Abstract
Purpose
The Woven EndoBridge (WEB) can be used to treat wide-necked aneurysms without antiplatelet medications, suggesting it may have advantages in the setting of aneurysmal subarachnoid hemorrhage (aSAH). The goal was assessment of safety and efficacy of WEB in aSAH given the delayed nature of aneurysmal thrombosis.
Methods
An international retrospective analysis of patients with aSAH treated with WEB was conducted at 7 tertiary centers from 2016 to 2020. Outcomes included rates of rebleeding, retreatment, complications, and complete occlusion. Furthermore, a systematic review and meta-analysis was conducted from 2011 to 2020 assessing the same outcomes. All pooled event rates were calculated using a random effect model.
Results
Consecutive patients with aSAH harbored 25 aneurysms that were treated with 29 WEB devices. The mean age was 53 years, and 65% were female. Zero experienced rebleeding, 2 were retreated, 2 experienced complications, 16 were completely occluded at 3 months, and 21 were completed occluded at 9–12 months. Meta-analysis of 309 WEB treatments for aSAH from 7 case series revealed 2.5% (95% CI 1–5%) had rebleeding, 9% (95% CI 4–17%) were retreated, 17% (95% CI 10–30%) had complications, and 61% (95% CI 51–71%) were completely occluded at 3–6 months.
Conclusion
WEB embolization in the setting of aSAH provides similar protection against rebleeding with comparable retreatment rates to traditional approaches. However, there is a higher rate of incomplete radiographic occlusion and operative complications compared to WEB embolization of unruptured aneurysms. Long-term prospective studies are needed to fully delineate the role of WEB embolization in aSAH.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the past decades, the treatment paradigm for ruptured intracranial aneurysms in the setting of aneurysmal subarachnoid hemorrhage (aSAH) has shifted towards endovascular techniques [1,2,3,4]. Among them, coil embolization has demonstrated improved functional outcomes and survival [5]. However, not all aneurysms are amenable to primary coil embolization, especially wide-neck bifurcation aneurysms. For instance, aneurysms with unfavorable dome-to-neck ratios often require the use of adjunctive devices such as balloons or stents which are associated with increased treatment risk. Additionally, the use of stents requires dual antiplatelet therapy (DAPT) due to the risk of thromboembolic complications, increasing the possibility of hemorrhagic events in the acute aSAH period [6,7,8]. The Woven EndoBridge (WEB) device (MicroVention, Aliso Viejo, CA) was introduced in Europe in 2010 and subsequently approved by the US Food and Drug Administration (FDA) in 2018 for internal carotid artery (ICA) terminus, middle cerebral artery (MCA) bifurcation, anterior communicating artery (ACoA), and basilar tip aneurysms (BTA) with a neck diameter > 4 mm or a dome-to-neck ratio of 1–2, and a dome diameter of 3–10 mm [9,10,11]. The WEB is a self-expanding, braided 3D mesh of nitinol wires in either a spherical or cylindrical shape that is placed within the aneurysm. The high metal surface area coverage at the neck of the aneurysm results in intrasaccular flow disruption with thrombosis and subsequent endothelialization across the neck of the aneurysm [12].
Given the lack of a stent or foreign material in the parent vessel following intrasaccular WEB deployment, there is no need for prolonged antiplatelet therapy which may prove the WEB device a valuable alternative for securing acutely ruptured, wide-necked intracranial aneurysms. However, while there are robust data supporting the use of WEB in unruptured aneurysms, less evidence exists for their use in acutely ruptured aneurysms. The purpose of the current study is to assess rates of rebleeding, retreatment, complications, and complete occlusion after WEB treatment for ruptured intracranial aneurysms in a case series from 2 multidisciplinary neurointerventional practices covering a total of 7 tertiary care centers and conduct an updated meta-analysis of the available literature.
