Abstract
Purpose
The Woven EndoBridge (WEB) device has been proven to be a safe and efficient endovascular treatment option for wide-necked bifurcation aneurysms. The study aimed to evaluate the incidence and risk factors of procedural complications related to WEB embolization of ruptured and unruptured intracranial aneurysms.
Methods
This was a multicenter, observational study of consecutive patients with ruptured and unruptured aneurysms who were treated with the WEB at three German tertiary care centers between May 2011 and February 2018. Patient characteristics, anatomical details and procedural aspects were retrospectively collected and the impact on procedure-related complications was evaluated.
Results
Among 120 patients (mean age 58.5 ± 11.9 years) with 120 aneurysms (mean size: 8.5 ± 4.5 mm), WEB implantation was successful in 112 patients (93.3%). The rates for overall and symptomatic complications were 11.7% and 5.0%, respectively. At 6‑month follow-up device-related morbidity was 1.2% among unruptured aneurysms and 2.6% among ruptured aneurysms. In the univariate analysis, a lower aspect ratio (p = 0.04) and an increased width-to-height ratio (p = 0.03) were significant risk factors for procedural complications.
Conclusion
The results of this study confirmed the WEB to be a safe treatment option, which is associated with low complication rates and minimal morbidity. Complications tended to occur more often in aneurysms with an unfavorable ratio between aneurysm height and aneurysm/neck width.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intrasaccular flow disruption represents a new paradigm for endovascular treatment of intracranial aneurysms, in particular for wide-necked and bifurcation aneurysms, which are typically challenging to treat by conventional endovascular means [21]. The Woven EndoBridge (WEB; Sequent Medical, Aliso Viejo, CA, USA) is a novel intrasaccular device, which is placed within the aneurysm cavity causing subsequent thrombosis of the aneurysm sac [6]. In contrast to intraluminal devices, such as stents and flow-diverters, the WEB leaves the parent artery unaffected, and does not necessarily require long-term antiplatelet therapy. These features make the WEB a suitable treatment option for both ruptured and unruptured aneurysms [5, 16].
Since its introduction in 2011, the safety profile of the WEB has been confirmed by several good clinical practice studies, in particular considering the complex subgroup of wide-necked aneurysms that are typically treated by this device. The overall periprocedural complication rate was 17.6% in the WEB Clinical Assessment of Intrasaccular Aneurysm Therapy (WEBCAST) trial, 18.2% in the WEBCAST 2 study, and 17.7% in the French Observatory study [19, 20, 22]. In the WEB Intra-saccular Therapy Study (WEB-IT), symptomatic complications were reported in 9.4% [8]. The majority of complications remained asymptomatic and device-related morbidity occurred in around 2% of patients [15, 17, 21]. Knowledge of risk factors for procedural complications may further increase the safety of this technique; however, a systematic risk factor analysis has not yet been available.
The objective of this multicenter study was to analyze the incidence and clinical relevance of complications related to WEB treatment. Univariate and bivariate logistic regression analyses were performed to identify independent risk factors for procedural complications.
Methods
This was a retrospective, observational study of consecutive patients that were treated with the WEB device at three German high-volume neurovascular centers between May 2011 and February 2018. Patients with successful and failed WEB implantation were both included in this study. Patients with multiple aneurysms treated with the WEB device during a single session were excluded from analysis. Some of the data were previously reported in three articles that focused on partially thrombosed aneurysms, retreatment strategies after WEB implantation, and risk factors of aneurysm recurrence, respectively [10, 11, 13]. According to the institutional guidelines, an ethics committee approval was not required for this retrospective, observational study.
Data Collection
The following data were recorded from the patient charts: age, gender, ruptured/unruptured aneurysm status, previous aneurysm treatment, aneurysm location, treatment success and use of additional devices and WEB type.
Conventional four-vessel digital subtraction angiography (DSA) and three-dimensional reconstructions of rotational angiography datasets were used to assess baseline aneurysm characteristics. The aneurysm size (largest diameter of the aneurysm sac), dome width, aneurysm height (H) and neck width (N) were measured for all aneurysms. Based on these parameters, the dome-to-neck (D/N) ratio, aspect ratio (H/N) and width-to-height (W/H) ratio were calculated. An aneurysm was defined as having a wide neck if the neck width was ≥4 mm and/or the D/N ratio was ≤2. The presence of partial intrasaccular aneurysm thrombosis was determined using magnetic resonance imaging (MRI), computed tomography angiography (CTA) or DSA. To assess aneurysm morphology, volume-rendered images of 3D rotational angiography datasets were reviewed independently by three senior consultant neuroradiologists (T.L., F.D. and C.K.). Lobular shape was defined as the presence of an additional aneurysm sac next to the main aneurysm sac [10]. Discrepancies were resolved in a consensus procedure.
