Abstract
Spontaneous subarachnoid hemorrhage (SAH) is a medical emergency characterized by hemorrhage in the subarachnoid space surrounding the brain. In the vast majority of cases (85 %), spontaneous SAH is caused by the rupture of a cerebral aneurysm (aSAH) [1]. The other 15 % are idiopathic and two-thirds of these have a characteristic appearance on computed tomography (CT) and are called benign perimesencephalic SAH (pSAH). The characteristic sign of aSAH is a sudden onset of severe “thunderclap” headache, but patients may also present with vomiting, nausea, photophobia, and nuchal rigidity [2]. A cranial CT scan demonstrates accumulation of blood in the basal cisterns (see Fig. 10.1); patients may also present with hemorrhage into the brain and ventricular system [2]. Hypertension and cigarette smoking are risk factors for aSAH [3]. Although uncommon—the incidence of aSAH in North America is approximately 8–11 per 100,000 persons per year [4, 5]—aSAH carries a poor prognosis, with only 35 % of patients surviving [6, 7]. Indeed, although aSAH accounts for only 7 % of all strokes [8], it is responsible for 27 % of all stroke-related years of life lost before age 65 [9]. The high mortality after aSAH may be partially attributed to misdiagnosis. Up to 50 % of cases are misdiagnosed as migraine or tension-type headache due to failure to obtain lumbar puncture or proper neuroimaging [2]. Despite these statistics, advances in the acute management of aSAH over the past 3 decades—mainly increased use of vascular imaging, reduced delays to treatment, and better acute care management [7]—have substantially reduced mortality after aSAH. In a meta-analysis, Lovelock et al. [7] observed that, while the incidence of aSAH has remained stable over the past 30 years, mortality has been reduced by half and the 30-day case fatality rate has decreased by 0.9 % per annum (Figs. 10.1 and 10.2).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Spontaneous subarachnoid hemorrhage (SAH) is a medical emergency characterized by hemorrhage in the subarachnoid space surrounding the brain. In the vast majority of cases (85 %), spontaneous SAH is caused by the rupture of a cerebral aneurysm (aSAH) [1]. The other 15 % are idiopathic and two-thirds of these have a characteristic appearance on computed tomography (CT) and are called benign perimesencephalic SAH (pSAH). The characteristic sign of aSAH is a sudden onset of severe “thunderclap” headache, but patients may also present with vomiting, nausea, photophobia, and nuchal rigidity [2]. A cranial CT scan demonstrates accumulation of blood in the basal cisterns (see Fig. 10.1); patients may also present with hemorrhage into the brain and ventricular system [2]. Hypertension and cigarette smoking are risk factors for aSAH [3]. Although uncommon—the incidence of aSAH in North America is approximately 8–11 per 100,000 persons per year [4, 5]—aSAH carries a poor prognosis, with only 35 % of patients surviving [6, 7]. Indeed, although aSAH accounts for only 7 % of all strokes [8], it is responsible for 27 % of all stroke-related years of life lost before age 65 [9]. The high mortality after aSAH may be partially attributed to misdiagnosis. Up to 50 % of cases are misdiagnosed as migraine or tension-type headache due to failure to obtain lumbar puncture or proper neuroimaging [2]. Despite these statistics, advances in the acute management of aSAH over the past 3 decades—namely increased use of vascular imaging and reduced delays to treatment [7]—have substantially reduced mortality after aSAH. In a meta-analysis, Lovelock et al. [7] observed that while the incidence of aSAH has remained stable over the past 30 years, mortality has been reduced by half and the 30-day case fatality rate has decreased by 0.9 % per annum (Fig. 10.2).
(a) aSAH secondary to anterior communicating artery aneurysm rupture. Note the characteristic accumulation of blood in the basal cisterns. (b) CT angiography illustrates the anterior communicating artery aneurysm (arrow) in the patient in (a). Figure adapted with permission from Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354:387–396
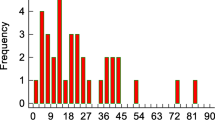
Thirty-day case fatality rate over time. The 30-day case fatality rate after aSAH has decreased by 0.9 % per annum due to increased use of vascular imaging and reduced delays to treatment. Adapted with permission from Lovelock CE, Rinkel GJE, Rothwell PM. Time trends in outcome of subarachnoid hemorrhage. Population-based study and systematic review. Neurology. 2010;74:1494–1501
Although mortality after aSAH has declined over the past few decades, the extent to which patients’ cognitive and functional outcomes have improved over the same time period remains unknown. A large proportion of aSAH patients—up to 76 % [10]—experience persistent cognitive deficits many years after aSAH. These cognitive deficits may lead to difficulties in aspects of functional independence such as return to work, managing finances, and housekeeping. Aneurysmal SAH-associated deficits in cognition and day-to-day functioning are particularly debilitating given that most patients are relatively young (mean age of 55 years [11]), are in their most productive years, and have major responsibilities with respect to work and family. This chapter describes the cognitive and functional deficits after aSAH and examines how clinical and neuroimaging factors influence cognitive and functional outcome.
Cognitive Outcome
Cognitive impairment is most frequent and severe within the first 3 months following aSAH [12], but residual cognitive dysfunction may persist for a lifetime [13]. The following section reviews the cognitive domains most commonly affected after aSAH: attention, memory, executive function, language, and visuospatial function.
Attention
Attention refers to the ability to allocate cognitive resources to a specific task, thereby producing focused behavior. Attention has many components, including selective attention (i.e., paying attention to a specific task), sustained attention (i.e., paying attention for a prolonged time period), and divided attention (i.e., paying attention to multiple tasks simultaneously). Several studies have found that among all cognitive domains, attentional deficits are the most frequent self-reported complaints by both aSAH patients and their relatives, with estimates as high as 70 % [14–20]. As a result of these attentional problems, patients often report difficulties with maintaining conversations, reading, watching television, and other tasks that involve cognitive processing [21].
The reported frequency and severity of attentional deficits after aSAH has been variable, however. A study by Ravnik et al. [22] found no correlation between subjective attentional impairment and performance on tests of attention; in fact, patients performed better on tests of attention than on tests of other cognitive domains. Other studies report the prevalence of attentional impairment, as measured by cognitive tests, to be modest, ranging from 3 to 19 % [23–28]. In one study, even patients with severe aSAH (i.e., grade 5 Hunt and Hess [29]) showed mild attentional deficits post-aSAH [30]. Hütter et al. [27] found that 70 % of aSAH survivors reported attention problems, but only 13 % were impaired on neuropsychological tests of attention. Discordance between self-reported cognitive deficits and results from objective cognitive tests may be attributed to patients misinterpreting their cognitive deficits as impairments of attention. Additionally, the high self-reported prevalence of attentional dysfunction may result from confounding factors such as depression [17] or excessive fatigue, the latter of which affects up to 75 % of aSAH survivors [14, 25, 31, 32].
Other studies have found that attentional deficits are common and widespread after aSAH, affecting upwards of 76 % of aSAH survivors [26, 33]. The extent of attentional impairment may depend on the timing of testing, with impairment more likely sooner after the hemorrhage, and on the specific type of attention being tested. Benke et al. [13] observed that while divided attention showed impairment after aSAH, sustained and short-term attention did not.
Several clinical variables affect the degree of attentional impairment post-aSAH. Greater aSAH severity, as measured by Hunt and Hess grade [29], the presence of blood in the Sylvian fissure, greater thickness of subarachnoid blood, as measured by Fisher grade [34], older age, intraventricular hemorrhage, hydrocephalus, and temporary clipping have been associated with poorer attentional function [16, 35–38]. Whether attentional function improves over time is controversial; some investigators claim no improvement over the 12-month period after aSAH [12, 33] while others show improvement over the same time period [39, 40].
