring 18 cm. Another notable characteristic of the fibula free flap is its extended pedicle. Given that patients who have undergone prior radiotherapy often present with compromised neck vessels, longer pedicles are essential to circumvent the need for vein grafts and mitigate potential complications. In our series, three out of the four cases involving vein grafts resulted in flap loss, underscoring our recommendation to avoid graft usage in ORN patients whenever possible and instead opt for flaps with longer pedicles.
We must highlight that no discernible differences were observed between the fibula flap and the iliac flap regarding recipient and donor area complications. Therefore, the choice between these two types of flaps can be guided by considerations related to flap configuration. In a specific case involving bilateral osteoradionecrosis of the ramus, we elected to resect the ramus and perform only soft tissue reconstruction. This approach aligns with the perspective put forth by Chang et al., suggesting that in patients with limited posterior mandibular ORN, reconstruction with soft tissue flaps may be a viable option [13]. However, when a small segment of the arc of the native mandible remains intact, it is reasonable to employ an osteotomized fibula flap interposed by the small segment, potentially reducing the need for two flaps in a compromised neck (Fig. 3).
Zenha et al. introduced a novel classification system and algorithm for mandibular reconstruction following a thorough retrospective analysis of 218 cases. In their study, a consistent approach to bone defects, both intraoral and extraoral, was applied across all classes of mandibular defects. As previously mentioned, the utilization of free flap reconstruction was specifically reserved for severe cases. Building upon this algorithm and after analyzing the flap choices in our 52 cases of jaw reconstruction, a possible algorithm of ORN management is depicted in Fig. 4.
In our study, patients with a history of previous neck dissection exhibited a heightened risk of major complications and return to operating room, although flap failure rates remained unaffected. A comparative study involving patients reconstructed with free flaps similarly revealed that individuals with a history of prior neck dissection face a greater likelihood of flap re-exploration when compared to those who have solely undergone radiotherapy [26]. Furthermore, the availability of recipient vessels was observed to be more constrained in patients with a history of neck dissection and/or radiation therapy [28]; also, recipient vessel availability was more limited in patients with neck dissection and/or radiation therapy [29]. Nevertheless, it is essential to emphasize that the risk of flap failure was not increased, suggesting that the use of free flaps in previously dissected necks remains a safe option [30]. Reconstructive surgeons must be aware that the risk of returning to the OR is higher and have a close postoperative surveillance.
The limitations inherent in our study include its retrospective design and the ideally larger sample size required to enhance statistical power. Consequently, our study lacks the robustness of larger-scale prospective investigations. To the extent of our knowledge, there is a paucity of prospective studies in the literature on this subject. Conducting prospective studies holds the potential to yield additional insights, enabling us to offer more precise and informed counseling to patients with advanced disease.
Conclusions
The iliac crest flap represents a valuable option for mandible reconstruction and is often the preferred choice for several conditions. However, this preference does not extend to ORN patients, for whom the fibula flap remains the optimal choice due to its reliability as a composite flap. It is worth noting that flap and complication rates are notably higher in ORN patients. Additionally, patients with a history of previous neck dissection are at a heightened risk of complications and should be appropriately informed. Despite the potential for complications, our study demonstrates a reassuring outcome as ORN recurrence occurred approximately in only one out of eight patients.
Data Availability
The data support the findings of this study are available from the corresponding author: Larissa Lanzaro, upon reasonable request.
References
Marx RE (1983) A new concept in the treatment of osteoradionecrosis. J Oral Maxillofac Surg 41(6):351–357
Singh A, Huryn JM, Kronstadt KL, Yom SK, Randazzo JR, Estilo CL (2022) Osteoradionecrosis of the jaw: a mini review. Front Oral Health 3:980786
Harris M (1992) The conservative management of osteoradionecrosis of the mandible with ultrasound therapy. Br J Oral Maxillofac Surg 30(5):313–318
Chronopoulos A, Zarra T, Ehrenfeld M, Otto S (2018) Osteoradionecrosis of the jaws: definition, epidemiology, staging and clinical and radiological findings. A concise review. Int Dental J 68(1):22–30
Nabil S, Samman N (2012) Risk factors for osteoradionecrosis after head and neck radiation: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol 113(1):54–69
Nadella KR, Kodali RM, Guttikonda LK, Jonnalagadda A (2015) Osteoradionecrosis of the jaws: clinico-therapeutic management: a literature review and update. J Maxillofac Oral Surg 14:891–901