WEB Treatment
All treatment indications were made within an interdisciplinary team consisting of neurointerventionalists and neurosurgeons and after discussion with the patient. At the centers, the WEB was typically used for wide-necked (neck width ≥4 mm and/or D/N ratio ≤2) and bifurcation aneurysms as an alternative treatment option for stent-assisted procedures or microsurgical clipping in aneurysms, which were not deemed suitable for conventional coiling. The WEB device is also used for poor grade subarachnoid hemorrhage (SAH) patients, which might have a realistic chance of recovery after correct endovascular treatment and intensive supportive neurocritical care [25].
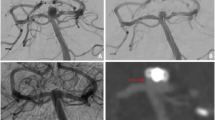
All procedures were performed with the patient under general anesthesia. The WEB device was delivered via a transfemoral approach using a triaxial access system and the dedicated VIA microcatheter in most cases (VIA 21, 27 or 33, Sequent Medical). In the present study, the following three WEB types were used: single-layer (SL), double-layer (DL), and single-layer sphere (SLS). To determine the appropriate WEB size, aneurysm width and height were measured on two-dimensional DSA images. Implant sizes were chosen to be slightly larger than the aneurysm equator diameter as recommended in the instructions for use (IFUs). The use of adjunctive endovascular techniques, such as stent implantation and coiling was left to the neurointerventionalist’s discretion and mainly depended on anatomical considerations. Where necessary, implantation of an additional stent was conducted in order to optimize intra-aneurysmal WEB positioning or to prevent potential WEB protrusion into the parent vessel. Adjunctive coiling may have been used for aneurysms with atypical configuration in order to provide adequate occlusion. On the first day after the procedure or in case of clinical deterioration, all initial SAH patients received a cranial CT scan to exclude rebleeding. After scheduled WEB embolization of an unruptured aneurysm, patients with new neurological deficits underwent MRI of the brain.
Anti-Aggregation Therapy
In elective cases a bolus of heparin (5000 IU) was administered after groin puncture, followed by aliquots of 1000 IU/h. Heparin was discontinued at the end of the procedure. For WEB implantation, all elective patients received acetylsalicylic acid (ASA) 100 mg/day starting 5–7 days before the procedure and ASA monotherapy was continued for a minimum of 4 weeks. In the case of additional stent implantation or flow-diversion, a daily dual antiplatelet regimen with ASA 100 mg and clopidogrel 75 mg was administered for at least 4 months after the intervention, starting 5–7 days before the procedure. Thereafter, ASA monotherapy was continued lifelong. Platelet inhibition was tested in all patients with ASA and accessorily P2Y12 assays where required (VerifyNow, Accumetrics, San Diego, CA, USA). A platelet inhibition level between 350–550 aspirin response units (ARU) and 30–90% for clopidogrel was postulated. An insufficient response to either drug was counteracted by dose escalation (e.g. clopidogrel 150 mg/day) or substitution with prasugrel (60 mg bolus, 10 mg/day). In cases of acute SAH and sole WEB treatment, no additional antiplatelet drugs were administered.
Complications and Clinical Outcome
Procedure-related complications were retrospectively obtained from the patient charts and the operation records. The focus was on periprocedural complications that occurred intraoperatively and in the early postinterventional period until discharge of the patient from hospital and the clinical outcome until 6‑month follow-up visit. Complications were classified as symptomatic or asymptomatic and both complication types are reported. Patients with symptomatic complications were defined to have new neurological deficits postoperatively that were either transient (deficits resolved until discharge) or persistent (neurological deficits at discharge).
According to the modified Rankin scale (mRS) score, clinical outcome was determined at baseline, at discharge from hospital and at 6‑month follow-up visit. A mRS score of 0–2 was categorized as favorable outcome and a score of 3–6 as unfavorable outcome. Device-related morbidity was defined as unfavorable outcome at 6‑month follow-up, which could be clearly ascribed to the WEB procedure.