Several investigators have correlated attentional function with neuroimaging. Mustonen et al. [41] found that cerebral perfusion heterogeneity, as measured by single photon emission tomography (SPET), at 1-week post-aSAH correlated with performance on attention tests at 1-year post-aSAH. Bendel et al. [42] found that hippocampal volumes after aSAH predicted performance on tests of attention 1-year post-aSAH.
Memory
In the aSAH outcome literature, memory is commonly stratified into different components, including visual memory, verbal memory, short-term memory, and long-term memory. Up to 57 % of survivors self-report memory problems after aSAH [14, 15, 19, 20, 43, 44]. Inability to remember new information and maintain short-term (working) memory are particularly common complaints [17, 44]. Verbal memory is commonly impaired in aSAH patients, the prevalence ranging from 14 to 68 % [12, 18, 20, 31, 45–49]. Likewise, deficits in visual memory are also frequent, with impairment prevalence ranging from 14 to 75 % [18, 20, 31, 33, 45–49].
Unlike attention, in which patients tend to overestimate the degree of subjective attentional dysfunction relative to neuropsychological tests, self-reported memory complaints often underestimate the degree of memory dysfunction as detected by neuropsychological impairment. Ljunggren et al. [18] found that 83 % of aSAH survivors had memory deficits on neuropsychological assessment, but only 58 % self-reported memory deficits on interview. Older age, fewer years of education, poorer neurological grade on admission (as measured by World Federations of Neurological Surgeons Grade [50]), hydrocephalus, ischemia, postoperative vasospasm, ruptured aneurysms in the anterior circulation, and thick subarachnoid blood in the anterior interhemispheric fissure and Sylvian fissures have been associated with poorer performance on tests of verbal and visual memory [33, 35, 51, 52]. Temporary clipping and partial resection of the gyrus rectus, meanwhile, have been associated with poorer short-term memory [27]. Some investigators have demonstrated a relationship between memory deficits and cerebral edema [35], but others have observed no correlation [53].
The wide range in the prevalence of memory impairment can be explained by the use of different standardized tests. Commonly used memory tests include the California Verbal Learning Test [54], the Visual Reproduction subtest of the Wechsler Memory Scale [55], and the Rey-Osterrieth Complex Figure—Recall subtest [56, 57]. Differences in difficulty and sensitivity to impairment between different memory tests may contribute to the variable rates of memory impairment. For instance, Mayer et al. [45] found that 31 % of aSAH survivors showed impaired visual memory on the Rey-Osterrieth Complex Figure—Recall subtest, whereas only 22 % showed impaired visual memory on the Visual Reproduction subtest. These findings suggest that the frequency of cognitive impairment after aSAH is determined in part by the particular test used to measure cognitive performance.
Time of testing in relation to the initial insult is also critical in determining aSAH-associated memory deficits. Powell et al. [12, 31] assessed verbal memory at 3, 9, and 18 months post-aSAH. Delayed verbal memory significantly improved from 3 to 9 months and from 9 to 18 months post-ictus, while immediate verbal memory showed no significant improvement in the same time period. Despite improvement in delayed verbal memory over 18 months, 14 % of aSAH patients still had significant delayed verbal memory impairments at 18-month follow-up. Although not all studies differentiate between immediate and delayed verbal memory, the finding that verbal memory improves over time has been replicated by others [39, 53, 58]. Visual memory may also improve over time [33, 39, 53], but results have been inconsistent [58]. Why verbal and visual memory improve over time remains unknown, although reduction of aSAH-associated intracranial pressure [59] and chronic inflammation may play a role [60]. Together, these results show that the prevalence of aSAH-associated memory impairment depends on the type of memory in question and on the length of the follow-up interval.
Although aSAH survivors often report a reduced capacity to learn new information [17], data by D’Esposito et al. [61] suggest that memory impairments are also characterized by an inability to recall information learned prior to aSAH. This form of retrograde amnesia, however, was only observed among patients with medial frontal lobe damage, mainly in arterial territories distal to the anterior communicating artery (ACoA). Given the role of the medial frontal lobe in initiation [62, 63], the inability to recall old information may be due to an inability to initiate memory retrieval. Indeed, Richardson [64] found that, on tests of object naming, aSAH patients had slower retrieval speeds compared to control participants.
The medial temporal lobes, a network of structures that includes the hippocampus together with the entorhinal, perirhinal, and parahippocampal cortices, are critically involved in memory function [65]. A correlation between left hemisphere infarctions and verbal memory impairment in patients with aSAH has been demonstrated [35, 66], but little is known about the specific brain regions in the left hemisphere responsible for verbal memory impairment in aSAH patients. Bendel et al. [42] performed magnetic resonance imaging (MRI) on aSAH survivors and found significantly reduced bilateral hippocampal volumes among aSAH patients relative to healthy controls at 1-year follow-up. Hippocampal volumes correlated with performance on one test of visual memory (the Visual Reproduction subtest of the Wechsler Memory Scale), but not with another visual memory test (the Rey-Osterrieth Complex Figure) or with tests of verbal memory. The investigators did not correlate memory impairment with changes in other brain regions, such as the frontal lobes. This may be important given the role of the frontal lobes in memory function [67] and given that frontal lobe injury is a common sequelae of aSAH [68]. Reduced frontal lobe integrity could account for the unexpected findings reported by Bendel et al. [42]. Indeed, Vilkki et al. [69] found that medial frontal lobe lesions on CT predicted poorer verbal memory in aSAH survivors.
Executive Function
Executive function is predominantly mediated by the frontal lobes [70] and encompasses higher-level cognitive abilities like planning, inhibition, problem-solving, and decision-making. Rather than fractionating executive function into its components, the majority of studies treat executive function as a unitary construct. Consequently, estimates of the frequency of executive dysfunction in aSAH survivors varies widely, ranging from 3 to 76 % [10, 12, 24, 31, 45–48, 71, 72]. Results from studies using neuropsychological assessments complement patients’ self-reported complaints; upwards of 30 % of aSAH survivors self-report a lack of initiative and a reduced capacity for planning and organizing [17, 18]. Executive dysfunction after aSAH is more pronounced in older patients, those with fewer years of education, and those with poorer neurological grade on admission [35, 36]. Similar to memory, a correlation between executive dysfunction and cerebral edema has been documented by some investigators [36], but not by others [53]. Surgical variables also affect outcome; Akyuz et al. [73] found that temporary vessel occlusion exceeding 9 min was a significant predictor of permanent long-term executive deficits.
Kreiter et al. [35] found that executive dysfunction was more severe among patients with ruptured anterior aneurysms than among those with posterior aneurysms. Findings from most other studies, however, suggest no relationship between ruptured aneurysm location and the profile of cognitive impairment [46, 53, 66, 74–76]. Interestingly, Manning et al. [77] found that aSAH patients who had ruptured ACoA aneurysms performed significantly better than patients with aneurysms at other locations on the Tower of London task [78], a test of executive function. Similarly, Papagno et al. [79] observed that patients with ACoA aneurysms performed better than those with aneurysms at other locations on tests of switching and inhibition. The relationship between aneurysm location and profile of cognitive impairment thus remains unclear.