Lyons A, Ghazali N (2008) Osteoradionecrosis of the jaws: current understanding of its pathophysiology and treatment. Br J Oral Maxillofac Surg 46(8):653–660
Delanian S, Lefaix J-L (2004) The radiation-induced fibroatrophic process: therapeutic perspective via the antioxidant pathway. Radiother Oncol 73(2):119–131
Raggio BS, Winters R (2018) Modern management of osteoradionecrosis. Curr Opin Otolaryngol Head Neck Surg 26(4):254–259
Jacobson AS, Buchbinder D, Hu K, Urken ML (2010) Paradigm shifts in the management of osteoradionecrosis of the mandible. Oral Oncol 46(11):795–801
Huang N, Wang P, Gong P, Huang B et al (2023) The progress in reconstruction of mandibular defect caused by osteoradionecrosis. J Oncol 2023:1440889
Buchbinder D, Hilaire HS (2006) The use of free tissue transfer in advanced osteoradionecrosis of the mandible. J Oral Maxillofac Surg 64(6):961–964
Chang DW, Oh H-K, Robb GL, Miller MJ (2001) Management of advanced mandibular osteoradionecrosis with free flap reconstruction. Head Neck J Sci Spec Head Neck 23(10):830–835
Schwartz HC, Kagan AR (2002) Osteoradionecrosis of the mandible: scientific basis for clinical staging. Am J Clin Oncol 25(2):168–171
Zenha H, Azevedo M, Vieira R, Costa H (2023) Microsurgical reconstruction of the mandible part ii: new classification system and algorithm. Eur J Plast Surg 46:707–716
Zaghi S, Danesh J, Hendizadeh L, Nabili V, Blackwell KE (2014) Changing indications for maxillomandibular reconstruction with osseous free flaps: a 17-year experience with 620 consecutive cases at ucla and the impact of osteoradionecrosis. Laryngoscope 124(6):1329–1335
Pinto C, Coelho J, Guedes T, Andresen C, Santos D, Martins JM, Gomes N, Zenha H, Costa H (2017) Microsurgical reconstruction in mandible osteoradionecrosis: a clinical experience from portugal. Eur J Plast Surg 40:277–288
Lee M, Chin RY, Eslick GD, Sritharan N, Paramaesvaran S (2015) Outcomes of microvascular free flap reconstruction for mandibular osteoradionecrosis: a systematic review. J Craniomaxillofac Surg 43(10):2026–2033
Curi MM, Santos MO, Feher O, Faria JCM, Rodrigues ML, Kowalski LP (2007) Management of extensive osteoradionecrosis of the mandible with radical resection and immediate microvascular reconstruction. J Oral Maxillofac Surg 65(3):434–438
Sweeny L, Topf M, Wax MK, Rosenthal EL, Greene BJ, Heffelfinger R, Krein H, Luginbuhl A, Petrisor D, Troob SH et al (2020) Shift in the timing of microvascular free tissue transfer failures in head and neck reconstruction. Laryngoscope 130(2):347–353
Nepon H, Safran T, Reece EM, Murphy AM, Vorstenbosch J, Davison PG (2021) Radiation-induced tissue damage: clinical consequences and current treatment options. In: Seminars in Plastic Surgery 35:181–188. Thieme Medical Publishers, Inc. 333 Seventh Avenue, 18th Floor, New York, NY
Tasch C, Pattiss A, Maier S, Lanthaler M, Pierer G (2022) Free flap outcome in irradiated recipient sites: a systematic review and meta-analysis. Plast Reconstr Surg Glob Open 10(3):e4216
Guelinckx PJ, Boeckx WD, Fossion E, Gruwez JA (1984) Scanning electron microscopy of irradiated recipient blood vessels in head and neck free flaps. Plast Reconstr Surg 74(2):217–226
Cooper JS, Fu K, Marks J, Silverman S (1995) Late effects of radiation therapy in the head and neck region. Int J Radiat Oncol Biol Phys 31(5):1141–1164
Madrid C, Abarca M, Bouferrache K (2010) Osteoradionecrosis: an update. Oral Oncol 46(6):471–474
Zenha H, Azevedo MS, Vieira R, Lanzaro L, Costa H (2023) Microsurgical reconstruction of the mandible part i: experience of 218 cases and surgical outcomes. Eur J Plast Surg 46:515–523
Kim RY, Sokoya M, Ducic Y, Williams F (2019) Free-flap reconstruction of the mandible. In: Seminars in Plastic Surgery 33:046–053. Thieme Medical Publishers
Shankhdhar VK, Mantri MR, Wagh S, Thiagarajan S, Chaukar D, Jaiswal D, Mathews S (2022) Microvascular flap reconstruction for head and neck cancers in previously operated and/or radiated neck: is it safe? Ann Plast Surg 88(1):63–67
Hanasono MM, Barnea Y, Skoracki RJ (2009) Microvascular surgery in the previously operated and irradiated neck. Microsurg Off J Int Microsurg Soc Eur Feder Soc Microsurg 29(1):1–7
Tan NC, Lin P-Y, Chiang Y-C, Chew K-Y, Chen C-C, Fujiwara T, Kuo Y-R (2014) Influence of neck dissection and preoperative irradiation on microvascular head and neck reconstruction—analysis of 853 cases. Microsurgery 34(8):602–607
Funding
The authors declare that no funds, grants, or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception, design, material preparation, data collection, and analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Approval was granted by the Ethics Committee of Centro Hospitalar Vila Nova de Gaia/Espinho - CES 39/2022.
Consent to participate
Consent was obtained from all individuals participants who participated in the study.
Competing interests
Larissa Lanzaro, Leonor Caixeiro, Carolina Chaves, Bruno Morgado, Cristina Pinto, Horácio Zenha, and Horácio Costa declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lanzaro, L., Caixeiro, L., Chaves, C. et al. Lessons learned from reconstructing advanced osteoradionecrosis with free vascularized flaps: a retrospective study. Eur J Plast Surg 47, 34 (2024). https://doi.org/10.1007/s00238-024-02170-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00238-024-02170-9