Statistical Analysis
Categorical variables were expressed as numbers with percentages and compared using the χ2-test and Fisher’s Exact test, when appropriate. Continuous variables were presented as means ± standard deviation. Continuous variables were tested for normality using the Shapiro-Wilk test and then compared between the groups using the two-sided unpaired Student’s t‑test (for normally distributed data) and the Mann-Whitney U-test (for non-normally distributed data). Univariate analysis was performed to reveal parameters that correlate with the occurrence of complications. Predictive factors in the univariate analysis (p < 0.1) were entered into a binary logistic regression model to identify independent factors of complications. Receiver operating characteristic (ROC) curve analysis was performed to determine cut-off values. All calculations were performed using SPSS software (IBM SPSS Statistics for Windows, Version 25.0, Armonk, NY, USA). A p-value <0.05 was considered as statistically significant.
Results
Patient and Aneurysm Characteristics
A total of 121 patients with 122 aneurysms were treated with the WEB device within the study period. Of the patients one that underwent WEB embolization for two aneurysms in a single session was excluded from analysis. Hence, the final study population consisted of 120 patients with 120 aneurysms. The mean patient age was 58.5 ± 11.9 years, 80 patients (66.7%) were female and 38 patients (31.7%) presented with aneurysmal subarachnoid hemorrhage. Baseline patient characteristics are outlined in Table 1.
A total of 11 patients were treated with the WEB for a previously treated and recurrent aneurysm (9.2%), 7 aneurysms (5.8%) showed intrasaccular partial thrombus formation and 14 had a lobular shape (11.7%). The most common aneurysm locations were the basilar artery (32.5%), the anterior communicating artery (Acom, 29.2%) and the middle cerebral artery (MCA, 14.2%). The mean aneurysm size was 8.5 ± 4.5 mm and the mean neck width was 4.5 ± 1.7 mm. A total of 109 aneurysms (90.8%) were classified as wide-necked. Baseline aneurysm characteristics are presented in Table 2.
Procedural Details
A WEB implantation was technically successful in 112 procedures (93.3%) but implantation failed in 8 patients (6.7%) for the following reasons: 1) WEB implantation was not possible due to an unfavorable aneurysm angle (5 cases), 2) the WEB narrowed the parent artery after implantation and was therefore removed (2 cases), and 3) the WEB was removed due to a significant aneurysm remnant in a SAH patient. Among the successful procedures, 86 aneurysms were treated by WEB only (76.8%) and 26 aneurysms in combination with other endovascular techniques (23.2%). Overall, additional coiling was performed in 11 aneurysms (9.8%) and stents or flow-diverters were implanted in 19 (17.0%). Both adjunctive coiling and intracranial stents were used in 4 patients (3.6%). Procedural specifics are listed in Table 3.
Complications and Clinical Outcome
Overall, complications occurred in 14 of 120 procedures (11.7%). In 6 patients (5.0%) the complications were associated with new neurological deficits, which were transient in 4 (3.3%) and persistent in 2 (1.7%). The procedure-related mortality rate was 0.8% and 11 patients (9.2%) had thromboembolic complications. Intraprocedural thrombus formation occurred in 9 patients, whereby the thrombus could be resolved by administration of tirofiban in 7 patients and by mechanical thrombectomy in 1. Another patient with an anterior communicating artery aneurysm had a thrombotic occlusion of the pericallosal artery, which could not be resolved during the procedure. Among these patients a new ischemic lesion was observed in two patients, which remained asymptomatic. Symptomatic infarction occurred in 3 patients (2.5%). In these patients, thrombus formation could not be observed during the procedure but the patients showed new neurological deficits afterwards. Among the patients with symptomatic stroke, two could be discharged in good clinical condition (mRS ≤2), while the third patient was moderately disabled (mRS 3). At follow-up, all three patients were independent (mRS ≤1). Of the patients two had a hemorrhagic complication (1.7%). In the first patient an intraoperative aneurysm rupture occurred due to misplacement of the WEB and resulted in subarachnoid hemorrhage. The patient finally died from brain edema which was associated with subarachnoid hemorrhage. In the second patient a peri-interventional aneurysmal rupture of a complex, partially thrombosed aneurysm at the anterior communicating artery resulted in intraventricular hemorrhage. The patient developed a hemiparesis and was discharged with a mRS score of 5. There were two further complications that were not thromboembolic or hemorrhagic: one patient had a single seizure and was free of complaints thereafter. The second patient had mild postoperative brain swelling after the procedure, which was associated with a transient hemiparesis. Complications are listed in Table 4.
