Abstract
Purpose
Non-aneurysmal perimesencephalic subarachnoid hemorrhage (PmSAH) represents 6.8% of spontaneous subarachnoid hemorrhage, and usually has a benign clinical course. However, patients might have early cerebral ischemic lesions and long-term neurocognitive complaints. Cerebral atrophy has been described in patients after aneurysmal SAH, but not in PmSAH. We aimed to investigate if PmSAH associates with increased brain volume loss.
Methods
In this prospective study, we included consecutive patients with PmSAH that performed MR in the first 10 days after hemorrhage, and follow-up MR 6–7 years later. Automated volumetric measurements of intracranial, white matter, gray matter, whole brain, lateral ventricles, hippocampus, and amygdala volumes were performed. Volumes were compared to a normal population, matched for age.
Results
Eight patients with PmSAH were included, with a mean age of 51.5 (SE 3.6) at baseline. The control group included 22 patients with a mean age of 56.3 (SE 2.0). A relative reduction of all volumes was found in both groups; however, PmSAH patients had significant reductions in intracranial, white and gray matter, whole brain, and hippocampal volumes when compared to controls. These changes had a higher magnitude in whole brain volume, with a significant absolute decrease of 6.5% in PmSAH patients (versus 1.9% in controls), and a trend for an increase in lateral ventricle volume (absolute 21.3% increase, versus 3.9% in controls).
Conclusion
Our cohort of PmSAH patients showed significant long-term parenchymal atrophy, and higher global and focal parenchymal volume loss rates when compared to a non-SAH population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Non-aneurysmal perimesencephalic subarachnoid hemorrhage (PmSAH) represents around 6.8% of spontaneous subarachnoid hemorrhages (SAH), with a slight male predominance and although a venous origin of the hemorrhage is suspected, it still has not been proved [1].
The clinical presentation is less severe compared to other forms of SAH [2] and the clinical outcome is favorable [3] with quality-of-life levels comparable to those of the normal population [4]. No differences in mortality were found in comparison to the general population[5].
Nevertheless, patients with acute PmSAH have been shown to have early ischemic lesions [6], and in the long term, cognitive and emotional sequelae have been reported [7, 8] with associated high levels of work absenteeism[9].
Even though focal and global cerebral atrophy has been described after SAH in patients with ruptured aneurysms [10, 11], to the best of our knowledge, there are no reports on brain volumes changes after PmSAH. We hypothesize that PmSAH similarly associates with parenchymal volume loss.
In this study, we aim to investigate if there is an increased global or segmental brain volume loss in PmSAH patients, and compare it to a population without SAH.
Methods
Subjects
All patients with acute spontaneous SAH admitted at our tertiary center between May 2013 and November 2014 were enrolled in a prospective cohort study approved by our institutional review board. Inclusion criteria for the main study were as follows: (1) age > 18 years, (2) acute non-traumatic SAH diagnosed by CT and/or lumbar puncture performed within the first 72 h of SAH onset, and (3) informed consent obtained from patient or legal representative. Patients in a very poor clinical condition (GCS 3), pregnant women, patients with renal insufficiency, and patients with any contraindication to perform MR or whose time of onset of SAH was unknown were excluded.
PmSAH was defined as SAH limited to the cisterns around the midbrain, or not extending beyond the proximal Sylvian or interhemispheric fissures, with no parenchymal extension, and with no aneurysm documented on a complete four-vessel and cervical digital subtraction angiography. All patients had a follow-up DSA after at least 7 days. The PmSAH cohort was studied in other publications (Fragata et al.), namely for the presence of ischemic lesions, using MRI-DWI, and for perfusion changes using CT, which differ from this work that besides being a longitudinal study uses volumetric analysis to document brain volume loss.
A control group (n = 22) composed of patients matched for age was selected from patients that performed MR for follow-up of intracranial meningiomas in the same period.