In addition to sometimes causing focal lesions in proximity to the ruptured aneurysm, aSAH often leads to diffuse, global damage to brain tissue in poor-grade patients [10, 80–82]. Global injury is mediated, in part, by elevated intracranial pressure [80], reduction of cerebral blood flow and brain oxygenation, blood–brain barrier breakdown, and global cerebral edema (together these factors contribute to early brain injury; see [83]). Findings from an MRI study by Bendel et al. [84] support the “diffuse damage” hypothesis. The authors found that at 1-year follow-up, aSAH patients showed significantly reduced total grey matter and white matter volumes relative to control subjects. Furthermore, the extent of grey matter volume loss was associated with poorer cognitive test performance, including poorer performance on tests of executive function.
Not all neuroimaging studies, however, support the “diffuse damage” hypothesis. Several MRI studies suggest that executive dysfunction results from focal lesions rather than diffuse damage. Bendel et al. [85] found that 91 % of aSAH patients with executive dysfunction had frontal lobe lesions. Similarly, Martinaud et al. [47] showed that executive dysfunction in aSAH patients was exclusively correlated with lesions to the left frontal lobe, including the left superior frontal gyrus, the left middle frontal gyrus, and the left anterior centrum semiovale. Deficits in behavioral aspects of executive function (e.g., reduction of daily activities, irritability, hyperactivity), meanwhile, were correlated with lesions to the left ventral striatum. An exception to these findings is a study by Vilkki et al. [69] who showed that patients with infarction in the medial frontal lobe had impaired memory, but intact executive function. The relationship between executive dysfunction and frontal lobe injury may thus be qualified by the specific location of the lesion.
Although executive function and memory are often considered distinct cognitive domains, several studies indicate that these domains may interact. As mentioned earlier, D’Esposito et al. [61] observed that patients with medial frontal lobe injury showed deficits in retrieving previously learned information on a memory test. How can injury to the frontal lobes—a region implicated in executive function—affect performance on a memory test? Posterior-inferior midline frontal lesions may damage the septum, which has connection to the hippocampus and plays a role in working memory. Haug et al. [86] suggest that medial frontal lobe injury, which commonly occurs in patients with ACoA aneurysms [47, 85], may lead to deficits in initiation. Indeed, the investigators found that, compared to patients with aneurysms in other locations, these patients tended to perform poorer on the initial portions of memory tests. They also tended to commit more false-positive errors on memory tests, which may arise due to confabulation as opposed to genuine memory impairment. Deficits in executive function may thus “spill over” to affect performance on tests of other cognitive domains, thereby giving a distorted picture of a patient’s cognitive functioning.
The use of different neuropsychological tests, each of which probes a different executive function, may partially explain the high variability in executive dysfunction after aSAH. Proust et al. [48] reported that among aSAH survivors treated with endovascular coiling, 29 % showed impairment on the Wisconsin Card Sorting Task (a measure of cognitive flexibility [87]), while only 7 % showed impairment on the Stroop task (a measure of inhibition [88]). Different aspects of executive function may thus have different rates of impairment. In support of this hypothesis, deficits in cognitive flexibility, as measured by the Wisconsin Card Sorting Task, are found in 8–44 % of aSAH patients [24, 45–48, 71], whereas deficits in inhibition, as measured by the Stroop task, are found in 17–56 % of aSAH patients [46–48].
A study by Manning et al. [77] illustrates the importance of differentiating between different aspects of “frontal lobe” function. Manning et al. [77] evaluated executive function 26 weeks post-aSAH in patients who had made a “good recovery” according to the Glasgow Outcome Scale (GOS) [89]. Aneurysmal SAH survivors performed significantly worse than healthy controls on the Wisconsin Card Sorting, Tower of London, and Stroop tasks, while performance on the Cognitive Estimates [90] task was within normal limits. Each of the tests used by Manning et al. [77] captures a slightly different executive “frontal lobe” function: the Tower of London task assesses planning and problem-solving, the Stroop task assesses ability to inhibit impulsive responding, while the Cognitive Estimates task measures ability to make judgments and estimations. These results indicate that some executive functions are impaired in aSAH survivors (e.g., cognitive flexibility, planning, problem-solving, inhibition), while others are intact (e.g., judgment, estimation). Furthermore, the data suggest that patients classified as having made a good recovery on the GOS may still experience profound cognitive deficits more than 6 months after aSAH. This is consistent with earlier studies showing that up to one-third of aSAH survivors who have made a good recovery on the GOS experience persistent neuropsychological impairment [91].
Different aspects of executive function may have different rates of recovery. Haug et al. [53] found that while inhibition improved within 1 year after aSAH, cognitive flexibility and attention did not. Results from longitudinal studies, however, must be interpreted with caution, as tests of executive function may be subject to practice effects (e.g., Stroop test [92], Trail Making Test [92], Wisconsin Card Sorting Test [93]). Studies that found improvement in response inhibition and cognitive flexibility over time [39, 58] used the Stroop test and Trail Making Test, both of which may have practice effects [92]. These findings further illustrate the importance of distinguishing between different executive functions.
Language
Language function involves comprehension and expression of meaningful written and oral information. The frequency of language impairment among aSAH survivors is highly variable, ranging from 0 to 76 % [10, 12, 24, 31, 45–48, 71]. Few studies have examined patients’ self-reported language complaints; Passier et al. [17] observed that only 8 % of aSAH survivors self-reported deficits in speaking or writing. Interestingly, language function appears to be critical for predicting patients’ perceptions of recovery. Chahal et al. [94] found that 52 % of patients felt they had made a complete recovery from the effects of aSAH 5 years post-ictus. Patients who reported making a full recovery, however, tended to perform better on tests of language and verbal functioning than patients who reported not making a full recovery, suggesting that linguistic function is key for patients’ perception of recovery. Older age, fewer years of education, aneurysms in the anterior circulation, and left hemisphere infarction are significant predictors of poorer language function after aSAH [35, 69].
Language function improves significantly within the first 3 months after aSAH [58] and continues to improve in the 18 months after hemorrhage [12, 31, 58]. Longitudinal studies have typically used the verbal and semantic fluency task, which is not subject to practice effects [92, 93]. Mavaddat et al. [10] followed aSAH patients with a favorable neurological outcome (i.e., GOS categories of moderate disability and good recovery) between 6 and 24 months after aSAH. Despite patients having a favorable neurological outcome, 76 % of aSAH survivors were significantly impaired on the verbal and semantic fluency task, indicating that overall patient status, as measured by the GOS, may not be an accurate indicator of language dysfunction after aSAH.
Visuospatial Function
Visuospatial function refers to one’s capacity for perception and spatial reasoning. According to several investigators [35, 45], visuospatial function is the least frequently impaired domain after aSAH, with an impairment prevalence of approximately 25 %. Furthermore, any visuospatial impairments that patients do exhibit tend to be mild and close to normative limits [40, 53]. Anterior aneurysms, the presence of blood in the Sylvian fissure, edema, older age, and right hemisphere lesions are significant predictors of poorer visuospatial function after aSAH [35, 69, 95]. Unlike other cognitive functions, deficits in visuospatial function persist over the 1-year period after aSAH [40, 58]. Although less is known about the integrity of visuospatial function after aSAH compared to other cognitive domains, several studies indicate that one test of visuospatial function—the Rey-Osterrieth Complex Figure Test—is the most sensitive test of long-term cognitive functioning in aSAH survivors (i.e., up to 5 years post-ictus) [40, 43].
Functional Outcome
Neuropsychological assessments attempt to characterize performance in individual cognitive domains. Day-to-day behavior, however, involves an interplay between many different cognitive domains rather than single cognitive domains working in isolation. Functional outcome encompasses activities of daily living (ADLs), instrumental activities of daily living (IADLs), and the ability to return to work. Each of these domains will be addressed in turn.