A total of 96 patients achieved favorable outcome at discharge (80.0%), 97.6% (80/82) in the non-SAH group and 42.1% (16/38) in the SAH group. At 6‑month follow-up, favorable outcome was achieved in 100 patients (83.3%), 97.6% (80/82) in the non-SAH group and 52.6% (20/38) in the SAH group. In the SAH group, favorable outcome was achieved by 70.6% (12/17) of patients with a World Federation of Neurosurgical Societies score of (WFNS) 1–2 and by 38.1% (8/21) of patients with WFNS 3–5 (p = 0.046). Device-related morbidity at 6‑month follow-up was 1.2% (1/82) in the non-SAH group and 2.6% (1/38) in the SAH group. In both cases, device-related morbidity was related to a hemorrhagic complications. The clinical outcomes are shown in Table 5.
Risk Factors for Complications
The following variables were tested as risk factors for periprocedural complications in the univariate analysis (Table 6): patient age, gender, aneurysm location, aneurysm size indices, ruptured/unruptured aneurysm status, previous aneurysm treatment, aneurysm shape, intrasaccular partial thrombus formation, use of additional devices and WEB type. In two patients with intraoperative adverse events (aneurysm perforation and occlusion of the parent artery), additional stents were implanted to treat the respective complication. Hence, these cases were categorized as “WEB only” for the statistical analysis of risk factors.
In the univariate analysis, complications occurred significantly more often in patients with a lower aspect ratio (1.6 ± 1.2 vs. 1.9 ± 1.0, p = 0.04; AUC = 0.333) and an increased W/H ratio (1.2 ± 0.3 vs. 1.0 ± 0.3, p = 0.03; AUC = 0.676). These variables were dependent in the multivariate analysis (aspect ratio p = 0.9, W/H ratio: p = 0.13). The other tested factors were not significantly associated with procedural complications in the univariate analysis.
Discussion
In the current study consecutive patients were analyzed that differed in terms of aneurysm location, aneurysm size, aneurysm status and treatment modality. Hence, complications rates of WEB implantation in a real-world setting are reported. Procedure-related complications occurred during 14 of 120 WEB procedures, representing an overall complication rate of 11.7%. This rate is comparable to previous retrospective studies on WEB embolization. For instance, complications occurred in 11.7% in the study by Behme et al. [1] and 15.4% in the study by Clajus et al. [5]. The most common adverse events related to WEB implantation are thromboembolic complications, accounting for 14.4% in the study by Pierot et al. [21], 10.0% in the study by Clajus et al. [5] and 11.8% in the study by Papagiannaki et al. [18].
In the present study, thromboembolic events occurred in 11 patients (9.2%), whereby 3 patients had transient neurological deficits (2.5%). In 8 cases, thrombus formation was observed during the procedure and could be resolved by anti-platelet therapy or mechanical thrombectomy. In one patient, the thrombus could not be resolved and resulted in cerebral infarction; however, none of the patients with intraprocedural thrombus formation were symptomatic after the procedure. Radiological proof of a new ischemic lesion was found in 5 patients (4.2%). Of these, three patients had new neurological deficits after the procedure but these were transient in all cases and the patients were free of symptoms at mid-term follow-up.
Overall, a favorable outcome was achieved in 97.6% of patients with unruptured aneurysms and 52.6% in patients with ruptured aneurysms. Device-related morbidity was 1.2% among elective cases and 2.6% in the SAH group. Similarly, morbidity was reported in 1.2% by Pierot et al. [21], 0% by Behme et al. [1], and 1.3% by Papagiannaki et al. [18]. These data collectively confirm the high safety profile of the WEB, especially considering the complex subset of aneurysms which is typically treated by the WEB.