Methods
Case series
This study was approved by the local institutional review boards. Informed consent was waived based on minimal patient risk and practical inability to perform this study without such a waiver. An international retrospective analysis was conducted at 7 tertiary care medical centers in the USA and Colombia. Consecutive patients were included in the study if they presented with aSAH for which the WEB device was used as the primary means of treatment within 7 days of rupture over a 4-year period spanning between January 1, 2016 and April 1, 2020. Pertinent patient demographic, clinical, and radiologic information, including Hunt & Hess and modified Fisher scores, was collected from the medical record [13, 14]. Aneurysm size, location and morphology were determined from catheter angiograms.
The decision to treat with the WEB device was made based on a combination of clinical and radiologic factors including patient demographics, aneurysm size, location, and morphology. Standard local procedures were followed at each site. All procedures were performed via a transfemoral approach. WEBs were deployed through a 0.021-, 0.027-, or 0.033-inch diameter microcatheter per the manufacturer protocol, depending on device size (VIA Microcatheter, MicroVention, Aliso Viejo, CA). The use of distal access catheters and WEB device sizing was at the discretion of each treating neurointerventionalist. No antiplatelet or anticoagulation therapy was used in the peri- or postoperative period unless indicated for other medical reasons.
Outcomes included rates of rebleeding, retreatment, procedure-related complications, and complete occlusion. Rebleeding was defined as any new or enlarging subarachnoid hemorrhage during the admission. Retreatment was defined as the need for an additional intervention to treat the aneurysm and most commonly involved the addition of a stent during the hospital course or clinical follow-up. Complications were classified as either major or minor. Major complications included death, intracranial hemorrhage (ICH), ischemic stroke, or retroperitoneal hematoma. Minor complications included transient ischemic attack (TIA), cranial neuropathy, and non-operative groin hematoma. All aneurysms were assessed for complete occlusion with follow-up angiography. The imaging modality and timing of follow-up angiographic imaging were neurointerventionalist-dependent but most commonly consisted of catheter angiography performed at 6, 12, and 18–24 months. If angiography demonstrated residual filling of the aneurysm neck (distinct from the device recess) [15] and/or dome, the aneurysm was categorized as not fully occluded.
Mean values with standard deviations were reported for continuous variables. Percent and count were reported for categorical variables. The data that support the findings of this study will be made available from the corresponding author upon reasonable request and pending approval of local institutional review boards.
Systematic review and meta-analysis
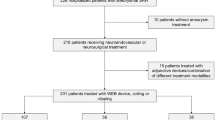
The search protocol, including hypotheses, outcomes, and inclusion/exclusion criteria, was developed a priori according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [16]. A literature search was performed using relevant key words to identify cases of ruptured aneurysms with aSAH that were treated by WEB embolization. The OVID Medline, Embase, Web of Science, and Cochrane Library databases were searched from inception to February 2020. The references of included publications were searched manually for other relevant papers. The following key words were used in combination: “rupture,” “aneurysm,” “subarachnoid hemorrhage,” “WEB embolization,” “Woven EndoBridge,” or “WEB.” The search was limited to articles in English.
Studies were included if they were randomized or had an observational prospective or retrospective study design, were dedicated to patients with ruptured aneurysms or in which outcomes for ruptured aneurysms were specifically and separately reported, and reported radiographic occlusion at any follow-up period. Outcomes included rates of rebleeding, retreatment, complications, and complete occlusion. Exclusion criteria included single case reports, non-peer-reviewed conference abstracts, review articles, and animal studies. Two reviewers (NMA and PH) performed title and abstract screening from the search query results. The full texts of eligible studies were obtained and reviewed for inclusion (PH); these results were then independently verified by a second reviewer (NMA). The quality of all eligible studies was evaluated independently and in duplicate by one reviewer (NMA), utilizing the 2011 Oxford Centre for Evidence-Based Medicine levels of evidence [17].