Activities of Daily Living
ADLs are those one performs for self-care [96]. Examples of ADLs include feeding, grooming, dressing, bathing, personal hygiene, and toileting. Aneurysmal SAH-associated ADL deficits are less common compared to cognitive deficits, with impairment ranging from 4 to 12 % [25, 72, 97, 98]. Severity of aSAH, as measured by Hunt and Hess grade [29], and hydrocephalus have been shown to predict ADL impairment after aSAH [99]. Performance on ADLs is key for patients’ perceptions of recovery; one recent study showed that ADL performance best differentiated aSAH survivors who reported making a complete recovery from those who reported disability [94]. Common ADL impairments at hospital discharge include incontinence and maintaining personal hygiene [100], but whether these deficits extend to longer follow-up periods remains unclear. Berry et al. [51] showed that the degree of ADL dysfunction correlated with the extent of memory impairment. Similarly, Mayer et al. [45] found deficits of visual memory, visuospatial function, and psychomotor functioning to be significantly associated with impairment in ADL at 3 months post-aSAH, thereby highlighting the link between cognition and functional outcome.
One concern with measuring ADLs after aSAH is that of ceiling effects. In studies that measure ADLs using the Barthel Index [101], over 95 % of assessed patients achieve the highest possible score [102]. Furthermore, many ADL measures (e.g., the Barthel Index, the Katz Index of Independence in ADLs [103]) rely heavily on patient self-report, the accuracy of which is uncertain. For instance, patients may be uncomfortable or embarrassed at disclosing difficulties with toileting or bathing. Thus, the specific profile of ADL impairments after aSAH remains unclear.
Instrumental Activities of Daily Living
IADLs are more complex than ADLs and include tasks like managing finances, shopping, and housekeeping [104]. IADLs are more frequently impaired than ADLs after aSAH, with an estimated prevalence of 44–93 % [12, 31, 105, 106]. Of all IADLs, driving appears to be the one in which patients show the most impairment, with up to 60 % of aSAH survivors requiring assistance [107]. Housekeeping difficulties are also common, as only 51 % of aSAH survivors are capable of managing their households without any limitations [15]. Deficits of visual memory, visuospatial function, language function, and psychomotor function are associated with IADL impairment [45, 94]. Similar to ADLs, the instruments used to measure IADLs may not be sensitive to the cognitive difficulties aSAH survivors may experience. While driving on a busy city street, for instance, aSAH survivors might experience transient lapses of concentration or feelings of being overwhelmed. Despite these subtle difficulties, however, patients would receive the maximum favorable score on the Mode of Transportation subscale of the Lawton IADL scale [104], as their performance fulfills the criteria of traveling independently. Furthermore, commonly used measures of IADL performance, like the Lawton IADL scale, often employ a binary scoring system that does not allow for different gradients of IADL performance. IADL measures also rely heavily on self-report, which may not accurately reflect patients’ true performance capabilities. Patients may be reluctant to disclose difficulties with driving, for instance, because they fear having their driver’s license suspended. Additional research is needed to characterize the specific IADL profile in aSAH survivors.
Return to Work
One of the most important components of day-to-day functioning is the ability to return to one’s previous occupation. This is especially important in the case of aSAH, as many aSAH survivors are young and have financial responsibilities and families to support. Among patients who were employed prior to aSAH, up to 40 % are unable to return to their previous occupation [14, 66, 80, 97, 108–111]. Other studies have found less favorable results, demonstrating that only 6–17 % of patients return to their previous occupation [32, 106, 112]. Even among those who do return to work, however, up to 59 % report reduced working capacity [15]. Return to work is an important issue even among patients with mild cognitive deficits; Haug et al. [30] found that only 21 % of previously employed aSAH patients with mild cognitive dysfunction were able to resume full-time employment. Patients frequently return to jobs with less responsibility, and they must often work fewer hours [14, 19, 32, 110, 111]. The impact of fatigue is profound, for up to 34 % of patients require daytime naps in order to function normally [20]. Research by Cedzich and Roth [15] indicates that, among patients who return to work, most do so between 6 and 12 months post-aSAH. Interestingly, patients’ employment status prior to aSAH has been shown to predict the extent of cognitive impairment 1-year post-ictus. Haug et al. [30] observed that the fraction of patients working full-time prior to hemorrhage was less among patients with severe cognitive impairment than among those with mild cognitive impairment 1 year after aSAH. Although only correlational, these results suggest that one’s resources before aSAH influence the course of post-stroke cognitive recovery.
Return to work and working ability are also influenced by aneurysm location and focal brain lesions. Unlike cognition, in which aneurysm location is less predictive of the profile of cognitive impairment [46, 53, 66, 74–76], return to work is greater among patients with middle cerebral artery aneurysms than among those with ACoA aneurysms [86]. Additionally, Vilkki et al. [66] found that left hemisphere lesions from aSAH were associated with failure to return to work and significantly reduced working ability. Self-reported planning and reasoning impairments and poorer performance on tests of executive function were also associated with failure to return to work. Unfortunately, although the investigators observed a correlation between left hemisphere lesions and failure to return to work, they did not examine language function in their sample, a cognitive domain predominantly mediated by the left hemisphere [113].
Additional Factors Affecting Outcome
Clipping vs. Coiling
There has been debate over the effects of microsurgical clipping and endovascular coiling of ruptured aneurysms on cognitive and functional outcome (Fig. 10.3). A randomized clinical trial, the International Subarachnoid Aneurysm Trial (ISAT), suggested that clinical outcome, as measured by the modified Rankin scale [114], was better after coiling than clipping [115].
(a) Surgical clipping of an aneurysm. Figure adapted from the University of Illinois College of Medicine at Chicago. Figure adapted with permission from Brisman JL, Song JK, Newell DW. Cerebral aneurysms. N Engl J Med. 2006;355(9):928–939. (b) Endovascular coiling of an aneurysm. Figure adapted from Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354:387–396
With respect to cognitive function, most studies indicate that verbal memory, visual memory, visuospatial function, attention, executive function, information processing speed, psychomotor function, language, and return to work are similar in patients treated by clipping or coiling [19, 39, 48, 58, 80, 116–118]. Several studies, however, have demonstrated that clipping is associated with poorer executive function, visual memory, and verbal memory compared to coiling [48, 80, 119, 120]. Bendel et al. [85], for instance, observed executive dysfunction in 73 % of clipped patients but in only 27 % of coiled patients. Why clipping is associated with greater cognitive impairment in these studies is unclear. Patients were not randomly assigned to clipping or coiling treatment, so differences in baseline risk for cognitive impairment cannot be excluded. One possibility is that clipped patients may have more brain injury. Hadjivassiliou et al. [120] found that 48 % of clipped patients suffered from encephalomalacia, compared to 0 % of coiled patients. Moreover, 87 % of clipped patients had infarcts compared to 57 % of coiled patients. Similarly, Bendel et al. [121] observed more frequent lesions after clipping than after coiling, particularly in the frontal lobes (70 % and 51 % had lesions after clipping and coiling, respectively) and the temporal lobes (48 % and 22 % had lesions after clipping and coiling, respectively).