Executing WEB procedures has a learning curve and initial proctoring is eligible since correct WEB sizing is crucial. Knowledge of risk factors for complications is essential for risk stratification and to further increase the safety of the WEB procedure. Known risk factors for procedural complications related to endovascular treatment include aneurysm location, ruptured aneurysm status, and use of stents [2,3,4, 23]. In the current study, complication rates were similar among ruptured (13.2%) and unruptured aneurysms (11.7%). Moreover, at least in this setting with a moderate sample size, a significant correlation between aneurysm location, maximum aneurysm diameter and procedural complications related to WEB treatment could not be established. Likewise, complications were not significantly increased in morphologically complex aneurysms, such as partially thrombosed aneurysms, lobulated aneurysms and large aneurysms. In these complex aneurysms, the WEB is generally used as part of a multimodal treatment approach in combination with stents and/or adjunctive coiling, since the diameter of these aneurysms typically exceeds the size of the largest available WEB (11 mm). Given that these types of aneurysms do not represent the primary indication for WEB implantation according to the device’s instructions for use (IFU), these aneurysms are otherwise also exceptionally challenging to treat by either endovascular or surgical methods and independent of the treatment strategy, which might be associated with increased complication rates and morbidity [7, 9, 13, 14]. Moreover, previous research has indicated that implantation of adjunctive intraluminal devices can be associated with increased rates of thromboembolic events when compared to stand-alone coiling [23]. For instance, Piotin et al. reported neurological complications in 7.4% after stent-assisted coiling compared to 3.8% after stand-alone coiling [23]. This difference was further associated with an increased procedure-related mortality rate among patients treated by stent-assisted coiling (4.6% vs. 1.2%) [23]. In a comparative study, we recently reported procedural complications in 21.2% after stent-assisted coiling, compared to 12.1% after WEB treatment [12]. In the majority of studies on the WEB procedure, additional stents were used to a varying extent [13, 16, 21]. In contrast, van Rooij et al. recently published a study in which they reported their experience in using the WEB as primary treatment option for patients with unruptured intracranial aneurysms [24]. Among 59 aneurysms, 55 were treated by WEB only and 4 with additional coiling. Additional stents were not used in any case. The authors reported a complication rate of 2.0%, which is considerably lower than that of the studies cited here. These results imply that complication rates may be more favorable in non-complex aneurysms treated by WEB only. Likewise, in the present study, patients treated by WEB only had a lower complication rate (10%) than patients intentionally treated in conjunction with stents and/or coiling (21%); however, this difference failed to reach statistical significance (p = 0.16), which may be attributed to a lack of statistical power.
In the present study, an increased W/H ratio and a lower aspect ratio were significantly associated with procedural complications, whereas the other aneurysm size indices, such as maximum aneurysm diameter, neck width and D/N ratio did not significantly correlate with the complication rate. In particular, complications occurred more often among aneurysms with a W/H ratio >1.1 (area under the curve, AUC = 0.676), meaning that the dome width was larger than the aneurysm height. Since large-scale studies could not confirm aneurysm size as an independent risk factor for procedural complications related to endovascular treatment [3, 4, 23], the results of this analysis need to be validated by further series.
In conclusion, the results of this study indicate that procedural complications may correlate with aneurysm size (W/H ratio, aspect ratio); however, in the multivariate analysis, an independent risk factor for procedure-related complications could not be identified. This might be, at least in part, related to the limited sample size of the study and to a lack of statistical power. It might be probable that large-scale studies will produce different results; however, the occurrence of complications in a real-world setting is described confirming the high safety profile of the WEB.
Limitations
The limitations of this study are mainly related to its retrospective design. The aneurysms were heterogeneous in size and configuration and different treatment methods were used for aneurysm embolization. Although a multicenter analysis was conducted, the sample size was only moderate. Due to these limitations, further studies with a larger patient sample will be required to draw a definite conclusion. Nevertheless, it is believe that this study provides valuable insights into the occurrence of complications related to WEB embolization.
Conclusion
In the current study the high safety profile of the WEB device, could be confirmed. The WEB embolization was associated with low complication and morbidity rates, which were independent of aneurysm size, location, and ruptured status. Also, the intentional use of adjunctive techniques did not have a significant impact on the complication rate; however, complications tended to occur more often in aneurysms with an unfavorable ratio between aneurysm height and aneurysm/neck width. Further studies will be necessary to confirm the results.
References
Behme D, Berlis A, Weber W. Woven EndoBridge intrasaccular flow disrupter for the treatment of ruptured and unruptured wide-neck cerebral aneurysms: report of 55 cases. AJNR Am J Neuroradiol. 2015;36:1501–6.