Pooled estimates and 95% confidence intervals (CI) were combined using a random-effects model. A p-value of less than 0.05 was interpreted as statistically significant. Publication bias was evaluated by visual inspection of funnel plots. The I2 test was used to assess heterogeneity between studies. I2 values greater than 40% were defined as significant heterogeneity between studies. Meta-regression was performed according to publication date to exclude the effect of early versus late usage. The meta-analysis was performed using the Comprehensive Meta-Analysis (CMA) software, version 3 (Biostat Inc., Englewood, NJ, USA).
Results
Case series
A total of 25 aneurysms were treated with the WEB device in the setting of aSAH at participating tertiary care centers in 25 patients (6 patients at Massachusetts General Hospital, Boston, USA, and 19 patients at AngioTeam Cerebrovascular, Medellín, Colombia) between 1/1/2016 and 4/1/2020. A total of 29 devices were opened (1.16 device per aneurysm) with more than one device opened in four cases. These 4 cases included 1 ICA terminus and 3 MCA aneurysms. In all cases, a second device was opened due to inadequate sizing of the device of the device at first attempt. The mean age of the 25 patients who underwent WEB treatment was 53 ± 16 years, and 64% of the cohort was female (Table 1).
The average aneurysm dome length was 5.84 mm (± 0.6) with an average width of 6.14 mm (± 0.5). Most treated aneurysms involved the anterior circulation (80%). Of all treated aneurysms, 16% arose from the anterior communicating artery, 16% arose from the ICA terminus, 48% arose from the MCA bifurcation, and 20% arose from the posterior circulation, from either the basilar tip (12%) or the superior cerebellar artery (8%).
No patients had rebleeding events during the hospitalization or at the time of last known follow-up. Two (8%) patients required retreatment with delayed placement of a flow diverter. Complications occurred in 2 (8%) cases, both of which were major and included intraoperative aneurysm rupture during aneurysm catheterization; one case was caused by the intermediate catheter and the second case by the microcatheter. Both cases were caused by tension being built within the construct (due in part to tortuous proximal anatomy) and sudden release of said tension causing the catheter to advance uncontrollably into the aneurysm. Complete aneurysm occlusion was observed in 16 (64%) at 3 months and 21 (84%) at 9–12 months post embolization. The mean follow-up time was 7.1 ± 5.5 months.
Systematic review and meta-analysis
Seven articles, all of which were observational case series, representing 309 ruptured aneurysms were identified and included in the final analysis [18,19,20,21,22,23,24]. All studies were observational retrospective analyses (Table 2) and therefore risk of bias was considered high since it cannot be excluded. Most of these aneurysms were in the anterior circulation (60%), and 85% of patients had good functional outcome at 3 months (mRs 0–2), a high rate which could partially relate to selection bias. Average follow-up time was 4 months. PPRIMA chart and data on each cohort are presented in detail in the Supplementary Material.
The likelihood of complete radiographic occlusion (Fig. 1) following WEB placement for ruptured aneurysms was 62% (95% CI 49–73%) at early 3–6 month angiographic follow-up. The rate of rebleeding was 2.5% (95% CI 1–5%) (Fig. 2). The overall retreatment rate was 9% (95% CI 4–17%), and the need for early or delayed stent placement was 5% (95% CI 1–12%). The pooled event rate for complications (procedural aneurysm rupture, thromboembolic, and device protrusion in the parent artery) across studies was 17% (95% CI 10–30%).
There was no effect of publication date as a predictor for complete occlusion rate among all series (Fig. 3). There was a significant heterogeneity (I2 > 40%) and publication bias in the studies reviewed for complete occlusion outcomes (Fig. 4), but not rebleeding and stent placement (I2 = 0%).
Discussion
We describe our case series from 2 multidisciplinary cerebrovascular practices comprising 7 tertiary care centers and present an updated meta-analysis of the available literature on WEB embolization for ruptured aneurysms in the setting of aSAH, including rates of rebleeding, retreatment, complications, and complete occlusion on follow-up. While there is a strong body of evidence supporting the use of WEB for unruptured, wide-neck bifurcation aneurysms [25,26,27], we present the first meta-analysis of these outcomes in the setting of aSAH.