Not all studies, however, have found an association between clipping and greater cognitive impairment. Santiago-Ramajo et al. [117, 122] observed poorer verbal and visual memory among coiled patients compared to clipped patients 4 months after aSAH. Likewise, Frazer et al. [39] found that coiled patients performed significantly poorer on tests of visuospatial function, executive function, and information processing speed 6 months after aSAH compared to clipped patients. Studies that observed poorer outcome among coiled patients examined cognitive performance within 6 months of SAH. Of the four studies that observed poorer outcome among clipped patients [48, 80, 119, 120], three examined cognitive function at least 1 year after SAH. Clipping and coiling may thus have different effects on cognitive outcome depending on time since treatment, with clipped patients having superior cognitive outcome in the short term and coiled patients having superior cognitive outcome in the long term. This hypothesis is consistent with data from Santiago-Ramajo et al. [122], who found that the rate of cognitive recovery between 4 and 12 months post-aSAH was greater for coiled patients than for clipped patients. Future studies should investigate the relative efficacy of clipping and coiling on cognitive and functional outcome over longer durations.
To what extent do clipping or coiling per se affect cognitive and functional outcome? Insight into this question can be provided by examining patients with pSAH, who have SAH but do not undergo clipping or coiling. Early studies investigating outcome after pSAH reported a favorable prognosis, with no change in quality of life or return to work [123, 124]. More recent reports, however, indicate that pSAH may not be as benign as previously believed. In one study, 62 % of pSAH survivors experienced headaches, depression, and forgetfulness on average 23 months post-pSAH [125]. Additionally, only 41 % of survivors were able to return to their previous occupations. Madureira et al. [126] observed minor cognitive impairments in 72 % of pSAH survivors and depression in 33 % at 39 months post-pSAH. These findings suggest that poor cognitive and functional outcome cannot be explained by surgical or endovascular procedures alone. Indeed, data by Hillis and colleagues [75] indicate that patients with aSAH who have undergone aneurysm clipping have poorer verbal and visual memory than patients who have undergone clipping of unruptured aneurysms, suggesting that extravasation of blood per se has detrimental effects on cognition. Surgical and endovascular procedures may not be innocuous, however; Hütter et al. [38] showed that, compared to SAH patients who were treated conservatively, patients who were treated surgically tended to exhibit poorer concentration. Patients in this study, however, were only examined in the acute phase (i.e., 6 days post-ictus) and it is unclear whether this difference would have persisted in the long term.
Neuroimaging
Many studies have found neuroanatomical changes accompanying SAH. Kivisaari et al. [68] found that CT, though useful as a diagnostic tool, was less sensitive than MRI in detecting lesions after aSAH. CT detected lesions in 57 % of patients, whereas MRI detected lesions in 81 % of patients. Most of this difference in sensitivity can be attributed to detecting frontal lobe lesions; CT only revealed frontal lobe injury in 16 % of cases, whereas MRI revealed frontal lobe injury in 48 % of cases. Other studies using SPECT have observed reduced cerebral perfusion after aSAH, particularly in subcortical regions and, in the case of ACoA aneurysm patients, anterior cortical areas [127]. Egge et al. [74] found that cerebral perfusion as measured by SPECT correlated with the degree of cognitive deficit post-aSAH, but the investigators only used composite scores of cognitive impairment and did not stratify by cognitive domain.
MRI studies have largely been limited to gross measures of atrophy such as ratios of grey matter volume to intracranial volume. Consistent with the hypothesis that aSAH causes diffuse brain injury, Bendel et al. [84, 85] observed gross brain atrophy and ventriculomegaly. The degree of gross brain atrophy predicted impairment in several domains, including memory, executive function, and language. Among a cohort of patients with anterior cerebral artery aneurysms, the degree of atrophy was greatest in frontal regions, namely the orbitofrontal cortex, the inferior frontal gyrus, the gyrus rectus, and thalamic and hypothalamic regions [85]. Increased risk of frontal lobe damage in patients with aneurysms of the anterior circulation is consistent with data by Rabinstein et al. [128], who showed that infarct location predicted aneurysm location in 77 % of cases. Future studies should extend these findings by examining how lesions to specific brain areas contribute to cognitive dysfunction.
Summary
Studies show that a high percentage of patients with aSAH have long-standing or permanent deficits in attention, memory, executive function, language, visuospatial function, IADLs, and returning to work. The variability in reported rates is likely due to multiple factors such as varying patient populations tested, different times of testing after aSAH, and different tests and definitions of abnormal performance on the tests. Subtle cognitive and real-world deficits that accompany aSAH often go undetected by gross outcome measures like the GOS. As a result, patients who are classified as having made a “good recovery” continue to experience deficits particularly in memory, executive function, and language many years after aSAH. These patients frequently cannot go back to work and often experience reduced life satisfaction. By raising clinical awareness about residual impairments in cognition and day-to-day functioning, it is our hope that clinicians and researchers will move toward developing comprehensive rehabilitation strategies that target these subtle yet debilitating symptoms.
References
van Gijn J, Rinkel GJE. Subarachnoid hemorrhage: diagnosis, causes and management. Brain. 2001;124:249–78.
Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354:387–96.
Feigin VL, Rinkel GJE, Lawes CMM, Algra A, Bennett DA, van Gijn J, et al. Risk factors for subarachnoid hemorrhage: an updated systematic review of epidemiological studies. Stroke. 2005;36:2773–80.
King Jr JT. Epidemiology of aneurysmal subarachnoid hemorrhage. Neuroimaging Clin N Am. 1997;7:659–68.
Østbye T, Levy AR, Mayo NE. Hospitalization and case-fatality rates for subarachnoid hemorrhage in Canada from 1982 through 1991. Stroke. 1997;28:793–8.
Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009;8:355–69.
Lovelock CE, Rinkel GJE, Rothwell PM. Time trends in outcome of subarachnoid hemorrhage. Population-based study and systematic review. Neurology. 2010;74:1494–501.
Feigin VL, Lawes CMM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2:43–53.
Johnston SC, Selvin S, Gress DR. The burden, trends, mortality from and demographics of subarachnoid hemorrhage. Neurology. 1998;50:1413–8.
Mavaddat N, Sahakian BJ, Hutchinson PJA, Kirkpatrick PJ. Cognition following subarachnoid hemorrhage from anterior communicating artery aneurysm: relation to timing of surgery. J Neurosurg. 1999;91:402–7.
Rinkel GJ, Algra A. Long-term outcomes of patients with aneurysmal subarachnoid haemorrhage. Lancet Neurol. 2011;10:349–56.
Powell J, Kitchen N, Heslin J, Greenwood R. Psychosocial outcomes at three and nine months after good neurological recovery from aneurysmal subarachnoid haemorrhage: predictors and prognosis. J Neurol Neurosurg Psychiatry. 2002;72:772–81.
Benke T, Koylu B, Delazer M, Trinka E, Kemmler G. Cholinergic treatment of amnesia following basal forebrain lesion due to aneurysm rupture—an open-label pilot study. Eur J Neurol. 2005;12:791–6.
Wermer MJH, Kool H, Albrecht KW, Rinkel GJE. Subarachnoid hemorrhage treated with clipping: long-term effects on employment, relationships, personality and mood. Neurosurgery. 2007;60:91–8.
Cedzich C, Roth A. Neurological and psychosocial outcome after subarachnoid haemorrhage, and the hunt and hess scale as a predictor of clinical outcome. Zentralbl Neurochir. 2005;66:112–8.
Hütter BO, Gilsbach JM. Which neuropsychological deficits are hidden behind a good outcome (Glasgow = I) after aneurysmal subarachnoid hemorrhage? Neurosurgery. 1993;33:999–1005.
Passier PECA, Visser-Meily JMA, van Zandvoort MJE, Post MWM, Rinkel GJE, van Heugten C. Prevalence and determinants of cognitive complaints after aneurysmal subarachnoid hemorrhage. Cerebrovasc Dis. 2010;29:557–63.