MR imaging
Patients presenting with PmSAH had an MR study between admission up to 72 h after SAH and 8–10 days after SAH on a 1.5-T scanner (Magnetom Avanto, Siemens Healthcare). The imaging protocol consisted of: T1 Sagittal MPRAGE 3D, axial DP/T2 TSE, T2*, and T2 FLAIR, as well as diffusion tensor imaging sequences. After a 6 to 7 years interval after the presenting hemorrhage, a follow-up MR was performed on the same scanner and using the same protocol. In the PmSAH group, 4 patients were lost to follow-up.
Patients in the control group had MR studies within a similar time interval performed on the same scanner, using a protocol that included T1 MPRAGE 3D images.
Volumetric analysis
To extract and measure brain tissue volumes we used volBrain (http://volbrain.upv.es/) [12], a completely automated segmentation tool. With the volBrain system, we obtained and analyzed the following volumes:
-
Intracranial cavity (ICC was defined as the sum of all WM, GM, and cerebrum-spinal fluid (CSF))
-
Tissue volumes: WM, GM volumes
-
Lateral ventricles, hippocampus, amygdala
All these segmentations, with the exception of tissue volumes, are based on different adaptations of multi-atlas patch-based label fusion segmentation [13].
We then calculated the percentage of volume change between baseline and follow-up MR using the formula: (vol2-vol1/vol1) × 100. We also calculated the annual difference, by dividing the total percentage of volume change by the follow-up interval in years.
Statistical analysis
We used SPSS software (V.23.0; IBM, Armonk, NY, USA) for data analysis. Variables were tested for normality. Parametric and nonparametric tests were used accordingly to compare global and segmental volumes between the baseline MR and the follow-up MR, and for comparison of volumes and differences in global and segmental volumes between the patient and control groups. The significant level of p value was set at 0.05.
Results
A total of 8 patients with PmSAH and a total of 22 controls were included. Demographic data are shown in Table 1.
Mean age for the PmSAH group at baseline was 51.5 (SE 3.6), and 38% were females. The control group had a mean age of 56.3 (SE 2.0) at baseline, and 86% were females. None of the patients with PmSAH had acute ischemic lesions on DWI, vasospasm during hospital admission or delayed cerebral ischemia. All PmSAH patients had a GCS of 15 at admission, except for one patient (with a score of 13). This patient also had the highest Fisher score (3), compared to the remaining patients: 4 patients had a modified Fisher score of 1 and 3 patients had a score of 2. Patients with PmSAH had a follow-up MR at 6.8 ± 0.4 years, and patients in the control group had a follow-up MR at 5.0 ± 1.5 years.
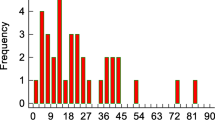
Segmental and global volumes had a trend for higher values in the PmSAH group, except for the volume of the lateral ventricles (see Fig. 1 and Supplementary Table I), possibly reflecting the slightly younger mean age in this group.
A summary of the results of segmental and global volumes for patient and control groups is shown in Table 2. We observed a relative reduction in all parenchymal volumes with time, both in the control group and in the patients with PmSAH. However, PmSAH patients showed significant reductions in intracranial volume, white matter and gray matter volume, whole brain volume, and hippocampal volume when compared to controls. These changes had a higher magnitude in whole brain volumes, where PmSAH patients showed a significant absolute decrease in volume of 6.5% (versus 1.9% in controls) (Table 3). We tried to understand if there was an increased annual rate of volume loss in the PmSAH group, translating an accelerated parenchymal atrophy. When we analyzed the annual rate of volume loss, again we found an increased annual loss of whole brain volume in patients with PmSAH compared to controls (− 0.91% in PmSAH patients versus − 0.34% in controls). Patients with PmSAH also showed a trend for larger increase in lateral ventricle volume (absolute 21.3% increase in volume, compared to 3.9% in controls), almost reaching significance (p = 0.055), possibly reflecting a higher degree of subcortical atrophy in these patients.
Discussion
In this study, we aimed to investigate if patients with PmSAH had increased brain volume loss, when compared to a non-SAH population. Our results reveal a globally increased parenchymal atrophy in the PmSAH group, when compared to the control group.