In contrast to the treatment of unruptured aneurysms in which the main objective is complete aneurysmal occlusion, the treatment of ruptured aneurysms in the setting of aSAH seeks to prioritize securing the rupture site and prevent rebleeding. In our case series of WEB treatments in the setting of aSAH at 7 centers, there were no cases of rebleeding after treatment. Given our small sample size and limited follow-up, meta-analysis also focused on the greater literature surrounding such complications. Among the existing literature, our meta-analysis found rebleeding in 2.8% of cases treated with WEB. This is similar to rebleeding after primary coiling in the setting of aSAH which has rates of 1.4–3.5% [1, 28,29,30]. Two patients (8%) in our case series required retreatment with delayed placement of flow diverting stents. This rate was lower than that found in our meta-analysis of WEB treatments where 17% required retreatment overall and 5% required an early or delayed stent. In comparison, primary coil embolization has similar retreatment rates in the setting of aSAH [31, 32].
Regarding complications, we observed 2 (8%) intraoperative ruptures among the 25 aneurysms treated in our series. Our meta-analysis showed the pooled complication rate (including procedural aneurysm rupture, thromboembolic event, and device protrusion in the parent artery) across studies was 16%. In comparison, the complication rate of primary coiling in the setting of aSAH has been reported between 5.87% and 9.9% [32,33,34]. Furthermore, others have reported a 9% complication rate for WEB treatment of non-ruptured aneurysms, consisting of 4 thromboembolic events and 1 hemorrhagic event [35]. The lower rate of complications in the treatment of unruptured aneurysms may be explained by the fragility of intracranial vasculature secondary to the inflammation cascade generated by aSAH paired with the more rigid delivery systems required for WEB deployment. In addition, WEB use is in its nascence and must be carefully selected primarily for lesions where traditional treatment approaches such as assisted or stand-alone coiling is not possible/preferred and associated with elevated risk of complication or recurrence (e.g., carotid terminus). Operator learning curve and experience may play additional roles in the difference in complication rates between ruptured and unruptured aneurysms treated with WEB. Interestingly, the learning curve derived in this study is shallow. These studies might be subject to lead-time bias in which papers are only published once the senior author has fulfilled their learning curve and thus, despite the difference in year of publication, there might not be a difference in outcomes. Role-regression slopes are only pure when compared between the same operator or group of operators and not across geographically and regulatory-diverse environments.
At 3-month follow-up in our series, there was complete aneurysm occlusion in 64% of cases. However, by 9–12 months, this number increased to 84%. Our meta-analysis of WEB treatments for ruptured aneurysms revealed that the likelihood of complete occlusion was 62% at an average of 4 months post-treatment across the available literature which is in good agreement with our reported case series. Randomized trial data have shown complete occlusion in 66% on first follow-up angiogram after primary coiling in the setting of aSAH [32]. In the current case series, we report a retreatment rate of 8% which is double that reported in the published literature for unruptured aneurysms treated with WEB. Interestingly, unruptured aneurysms treated with WEB have demonstrated an occlusion rate of 88% after a mean follow-up interval of 11 months which is similar to the 84% occlusion rate that we report here at 9–12-month angiographic follow-up. These findings suggest that occlusion rates of ruptured aneurysms treated with WEB may ultimately approach those of unruptured aneurysms treated intrasaccular flow-diversion given a long enough period of longitudinal follow-up [26].