Ljunggren B, Sonesson B, Säveland H, Brandt L. Cognitive impairment and adjustment in patients without neurological deficits after aneurysmal SAH and early operation. J Neurosurg. 1985;62:673–9.
Schuiling WJ, Rinkel GJE, Walchenbach R, de Weerd AW. Disorders of sleep and wake in patients after subarachnoid hemorrhage. Stroke. 2005;36:578–82.
Sonesson B, Ljunggren B, Säveland H, Brandt L. Cognition and adjustment after late and early operation for ruptured aneurysm. Neurosurgery. 1987;21:279–87.
McKenna P, Willison JR, Lowe D, Neil-Dwyer G. Recovery after subarachnoid haemorrhage. Br Med J. 1989;299:485–7.
Ravnik J, Starovasnik B, Šešok S, Pirtosek Z, Svigelj V, Bunc G, et al. Long-term cognitive deficits in patients with good outcomes after aneurysmal subarachnoid hemorrhage from anterior communicating artery. Croat Med J. 2006;47:253–63.
Cheng H, Shi J. Neuropsychological evaluations and cognitive deficits in patients with aneurysmal SAH. Chin J Clin Psychol. 2005;13:86–7.
Cheng H, Shi J, Zhou M. Cognitive assessment in Chinese patients with aneurysmal subarachnoid hemorrhage. Behav Neurol. 2006;17:117–20.
Noble AJ, Baisch S, Mendelow AD, Allen L, Kane P, Schenk T. Posttraumatic stress disorder explains reduced quality of life in subarachnoid hemorrhage patients in both short and long term. Neurosurgery. 2008;63:1095–105.
Hütter BO, Gilsbach JM. Introspective capacities in patients with cognitive deficits after subarachnoid hemorrhage. J Clin Exp Neuropsychol. 1995;17:499–517.
Hütter BO, Gilsbach JM, Kreitschmann I. Quality of life and cognitive deficits after subarachnoid haemorrhage. Br J Neurosurg. 1995;9:465–75.
Thompson JN, Sheldrick R, Berry E. Cognitive and mental health difficulties following subarachnoid hemorrhage. Neuropsychol Rehabil. 2011;21:92–102.
Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg. 1968;28:14–20.
Haug T, Sorteberg A, Finset A, Lindegaard KF, Lundar T, Sorteberg W. Cognitive functioning and health-related quality of life 1 year after aneurysmal subarachnoid hemorrhage in preoperative comatose patients (Hunt and Hess Grade V patients). Neurosurgery. 2010;66:474–84.
Powell J, Kitchen N, Heslin J, Greenwood R. Psychosocial outcomes at 18 months after good neurological recovery from aneurysmal subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2004;75:1119–24.
Buchanan KM, Elias LJ, Goplen GB. Differing perspectives on outcome after subarachnoid haemorrhage: the patient, the relative, the neurosurgeon. Neurosurgery. 2000;46:831–8.
Ogden JA, Mee EW, Henning M. A prospective study of impairment of cognition and memory and recovery after subarachnoid hemorrhage. Neurosurgery. 1993;33:572–86.
Fisher C, Kistler J, Davis J. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery. 1980;6:1–9.
Kreiter KT, Copeland D, Bernardini GL, Bates JE, Peery S, Claassen J, et al. Predictors of cognitive dysfunction after subarachnoid hemorrhage. Stroke. 2002;33:200–9.
Egge A, Waterloo K, Sjøholm H, Solberg T, Ingebrigtsen T, Romner B. Prophylactic hyperdynamic postoperative fluid therapy after aneurysmal subarachnoid hemorrhage: a clinical, prospective, randomized, controlled study. Neurosurgery. 2001;49:593–606.
Hütter BO, Gilsbach JM. Early neuropsychological sequelae of aneurysm surgery and subarachnoid hemorrhage. Acta Neurochir (Wien). 1996;138:1370–8.
Hütter BO, Kreitschmann-Andermahr I, Gilsbach JM. Cognitive deficits in the acute stage after subarachnoid hemorrhage. Neurosurgery. 1998;43:1054–65.
Frazer D, Ahuja A, Watkins L, Cipolotti L. Coiling versus clipping for the treatment of aneurysmal subarachnoid hemorrhage: a longitudinal investigation into cognitive outcome. Neurosurgery. 2007;60:434–42.
Penninx JF, Visser-Meily JMA, Passier PECA, Rinkel GJE, Post MW, Van Zandvoort MJE. The prognostic value of neuropsychological examination after SAH. Behav Neurol. 2010;23:173–5.
Mustonen T, Koivisto T, Vanninen R, Hänninen T, Vapalahti M, Hernesniemi J, et al. Heterogeneity of cerebral perfusion 1 week after haemorrhage is an independent predictor of clinical outcome in patients with aneurysmal subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2008;79:1128–33.
Bendel P, Koivisto T, Hänninen T, Kolehmainen A, Könönen M, Hurskainen H, et al. Subarachnoid hemorrhage is followed by temporomesial volume loss. Neurology. 2006;67:575–82.
Ogden JA, Utley T, Mee EW. Neurological and psychosocial outcome 4 to 7 years after subarachnoid hemorrhage. Neurosurgery. 1997;41:25–34.
Barth M, Thomé C, Schmiedek P, Weiss C, Kasuya H, Vajcokzy P. Characterization of functional outcome and quality of life following subarachnoid hemorrhage in patients treated with and without nicardipine prolonged-release implants. J Neurosurg. 2009;110:955–60.
Mayer SA, Kreiter KT, Copeland D, Bernardini GL, Bates JE, Peery S, et al. Global and domain-specific cognitive impairment and outcome after subarachnoid hemorrhage. Neurology. 2002;59:1750–8.
Ørbo M, Waterloo K, Egge A, Isaksen J, Ingebrigtsen T, Romner B. Predictors for cognitive impairment one year after surgery for aneurysmal subarachnoid hemorrhage. J Neurol. 2008;255:1770–6.
Martinaud O, Perin B, Gérardin E, Proust F, Bioux S, Gars DL, et al. Anatomy of executive deficit following ruptured anterior communicating artery aneurysm. Eur J Neurol. 2009;16:595–601.
Proust F, Martinaud O, Gérardin E, Derrey S, Levèque S, Bioux S, et al. Quality of life and brain damage after microsurgical clip occlusion or endovascular coil embolization for ruptured anterior communicating artery aneurysms: neuropsychological assessment. J Neurosurg. 2009;110:19–29.
Romner B, Sonesson B, Ljunggren B, Brandt L, Säveland H, Holtås S. Late magnetic resonance imaging related to neurobehavioral functioning after aneurysmal subarachnoid hemorrhage. Neurosurgery. 1989;25:390–7.
Drake CG. Report of World Federation of Neurological Surgeons Committee on a universal subarachnoid hemorrhage grading scale. J Neurosurg. 1988;68:985–6.
Berry E, Jones RA, West CG, Brown JD. Outcome of subarachnoid haemorrhage. An analysis of surgical variables, cognitive and emotional sequelae related to SPECT scanning. Br J Neurosurg. 1997;11:378–87.
Richardson JTE. Performance in free recall following rupture and repair of intracranial aneurysm. Brain Cogn. 1989;9:210–26.
Haug T, Sorteberg A, Sorteberg W, Lindegaard K, Lundar T, Finset A. Cognitive outcome after subarachnoid hemorrhage: time course of recovery and relationship to clinical, radiological and management parameters. Neurosurgery. 2007;60:649–57.