Borggrefe J, Behme D, Mpotsaris A, Weber W. Complications associated with cerebral aneurysm morphology in balloon-assisted coil embolization of ruptured and unruptured aneurysms—a single-center analysis of 116 consecutive cases. World Neurosurg. 2016;91:483–9.
Chalouhi N, Jabbour P, Singhal S, Drueding R, Starke RM, Dalyai RT, Tjoumakaris S, Gonzalez LF, Dumont AS, Rosenwasser R, Randazzo CG. Stent-assisted coiling of intracranial aneurysms: predictors of complications, recanalization, and outcome in 508 cases. Stroke. 2013;44:1348–53.
Chalouhi N, Tjoumakaris S, Gonzalez LF, Dumont AS, Starke RM, Hasan D, Wu C, Singhal S, Moukarzel LA, Rosenwasser R, Jabbour P. Coiling of large and giant aneurysms: complications and long-term results of 334 cases. AJNR Am J Neuroradiol. 2014;35:546–52.
Clajus C, Strasilla C, Fiebig T, Sychra V, Fiorella D, Klisch J. Initial and mid-term results from 108 consecutive patients with cerebral aneurysms treated with the WEB device. J Neurointerv Surg. 2017;9:411–7.
Ding YH, Lewis DA, Kadirvel R, Dai D, Kallmes DF. The Woven EndoBridge: a new aneurysm occlusion device. AJNR Am J Neuroradiol. 2011;32:607–11.
Ferns SP, van Rooij WJ, Sluzewski M, van den Berg R, Majoie CB. Partially thrombosed intracranial aneurysms presenting with mass effect: long-term clinical and imaging follow-up after endovascular treatment. AJNR Am J Neuroradiol. 2010;31:1197–205.
Fiorella D, Molyneux A, Coon A, Szikora I, Saatci I, Baltacioglu F, Sultan A, Arthur A; WEB-IT Study Investigators. Demographic, procedural and 30-day safety results from the WEB Intra-saccular Therapy Study (WEB-IT). J Neurointerv Surg. 2017;9:1191–6.
Goertz L, Kasuya H, Hamisch C, Kabbasch C, von Spreckelsen N, Ludyga D, Timmer M, Stavrinou P, Goldbrunner R, Brinker G, Krischek B. Impact of aneurysm shape on morbidity after clipping of unruptured intracranial aneurysms. Acta Neurochir (Wien). 2018;160:2169-76.
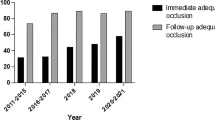
Kabbasch C, Goertz L, Siebert E, Herzberg M, Borggrefe J, Dorn F, Liebig T. Factors that determine aneurysm occlusion after embolization with the Woven EndoBridge (WEB). J Neurointerv Surg. 2018 Oct 24. doi: 10.1136/neurintsurg-2018-014361. [Epub ahead of print]
Kabbasch C, Goertz L, Siebert E, Herzberg M, Hamisch C, Mpotsaris A, Dorn F, Liebig T. Treatment strategies for recurrent and residual aneurysms after Woven Endobridge implantation. J Neurointerv Surg. 2018 Aug 28. doi: 10.1136/neurintsurg-2018-014230. [Epub ahead of print]
Kabbasch C, Goertz L, Siebert E, Herzberg M, Borggrefe J, Krischek B, Stavrinou P, Dorn F, Liebig T. WEB embolization versus stent-assisted coiling: comparison of complication rates and angiographic outcomes. J Neurointerv Surg. 2018; https://doi.org/10.1136/neurintsurg-2018-014555
Kabbasch C, Mpotsaris A, Reiner M, Liebig T. WEB as part of a multimodality treatment in complex, large, and partially thrombosed intracranial aneurysms: a single-center observational study of technical success, safety, and recurrence. J Neurointerv Surg. 2016;8:1235–9.
Kim SJ, Choi IS. Midterm outcome of partially thrombosed intracranial aneurysms treated with Guglielmi detachable coils. Interv Neuroradiol. 2000;6:13–25.
Lawson A, Molyneux A, Sellar R, Lamin S, Thomas A, Gholkar A, Patankar T. Safety results from the treatment of 109 cerebral aneurysms using the Woven EndoBridge technique: preliminary results in the United Kingdom. J Neurosurg. 2018;128:144–53.