These findings suggest that there might be increased brain atrophy in PmSAH, which globally affects the brain, but is also selective for the hippocampi. If we consider that the control group has a higher mean age, which would predictably imply higher brain volume loss rates with time, our findings have even more impact. The annual rate of volume loss seems to be higher only for whole brain volume in patients with PmSAH when compared to controls, suggesting that the parenchymal insult possibly occurs focally at the time of hemorrhage.
The association between increased brain atrophy and PmSAH might help explain the cognitive and emotional sequelae described in these patients [7, 8]. A similar impact of aneurysmal subarachnoid hemorrhage in brain volumes has been described, affecting not only the white and gray matter, but also specifically the hippocampus/temporo-mesial region [10, 11, 14, 15]. This might indicate that the hemorrhage, despite the mechanism in its origin, is in itself a sufficient insult to potentially harm the brain, and lead to parenchymal volume loss. In fact, there is evidence in the literature for a direct apoptotic effect of acute subarachnoid hemorrhage, a mechanism that contributes to early brain injury [16, 17]. Also, early acute ischemic lesions are present both in PmSAH [6] and aneurysmal SAH patients [18], representing an acute insult after hemorrhage. Most studies on early brain injury have focused on aneurysmal hemorrhage; however, we might speculate that there is some form of acute parenchymal injury that also affects PmSAH patients, possibly to a smaller extent.
Our study has some limitations; the most important of all is the small sample size, considering the heterogeneity of the physiological brain atrophy. Neuropsychological evaluation was not performed, to investigate if the more significant atrophy we found in these patients would correlate to cognitive changes.
Volumetric measurements were automatic, therefore not operator dependent, using a reproducible and accurate software [12]. The control population was not matched for sex, since we included patients with intracranial meningiomas, more frequent in the female population. However, one would not expect this to influence the results, since the sex-specific changes in brain size with aging are reported mainly for cerebrospinal fluid volume, but not for parenchymal structures [19].
In conclusion, we report increased parenchymal atrophy in patients with PmSAH in our cohort, mainly reflected in whole brain volume, when compared to a control population. Further investigation in larger cohorts is needed to confirm our findings and better understand the pathophysiological mechanisms behind these findings, and their relation to the neurocognitive changes that occur after PmSAH.
Abbreviations
- PmSAH:
-
Non-aneurysmal perimesencephalic subarachnoid hemorrhage
- SAH:
-
Subarachnoid hemorrhage
- ICC:
-
Intracranial cavity
- WM:
-
White matter
- GM:
-
Gray matter
- CSF:
-
Cerebrospinal fluid
- GCS:
-
Glasgow coma score
References
Mensing LA, Vergouwen MDI, Laban KG et al (2018) Perimesencephalic hemorrhage: a review of epidemiology, risk factors, presumed cause, clinical course, and outcome. Stroke 49:1363–1370. https://doi.org/10.1161/STROKEAHA.117.019843
Beseoglu K, Pannes S, Steiger HJ, Hänggi D (2010) Long-term outcome and quality of life after nonaneurysmal subarachnoid hemorrhage. Acta Neurochir (Wien) 152:409–416. https://doi.org/10.1007/s00701-009-0518-8
Konczalla J, Platz J, Schuss P et al (2014) Non-aneurysmal non-traumatic subarachnoid hemorrhage: patient characteristics, clinical outcome and prognostic factors based on a single-center experience in 125 patients. BMC Neurol. https://doi.org/10.1186/1471-2377-14-140