Elwood RE. The California Verbal Learning Test: psychometric characteristics and clinical application. Neuropsychol Rev. 1995;5:173–7.
Wechsler D. Wechsler memory scale-revised. San Antonio, TX: The Psychological Corporation; 1987.
Osterrieth PA. Le test de copie d’une figure complexe. Arch Psychol. 1944;30:206–356.
Rey A. L’examen psychologique dans les cas d’encéphalopathie traumatique. Arch Psychol. 1941;28:286–340.
Koivisto T, Vanninen R, Hurskainen H, Saari T, Hernesniemi J, Vapalahti M. Outcomes of early endovascular versus surgical treatment of ruptured cerebral aneurysms: a prospective randomized study. Stroke. 2000;31:2369–77.
Graetz D, Nagel A, Schlenk F, Sakowitz O, Vajkoczy P, Sarrafzadeh A. High ICP as trigger of proinflammatory IL-6 cytokine activation in aneurysmal subarachnoid hemorrhage. Neurol Res. 2010;32:728–35.
Chaichana KL, Pradilla G, Huang J, Tamargo RJ. Role of inflammation (leukocyte-endothelial cell interactions) in vasospasm after subarachnoid hemorrhage. World Neurosurg. 2010;73:22–41.
D’Esposito M, Alexander MP, Fischer R, McGlinchey-Berroth R, O’Connor M. Recovery of memory and executive function following anterior communicating artery aneurysm rupture. J Int Neuropsychol Soc. 1996;2:565–70.
Rushworth MF, Kennerley SW, Walton ME. Cognitive neuroscience: resolving conflict in and over the medial frontal cortex. Curr Biol. 2005;15:R54–6.
Stuss DT, Alexander MP, Hamer L, Palumbo C, Dempster R, Binns M, et al. The effects of focal anterior and posterior brain lesions on verbal fluency. J Int Neuropsychol Soc. 1998;4:265–78.
Richardson JTE. Cognitive performance following rupture and repair of intracranial aneurysm. Acta Neurol Scand. 1991;83:110–22.
Squire LR, Stark CEL, Clark RE. The medial temporal lobe. Annu Rev Neurosci. 2004;27:279–306.
Vilkki JS, Juvela S, Siironen J, Ilvonen T, Varis J, Porras M. Relationship of local infarctions to cognitive and psychosocial impairments after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2004;55:790–803.
Fletcher PC, Henson RNA. Frontal lobes and human memory: insights from functional neuroimaging. Brain. 2001;124:849–81.
Kivisaari RP, Salonen O, Servo A, Autti T, Hernesniemi J, Öhman J. MR imaging after aneurysmal subarachnoid hemorrhage and surgery: a long-term follow-up study. AJNR Am J Neuroradiol. 2001;22:1143–8.
Vilkki J, Holst P, Öhman J, Servo A, Heiskanen O. Cognitive deficits related to computed tomographic findings after surgery for a ruptured intracranial aneurysm. Neurosurgery. 1989;25:166–72.
Stuss DT, Levine B. Adult clinical neuropsychology: lessons from studies of the frontal lobes. Annu Rev Psychol. 2002;53:401–33.
Anderson SW, Todd MM, Hindman BJ, Clarke WR, Torner JC, Tranel D, IHAST Investigators, et al. Effects of intraoperative hypothermia on neuropsychological outcomes after intracranial aneurysm surgery. Ann Neurol. 2006;60:518–27.
Noble AJ, Schenk T. Posttraumatic stress disorder in the family and friends of patients who have suffered spontaneous subarachnoid hemorrhage. J Neurosurg. 2008;109:1027–33.
Akyuz M, Erylmaz M, Ozdemir C, Goksu E, Ucar T, Tuncer R. Effect of temporary clipping on frontal lobe functions in patients with ruptured aneurysm of the anterior communicating artery. Acta Neurol Scand. 2005;112:293–7.
Egge A, Waterloo K, Sjøholm H, Ingebrigtsen T, Forsdahl S, Jacobsen EA, et al. Outcome 1 year after aneurysmal subarachnoid hemorrhage: relation between cognitive performance and neuroimaging. Acta Neurol Scand. 2005;112:76–80.
Hillis AE, Anderson N, Sampath P, Rigamonti D. Cognitive impairments after surgical repair of ruptured and unruptured aneurysms. J Neurol Neurosurg Psychiatry. 2000;69:608–15.
Samra SK, Giordani B, Caveney AF, Clarke WR, Scott PA, Anderson S, et al. Recovery of cognitive function after surgery for aneurysmal subarachnoid hemorrhage. Stroke. 2007;38:1864–72.
Manning L, Pierot L, Dufour A. Anterior and non-anterior ruptured aneurysms: memory and frontal lobe function performance following coiling. Eur J Neurol. 2005;12:466–74.
Shallice T. Specific impairments of planning. Philos Trans R Soc Lond B Biol Sci. 1982;298:199–209.
Papagno C, Rizzo S, Ligori L, Lima J, Riggio A. Memory and executive functions in aneurysms of the anterior communicating artery. J Clin Exp Neuropsychol. 2003;25:24–35.
Bellebaum C, Schäfers L, Schoch B, Wanke I, Stolke D, Forsting M, et al. Clipping versus coiling: neuropsychological follow up after aneurysmal subarachnoid haemorrhage (SAH). J Clin Exp Neuropsychol. 2004;26:1081–92.
Salmond CH, DeVito EE, Clark L, Menon DK, Chatfield DA, Pickard JD, et al. Impulsivity, reward sensitivity, and decision-making in subarachnoid hemorrhage survivors. J Int Neuropsychol Soc. 2006;12:697–706.
Uski TK, Lilja Å, Säveland H, Ekman R, Sonesson B, Brandt L. Cognitive functioning and cerebrospinal fluid concentrations of neuropeptides for patients with good neurological outcomes after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2000;47:812–8.
Cahill J, Zhang JH. Subarachnoid hemorrhage: is it time for a new direction? Stroke. 2009;40:S86–7.
Bendel P, Koivisto T, Aikiä M, Niskanen E, Könönen M, Hänninen T, et al. Atrophic enlargement of CSF volume after subarachnoid hemorrhage: correlation with neuropsychological outcome. AJNR Am J Neuroradiol. 2010;31:370–6.
Bendel P, Koivisto T, Niskanen E, Könönen M, Aikiä M, Hänninen T, et al. Brain atrophy and neuropsychological outcome after treatment of ruptured anterior cerebral artery aneurysms: a voxel-based morphometric study. Neuroradiology. 2009;51:711–22.
Haug T, Sorteberg A, Sorteberg W, Lindegaard K, Lundar T, Finset A. Cognitive functioning and health related quality of life after rupture of an aneurysm on the anterior communicating artery versus middle cerebral artery. Br J Neurosurg. 2009;23:507–15.
Nelson HE. A modified card sorting test sensitive to frontal lobe defects. Cortex. 1976;12:313–24.
Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18:643–62.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–4.
Shallice T, Evans ME. The involvement of the frontal lobes in cognitive estimation. Cortex. 1978;14:294–303.
Desantis A, Laiacona M, Barbarotto R, Basso A, Villani R, Spagnoli D, et al. Neuropsychological outcome of patients operated upon for an intracranial aneurysm: analysis of general prognostic factors and of the effects of the location of the aneurysm. J Neurol Neurosurg Psychiatry. 1989;52:1135–40.