There are several limitations to this study. Given the retrospective design of our series and each of the included studies in our meta-analysis, these data are inherently subject to selection bias. Treatment approaches and imaging follow-up were at the discretion of treating clinicians. While our case series has a relatively small sample size, our meta-analysis includes all published cases of WEB embolization in the setting of aSAH to date. Still, there was a significant heterogeneity and publication bias for the radiographic occlusion and retreatment rate outcome. The wide confidence intervals suggest the need for larger, long-term prospective studies and randomized trials to further elucidate these findings. Future comparisons may include only wide-neck bifurcation aneurysms to compare WEB versus stent-assisted coiling.
Conclusion
The WEB device holds promise for the treatment of wide-neck bifurcation aneurysms, including those in the setting of acute rupture with aSAH. The importance of a reliable treatment option following aneurysm rupture, particularly for aneurysms that would otherwise require adjunctive stenting and antiplatelet therapy due to their location and morphology, cannot be overstated. The WEB device in aSAH appears to provide similar protection against rebleeding with comparable retreatment rates to traditional aneurysm treatment approaches in aSAH; however, there may be a slightly higher rate of incomplete radiographic occlusion and operative complications compared to WEB embolization for unruptured aneurysms. Long-term prospective studies and randomized trials are needed to fully delineate the role of WEB embolization in aSAH.
Abbreviations
- ACoA:
-
Anterior communicating artery
- aSAH:
-
Aneurysmal subarachnoid hemorrhage
- BTA:
-
Basilar tip aneurysms
- CI:
-
Confidence intervals
- DAPT:
-
Dual antiplatelet therapy
- FDA:
-
Food and Drug Administration
- ICA:
-
Internal carotid artery
- ICH:
-
Intracranial hemorrhage
- MCA:
-
Middle cerebral artery
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- TIA:
-
Transient ischemic attack
- WEB:
-
Woven EndoBridge
References
Molyneux A, Kerr R, Stratton I et al (2002) International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 360(9342):1267–1274. https://doi.org/10.1016/S0140-6736(02)11314-6
McDougall CG, Spetzler RF, Zabramski JM et al (2012) The barrow ruptured aneurysm trial: clinical article. J Neurosurg 116(1):135–144. https://doi.org/10.3171/2011.8.JNS101767
Andaluz N, Zuccarello M (2008) Recent trends in the treatment of cerebral aneurysms: analysis of a nationwide inpatient database. J Neurosurg 108(6):1163–1169. https://doi.org/10.3171/JNS/2008/108/6/1163
Lin N, Cahill KS, Frerichs KU, Friedlander RM, Claus EB (2012) Treatment of ruptured and unruptured cerebral aneurysms in the USA: a paradigm shift. J Neurointerv Surg 4(3):182–189. https://doi.org/10.1136/jnis.2011.004978
Li H, Pan R, Wang H et al (2013) Clipping versus coiling for ruptured intracranial aneurysms: a systematic review and meta-analysis. Stroke 44(1):29–37. https://doi.org/10.1161/STROKEAHA.112.663559
Ryu CW, Park S, Shin HS, Koh JS (2015) Complications in stent-assisted endovascular therapy of ruptured intracranial aneurysms and relevance to antiplatelet administration: a systematic review. Am J Neuroradiol 36(9):1682–1688. https://doi.org/10.3174/ajnr.A4365
Bechan RS, Sprengers ME, Majoie CB, Peluso JP, Sluzewski M, Van Rooij WJ (2016) Stent-assisted coil embolization of intracranial aneurysms: complications in acutely ruptured versus unruptured aneurysms. Am J Neuroradiol 37(3):502–507. https://doi.org/10.3174/ajnr.A4542
Zhao B, Tan X, Yang H et al (2017) Stent-assisted coiling versus coiling alone of poor-grade ruptured intracranial aneurysms: a multicenter study. J Neurointerv Surg 9(2):165–168. https://doi.org/10.1136/neurintsurg-2016-012259
Ding YH, Lewis DA, Kadirvel R, Dai D, Kallmes DF (2011) The Woven EndoBridge: a new aneurysm occlusion device. Am J Neuroradiol 32(3):607–611. https://doi.org/10.3174/ajnr.A2399
Pierot L, Liebig T, Sychra V et al (2012) Intrasaccular flow-disruption treatment of intracranial aneurysms: preliminary results of a multicenter clinical study. Am J Neuroradiol 33(7):1232–1238. https://doi.org/10.3174/ajnr.A3191
Woven EndoBridge (WEB) Aneurysm Embolization System P170032 FDA Approval. https://www.fda.gov/medical-devices/recently-approved-devices/woven-endobridge-web-aneurysm-embolization-system-p170032. Accessed August 23, 2020.