Konczalla J, Schmitz J, Kashefiolasl S et al (2015) Non-aneurysmal subarachnoid hemorrhage in 173 patients: a prospective study of long-term outcome. Eur J Neurol 22:1329–1336. https://doi.org/10.1111/ene.12762
Greebe P, Rinkel GJE (2007) Life expectancy after perimesencephalic subarachnoid hemorrhage. Stroke 38:1222–1224. https://doi.org/10.1161/01.STR.0000260093.49693.7a
Fragata I, Canto-Moreira N, Canhão P (2019) Ischemic lesions in acute and subacute perimesencephalic subarachnoid hemorrhage. Am J Roentgenol 212:418–424. https://doi.org/10.2214/AJR.18.19700
Boerboom W, Heijenbrok-Kal MH, Khajeh L et al (2014) Differences in cognitive and emotional outcomes between patients with perimesencephalic and aneurysmal subarachnoid haemorrhage. J Rehabil Med 46:28–32. https://doi.org/10.2340/16501977-1236
Madureira S, Canhão P, Guerreiro M, Ferro JM (2000) Cognitive and emotional consequences of perimesencephalic subarachnoid hemorrhage. J Neurol 247:862–867. https://doi.org/10.1007/s004150070074
Marquardt G, Niebauer T, Schick U, Lorenz R (2000) Long term follow up after perimesencephalic subarachnoid haemorrhage [16] (multiple letters). J Neurol Neurosurg Psychiatry 69:127–130. https://doi.org/10.1136/jnnp.70.3.419
Bendel P, Koivisto T, Aikia M et al (2010) Atrophic enlargement of CSF volume after subarachnoid hemorrhage: correlation with neuropsychological outcome. Am J Neuroradiol 31:370–376. https://doi.org/10.3174/ajnr.A1804
Bendel P, Koivisto T, Hanninen T et al (2006) Subarachnoid hemorrhage is followed by temporomesial volume loss: MRI volumetric study [3]. Neurology 67:575–582. https://doi.org/10.1212/01.wnl.0000262956.27015.9d
Manjón JV, Coupé P (2016) Volbrain: an online MRI brain volumetry system. Front Neuroinform 10:1–14. https://doi.org/10.3389/fninf.2016.00030
Coupé P, Manjón JV, Fonov V et al (2011) Patch-based segmentation using expert priors: application to hippocampus and ventricle segmentation. Neuroimage 54:940–954. https://doi.org/10.1016/j.neuroimage.2010.09.018
Lee GY, Ryu CW, Ko HC, Jahng GH (2020) Correlation between gray matter volume loss followed by aneurysmal subarachnoid hemorrhage and subarachnoid hemorrhage volume. Neuroradiology 62:1401–1409. https://doi.org/10.1007/s00234-020-02445-5
Hedderich DM, Reess TJ, Thaler M et al (2019) Hippocampus subfield volumetry after microsurgical or endovascular treatment of intracranial aneurysms-an explorative study. Eur Radiol Exp 3:13. https://doi.org/10.1186/s41747-019-0092-7
Hasegawa Y, Suzuki H, Sozen T et al (2011) Apoptotic mechanisms for neuronal cells in early brain injury after subarachnoid hemorrhage. Acta Neurochir Suppl 110:43–48. https://doi.org/10.1007/978-3-7091-0353-1
Cahill WJ, Calvert JH, Zhang JH (2006) Mechanisms of early brain injury after subarachnoid hemorrhage. J Cereb Blood Flow Metab 26:1341–1353. https://doi.org/10.1038/sj.jcbfm.9600283
Frontera JA, Ahmed W, Zach V et al (2015) Acute ischaemia after subarachnoid haemorrhage, relationship with early brain injury and impact on outcome: a prospective quantitative MRI study. J Neurol Neurosurg Psychiatry 86:71–78. https://doi.org/10.1136/jnnp-2013-307313
Edward Coffey C, F. Lucke J, A. Saxton J, et al (1998) Sex differences in metabolic brain aging. Arch Neurol 55:169–179. https://doi.org/10.1073/pnas.1904673116
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gama Lobo, G., Fragata, I. Long-term global and focal cerebral atrophy in perimesencephalic subarachnoid hemorrhage—a case–control study. Neuroradiology 64, 669–674 (2022). https://doi.org/10.1007/s00234-021-02804-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-021-02804-w