Dikmen SS, Heaton RK, Grant I, Temkin NR. Test-retest reliability and practice effects of expanded Halstead-Reitan Neuropsychological Test Battery. J Int Neuropsychol Soc. 1999;5:346–56.
Basso MR, Bornstein RA, Lang JM. Practice effects on commonly used measures of executive function across twelve months. Clin Neuropsychol. 1999;13:283–92.
Chahal N, Barker-Collo S, Feigin V. Cognitive and functional outcomes of 5-year subarachnoid haemorrhage survivors: comparison to matched healthy controls. Neuroepidemiology. 2011;37:31–8.
Satzger W, Niedermeier N, Schönberger J, Engel RR, Beck OJ. Timing of operation for ruptured cerebral aneurysm and long-term recovery of cognitive functions. Acta Neurochir (Wien). 1995;136:168–74.
Christiansen C, Baum C. Occupational therapy. Enabling function and well-being. Thorofare, NJ: Slack; 1997.
Hackett ML, Anderson CS. Health outcomes 1 year after subarachnoid hemorrhage: an international population-based study. Neurology. 2000;55:658–62.
Pasternak JJ, McGregor DG, Schroeder DR, Lanier WL, Shi Q, Hindman BJ, et al. Hyperglycemia in patients undergoing cerebral aneurysm surgery: its association with long-term gross neurologic and neuropsychological function. Mayo Clin Proc. 2008;83:406–17.
Dombovy ML, Drew-Cates J, Serdans R. Recovery and rehabilitation following subarachnoid haemorrhage. Part I: outcome after inpatient rehabilitation. Brain Inj. 1998;12:443–54.
Ślusarz R, Beuth W, Książkiewicz B. Postsurgical examination of functional outcome of patients having undergone surgical treatment of intracranial aneurysm. Scand J Caring Sci. 2009;23:130–9.
Mahoney F, Barthel D. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–5.
Kim DH, Haney CL, van Ginhoven G. Utility of outcome measures after treatment for intracranial aneurysms: a prospective trial involving 520 patients. Stroke. 2005;36:792–6.
Katz S, Down TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10:20–30.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86.
Fernandez A, Schmidt JM, Claassen J, Pavlicova M, Huddleston D, Kreiter KT, et al. Fever after subarachnoid hemorrhage: risk factors and impact on outcome. Neurology. 2007;68:1013–9.
Kirkness CJ, Thompson JM, Ricker BA, Buzaitis A, Newell DW, Dikmen S, et al. The impact of aneurysmal subarachnoid hemorrhage on functional outcome. J Neurosci Nurs. 2002;34:134–41.
Dombovy ML, Drew-Cates J, Serdans R. Recovery and rehabilitation following subarachnoid haemorrhage. Part II: long-term follow-up. Brain Inj. 1998;12:887–94.
Carter BS, Buckley D, Ferraro R, Rordorf G, Ogilvy CS. Factors associated with reintegration to normal living after subarachnoid hemorrhage. Neurosurgery. 2000;46:1326–33.
Haug T, Sorteberg A, Sorteberg W, Lindegaard KF, Lundar T, Finset A. Surgical repair of unruptured and ruptured middle cerebral artery aneurysms: impact on cognitive functioning and health-related quality of life. Neurosurgery. 2009;64:412–20.
Morris PG, Wilson JTL, Dunn L. Anxiety and depression after spontaneous subarachnoid hemorrhage. Neurosurgery. 2004;54:47–54.
Tomberg T, Orasson A, Linnamägi Ü, Toomela A, Pulver A, Asser T. Coping strategies in patients following subarachnoid haemorrhage. Acta Neurol Scand. 2001;104:148–55.
Hop JW, Rinkel GJE, Algra A, van Gijn J. Changes in functional outcome and quality of life in patients and caregivers after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2001;95:957–63.
Witelson SF, Pallie W. Left hemisphere specialization for language in the newborn: neuroanatomical evidence of asymmetry. Brain. 1973;96:641–6.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJA, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–7.
Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 2002;360:1267–74.
Mukerji N, Holliman D, Baisch S, Noble A, Schenk T, Nath F. Neuropsychologic impact of treatment modalities in subarachnoid hemorrhage: clipping is no different from coiling. World Neurosurg. 2010;74:129–38.
Santiago-Ramajo S, Katati MJ, Pérez-García M, Coín-Mejias MA, Vilar-Lopez R, Caracuel-Romero A, et al. Neuropsychological evaluation of the treatments applied to intracranial aneurysms in a Spanish sample. J Clin Exp Neuropsychol. 2007;29:634–41.
Wong GKC, Wong R, Mok VCT, Fan DS, Leung G, Wong A, et al. Clinical study on cognitive dysfunction after spontaneous subarachnoid haemorrhage: patient profiles and relationship to cholinergic dysfunction. Acta Neurochir. 2009;151:1601–7.
Fontanella M, Perozzo P, Ursone R, Garbossa D, Bergui M. Neuropsychological assessment after microsurgical clipping or endovascular treatment for anterior communicating artery aneurysm. Acta Neurochir. 2003;145:867–72.
Hadjivassiliou M, Tooth CL, Romanowski CAJ, Byrne J, Battersby RD, Oxbury S, et al. Aneurysmal SAH: cognitive outcome and structural damage after clipping or coiling. Neurology. 2001;56:1672–7.
Bendel P, Koivisto T, Könönen M, Hänninen T, Hurskainen H, Saari T, et al. MR imaging of the brain 1 year after aneurysmal subarachnoid hemorrhage: randomize study comparing surgical with endovascular treatment. Radiology. 2008;246:543–52.
Santiago-Ramajo S, Katati MJ, Pérez-García M, Arjona-Moron V. Evaluating the recovery of cognitive impairment in subarachnoid hemorrhage taking into consideration the practice effects. Neurosurgery. 2010;67:1497–504.
Brilstra EH, Hop JW, Rinkel GJE. Quality of life after perimesencephalic haemorrhage. J Neurol Neurosurg Psychiatry. 1997;63:382–4.
Rinkel GJ, Wijdicks EF, Vermeulen M, Hageman LM, Tans JT, van Gijn J. Outcome in perimesencephalic (nonaneurysmal) subarachnoid hemorrhage: a follow-up study in 37 patients. Neurology. 1990;40:1130–2.
Marquardt G, Niebauer T, Schick U, Lorenz R. Long term follow up after perimesencephalic subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2000;69:127–30.
Madureira S, Canhão P, Guerreiro M, Ferro JM. Cognitive and emotional consequences of perimesencephalic subarachnoid hemorrhage. J Neurol. 2000;415:862–7.
Tooth CL, Tindale WB, Hadjivassiliou M, Romanowski CA, Hunt E, Pantke R, et al. Subcortical hypoperfusion following surgery for aneurysmal subarachnoid haemorrhage: implications for cognitive performance? Behav Neurol. 2000;12:39–51.
Rabinstein AA, Friedman JA, Weigand SD, McClelland RL, Fulgham JR, Manno EM, et al. Predictors of cerebral infarction in aneurysmal subarachnoid hemorrhage. Stroke. 2004;35:1862–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Al-Khindi, T., Macdonald, R.L., Mayer, S., Schweizer, T.A. (2014). Behavior After Aneurysmal Subarachnoid Hemorrhage: Cognition and Functional Outcome. In: Schweizer, T., Macdonald, R. (eds) The Behavioral Consequences of Stroke. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-7672-6_10
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7672-6_10
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-7671-9
Online ISBN: 978-1-4614-7672-6
eBook Packages: MedicineMedicine (R0)