Lescher S, du Mesnil de Rochemont R, Berkefeld J (2016) Woven Endobridge (WEB) device for endovascular treatment of complex unruptured aneurysms—a single center experience. Neuroradiology 58(4):383–390. https://doi.org/10.1007/s00234-016-1641-x
Hunt WE, Hess RM (1968) Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg 28(1):14–20. https://doi.org/10.3171/jns.1968.28.1.0014
Frontera JA, Claassen J, Schmidt JM et al (2006) Prediction of symptomatic vasospasm after subarachnoid hemorrhage: the modified fisher scale. Neurosurgery 59(1):21–26. https://doi.org/10.1227/01.NEU.0000218821.34014.1B
Caroff J, Mihalea C, Tuilier T et al (2016) Occlusion assessment of intracranial aneurysms treated with the WEB device. Neuroradiology 58(9):887–891. https://doi.org/10.1007/s00234-016-1715-9
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339(7716):332–336. https://doi.org/10.1136/bmj.b2535
Howick J, Chalmers I, Glasziou P, et al. The Oxford 2011 Levels of Evidence. Oxford Centre Evidence-Based Medicine. Vol 1.; 2011. http://www.cebm.net/index.aspx?o=5653. Accessed September 23, 2020.
Caroff J, Mihalea C, Dargento F et al (2014) Woven Endobridge (WEB) Device for endovascular treatment of ruptured intracranial wide-neck aneurysms: a single-center experience. Neuroradiology 56(9):755–761. https://doi.org/10.1007/s00234-014-1390-7
Liebig T, Kabbasch C, Strasilla C et al (2015) Intrasaccular flow disruption in acutely ruptured aneurysms: a multicenter retrospective review of the use of the WEB. Am J Neuroradiol 36(9):1721–1727. https://doi.org/10.3174/ajnr.A4347
Van Rooij WJ, Peluso JP, Bechan RS, Sluzewski M (2016) WEB treatment of ruptured intracranial aneurysms. Am J Neuroradiol 37(9):1679–1683. https://doi.org/10.3174/ajnr.A4811
Popielski J, Berlis A, Weber W, Fischer S (2018) Two-center experience in the endovascular treatment of ruptured and unruptured intracranial aneurysms using the web device: a retrospective analysis. Am J Neuroradiol 39(1):111–117. https://doi.org/10.3174/ajnr.A5413
Da Ros V, Bozzi A, Comelli C et al (2019) Ruptured intracranial aneurysms treated with Woven Endobridge intrasaccular flow disruptor: a multicenter experience. World Neurosurg 122:e498–e505. https://doi.org/10.1016/j.wneu.2018.10.088
Raj R, Rautio R, Pekkola J, Rahi M, Sillanpää M, Numminen J (2019) Treatment of ruptured intracranial aneurysms using the Woven EndoBridge device: a two-center experience. World Neurosurg 123:e709–e716. https://doi.org/10.1016/j.wneu.2018.12.010
Youssef PP, Dornbos D, Peterson J et al (2020) Woven EndoBridge (WEB) device in the treatment of ruptured aneurysms. J Neurointerv Surg. https://doi.org/10.1136/neurintsurg-2020-016405
van Rooij SBT, Sprengers ME, Peluso JP, et al. A systematic review and meta-analysis of Woven EndoBridge single layer for treatment of intracranial aneurysms. Interv Neuroradiol. 2020;26(4). https://doi.org/10.1177/1591019920904421
Tau N, Sadeh-Gonik U, Aulagner G, Turjman F, Gory B, Armoiry X (2018) The Woven EndoBridge (WEB) for endovascular therapy of intracranial aneurysms: update of a systematic review with meta-analysis. Clin Neurol Neurosurg 166:110–115. https://doi.org/10.1016/j.clineuro.2018.01.025
Asnafi S, Rouchaud A, Pierot L, Brinjikji W, Murad MH, Kallmes DF (2016) Efficacy and safety of the woven endobridge (web) device for the treatment of intracranial aneurysms: a systematic review and meta-analysis. Am J Neuroradiol 37(12):2287–2292. https://doi.org/10.3174/ajnr.A4900
Sluzewski M, Van Rooij WJ. Early rebleeding after coiling of ruptured cerebral aneurysms: Incidence, morbidity, and risk factors. Am J Neuroradiol. 2005;26(7):1739–1743. https://pubmed.ncbi.nlm.nih.gov/16091523/. Accessed August 23, 2020.