Liebig T, Kabbasch C, Strasilla C, Berlis A, Weber W, Pierot L, Patankar T, Barreau X, Dervin J, Kuršumović A, Rath S, Lubicz B, Klisch J. Intrasaccular flow disruption in acutely ruptured aneurysms: a multicenter retrospective review of the use of the WEB. AJNR Am J Neuroradiol. 2015;36:1721–7.
Lv X, Zhang Y, Jiang W. Systematic review of Woven EndoBridge for wide-necked bifurcation aneurysms: complications, adequate occlusion rate, morbidity, and mortality. World Neurosurg. 2018;110:20–5.
Papagiannaki C, Spelle L, Januel AC, Benaissa A, Gauvrit JY, Costalat V, Desal H, Turjman F, Velasco S, Barreau X, Courtheoux P, Cognard C, Herbreteau D, Moret J, Pierot L. WEB intrasaccular flow disruptor—prospective, multicenter experience in 83 patients with 85 aneurysms. AJNR Am J Neuroradiol. 2014;35:2106–11.
Pierot L, Costalat V, Moret J, Szikora I, Klisch J, Herbreteau D, Holtmannspötter M, Weber W, Januel AC, Liebig T, Sychra V, Strasilla C, Cognard C, Bonafé A, Molyneux A, Byrne JV, Spelle L. Safety and efficacy of aneurysm treatment with WEB: results of the WEBCAST study. J Neurosurg. 2016;124:1250–6.
Pierot L, Gubucz I, Buhk JH, Holtmannspötter M, Herbreteau D, Stockx L, Spelle L, Berkefeld J, Januel AC, Molyneux A, Byrne JV, Fiehler J, Szikora I, Barreau X. Safety and efficacy of aneurysm treatment with the WEB: results of the WEBCAST 2 study. AJNR Am J Neuroradiol. 2017;38:1151-5.
Pierot L, Moret J, Barreau X, Szikora I, Herbreteau D, Turjman F, Holtmannspotter M, Januel AC, Costalat V, Fiehler J, Klisch J, Gauvrit JY, Weber W, Desal H, Velasco S, Liebig T, Stockx L, Berkefeld J, Molyneux A, Byrne J, Spelle L. Safety and efficacy of aneurysm treatment with WEB in the cumulative population of three prospective, multicenter series. J Neurointerv Surg. 2018;10:553–9.
Pierot L, Moret J, Turjman F, Herbreteau D, Raoult H, Barreau X, Velasco S, Desal H, Januel AC, Courtheoux P, Gauvrit JY, Cognard C, Soize S, Molyneux A, Spelle L. WEB treatment of intracranial aneurysms: feasibility, complications, and 1‑month safety results with the WEB DL and WEB SL/SLS in the French observatory. AJNR Am J Neuroradiol. 2015;36:922–7.
Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ, Moret J. Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke. 2010;41:110–5.
van Rooij SB, van Rooij WJ, Peluso JP, Sluzewski M. The Woven EndoBridge (WEB) as primary treatment for unruptured intracranial aneurysms. Interv Neuroradiol. 2018;24(5):475–81.
Taylor CJ, Robertson F, Brealey D, O’shea F, Stephen T, Brew S, Grieve JP, Smith M, Appleby I. Outcome in poor grade subarachnoid hemorrhage patients treated with acute endovascular coiling of aneurysms and aggressive intensive care. Neurocrit Care. 2011;14:341–7.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
L. Goertz, E. Siebert, M. Herzberg, H. Neuschmelting, J. Borggrefe, Ö.A. Onur declare that they have no competing interests. T. Liebig serves as proctor for MicroVention Inc./Sequent Medical (Aliso Viejo, CA, USA). F. Dorn and C. Kabbasch serve as consultants for Acandis GmbH (Pforzheim, Germany).
Ethical standards
All procedures reported in this article were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. According to institutional guidelines, no ethics committee approval was required for this retrospective observational study. The manuscript does not contain any details that might disclose the identity of the patients.
Additional information
L. Goertz and T. Liebig contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Goertz, L., Liebig, T., Siebert, E. et al. Risk Factors of Procedural Complications Related to Woven EndoBridge (WEB) Embolization of Intracranial Aneurysms. Clin Neuroradiol 30, 297–304 (2020). https://doi.org/10.1007/s00062-019-00762-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-019-00762-8