Lindgren A, Vergouwen M Di, van der Schaaf I, et al. Endovascular coiling versus neurosurgical clipping for people with aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev. 2018;2018(8). https://doi.org/10.1002/14651858.CD003085.pub3
Johnston SC (2006) Rates of delayed rebleeding from intracranial aneurysms are low after surgical and endovascular treatment. Stroke 37(6):1437–1442. https://doi.org/10.1161/01.STR.0000221331.01830.ce
Renowden SA, Koumellis P, Benes V, Mukonoweshuro W, Molyneux AJ, McConachie NS (2008) Retreatment of previously embolized cerebral aneurysms: the risk of further coil embolization does not negate the advantage of the initial embolization. Am J Neuroradiol 29(7):1401–1404. https://doi.org/10.3174/ajnr.A1098
Molyneux AJ, Kerr RS, Yu LM et al (2005) International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and. Lancet 366(9488):809–817. https://doi.org/10.1016/S0140-6736(05)67214-5
Ahmed SI, Javed G, Bareeqa SB, et al. Endovascular coiling versus neurosurgical clipping for aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. Cureus. 2019;11(3). https://doi.org/10.7759/cureus.4320
Van Rooij WJ, Sluzewski M, Beute GN, Nijssen PC (2006) Procedural complications of coiling of ruptured intracranial aneurysms: incidence and risk factors in a consecutive series of 681 patients. Am J Neuroradiol 27(7):1498–1501
Kabbasch C, Goertz L, Siebert E et al (2019) Comparison of WEB embolization and coiling in unruptured intracranial aneurysms: safety and efficacy based on a propensity score analysis. World Neurosurg 126:e937–e943. https://doi.org/10.1016/j.wneu.2019.03.016
Funding
RWR was supported by National Institute of Health [NIH-NINDS R25NS065743].
Author information
Authors and Affiliations
Contributions
Conception and design: Alotaibi; acquisition of data: Alotaibi, Harker; analysis and interpretation of data: all authors; drafting the article: Harker, Alotaibi, Regenhardt; critically revising the article: all authors; reviewed submitted version of manuscript: all authors; approved the final version of the manuscript on behalf of all authors: Harker; statistical analysis: Alotaibi; and study supervision: Patel.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
AB Patel: Consultant for Penumbra, MicroVention, and Medtronic. B Pabon: Consultant for MicroVention. The remaining authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 150 KB)
Rights and permissions
About this article
Cite this article
Harker, P., Regenhardt, R.W., Alotaibi, N.M. et al. The Woven EndoBridge device for ruptured intracranial aneurysms: international multicenter experience and updated meta-analysis. Neuroradiology 63, 1891–1899 (2021). https://doi.org/10.1007/s00234-021-02727-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-021-02727-6